INTRODUCTION
A tracheostomy is a common procedure done for patients who need prolonged mechanical ventilation, are unable to protect their airway or have pathologies of the oropharynx leading to the potential for upper airway obstruction. While a tracheostomy is relatively safe, complications are common, and it is essential to understand the management steps to ensure that the patient’s tracheostomy functions as intended.1
In a single center study of 100 patients undergoing tracheostomy, the complication rate was 47% during the initial hospitalization. The most common complications included obstruction of the tracheostomy (19%), bleeding (16%), infection (14%), and accidental decannulation (13%).2 While these complications are common, if managed appropriately, mortality directly related to the tracheostomy has a very low incidence.3,4
MANAGEMENT STEPS OF A POTENTIALLY MALFUNCTIONING TRACHEOSTOMY
In the setting of an occluded or accidentally decannulated tracheostomy, one would expect high airway pressures or loss of tidal volumes if the patient is being mechanically ventilated, and potentially a loss of end-tidal carbon dioxide. If there is concern for either of these complications, the following interventions should be taken to determine the cause of the potential malfunctioning of the tracheostomy tube.
First, the anesthesia professional should deflate the tracheostomy cuff to allow spontaneous breathing, if possible. At the same time, it is important to gain more information about the tracheostomy, including how long ago was it placed, the indication for placement, and the type of tracheostomy (surgical vs. percutaneous). One also needs to determine whether the patient has a patent upper airway allowing for mask ventilation and intubation and the potential for difficult oral intubation, if necessary. If the patient is breathing spontaneously around the deflated cuff, the anesthesia professional should place an oxygen mask on the patient’s mouth and tracheostomy stoma since the patient could potentially be breathing through either location. If available, waveform capnography should be used to assist in determining which site, if any, the patient is able to breathe through.5
To exclude the possibility of an occluded tracheostomy tube, the anesthesia professional should remove the inner cannula (if present) (Figure 1). The inner cannula is designed to be easily removable to allow cleaning of mucous and other material which can occlude the tracheostomy tube. If ventilation still remains inadequate, the anesthesia professional can then advance a suction catheter through the tracheostomy tube into the distal trachea. If the suction catheter does not advance beyond the end of the tracheostomy, the tip of the tracheostomy may be pressed up against the tracheal wall or occluded by an overinflated cuff.

Figure 1: Middle—cuffed tracheostomy, left—obturator to assist with insertion of tracheostomy, right—removable inner cannula.
If the suction catheter does not advance beyond the tip of the tracheostomy, the tracheostomy may have become displaced from the trachea and positioned in the subcutaneous tissue in the neck.6 To determine the cause of the inadequate ventilation, the anesthesia professional can attempt to gently provide positive pressure ventilation via a bag-valve-mask. If end-tidal CO2 is not present and/or high airway pressures are experienced, attempts to provide positive pressure ventilation must immediately be stopped and it should be assumed that the tracheostomy tube is no longer in the trachea. If available, a bronchoscopy scope can be advanced down the tracheostomy tube to confirm that it is no longer in the trachea.7 Attempts to provide positive pressure ventilation with a dislodged tracheostomy that is located in the subcutaneous tissue can lead to complications including subcutaneous emphysema, pneumothoraces, and pneumomediastinum. In addition, the pressurized air can track into the subcutaneous tissues of the upper airway making intubation difficult. (Figure 2).
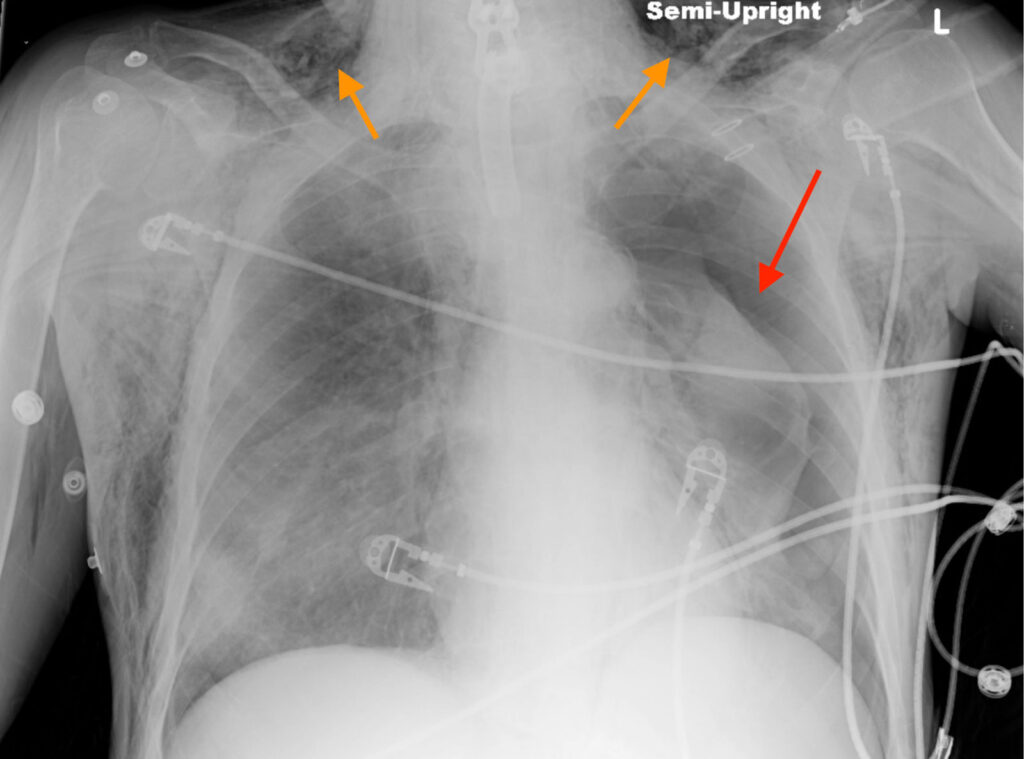
Figure 2: Chest x-ray from a patient with a malpositioned tracheostomy tube who received positive pressure ventilation, leading to a left-sided pneumothorax (red arrow) and subcutaneous emphysema (orange arrows) in the neck.
If there is concern that the tracheostomy is in the subcutaneous tissue and the patient is not ventilating adequately, the tracheostomy must be removed. Once the tracheostomy tube has been removed, assess the patient’s ventilation both orally and through the tracheostomy stoma; if adequate, wait for additional help to arrive. If ventilation remains inadequate and the patient is desaturating, the anesthesia professional should attempt to mask ventilate the patient either orally while occluding the stoma or via the tracheostomy stoma itself.8 A pediatric mask may be helpful in ventilating via the stoma.
If mask ventilation is inadequate, the patient will need to be urgently intubated orally or via the tracheostomy stoma. The decision of oral vs. via stoma will be influenced by the presence of a patent upper airway, the expected difficulty of oral intubation, experience of the providers present, and the age of the tracheostomy. Factors that would support attempting oral intubation include providers inexperienced in replacing tracheostomies, history of easy oral intubation, no oropharyngeal pathology present, or if it is a “new” tracheostomy (surgical tracheostomy <4 days, percutaneous tracheostomy <7–10 days).9 With a “fresh” tracheostomy stoma there is a risk of inadvertently advancing the tube into the subcutaneous tissue. A surgical tracheostomy is considered “mature” earlier because the surgical tracheostomy typically has a portion of the trachea that is sutured to the skin which decreases the risk of advancing a tube into the subcutaneous tissue. Factors that would support intubating the tracheostomy stoma as opposed to intubation orally include the provider’s comfort in replacing a tracheostomy, a history of difficult intubation or known oropharyngeal pathology that will make oral intubation difficult, or a “mature” tracheostomy with a well-healed stoma.6
If the stoma is “mature” with a moderate sized opening and a clear path to the trachea, a tracheostomy tube can simply be advanced back into the trachea. If the stoma is small or difficulty is expected, an endotracheal tube is recommended since it may be less likely to advance into a false passage.5 An intubation bougie can be placed into the stoma first and used to feel for the tracheal rings in a fashion similar to oral intubation. Alternatively, a bronchoscopy scope can be advanced into the stoma first while attempting to identify the trachea. Then a bougie or bronchoscopy scope can be used to facilitate advancing the endotracheal tube into the trachea.10
To improve the safety for patients with a tracheostomy, it is recommended to have bedside signs and algorithm sheets readily available for reference to facilitate the management of these patients (Figures 3 and 4).11
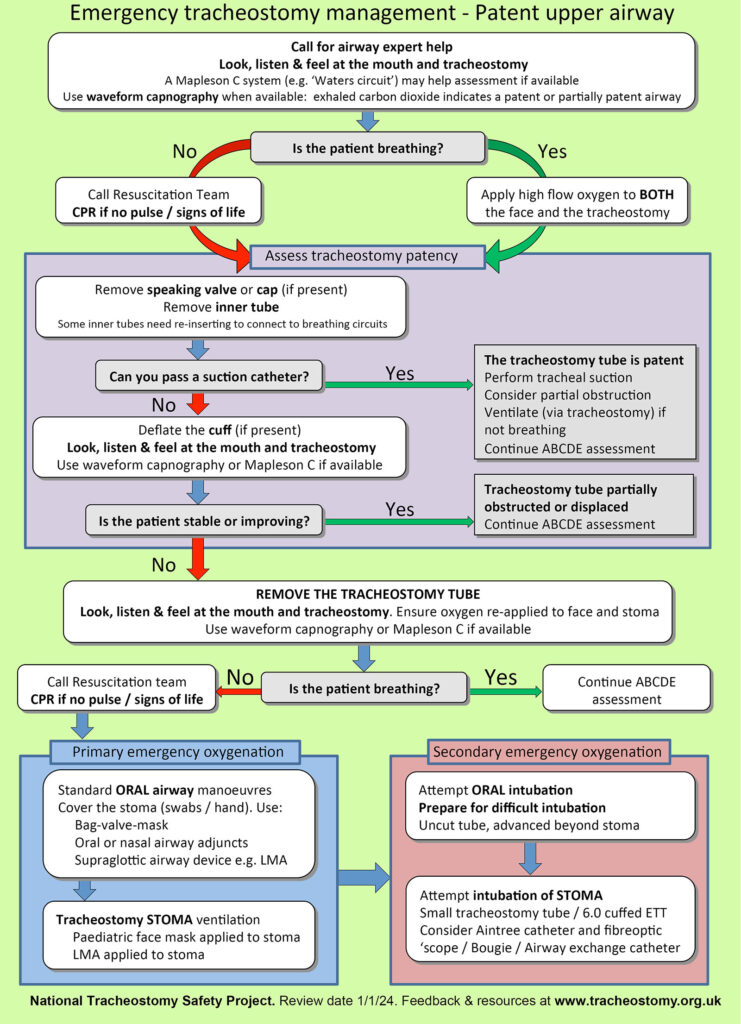
Figure 3: Emergency tracheostomy management algorithm. Used with permission from Brendan McGrath and the National Tracheostomy Safety Project.
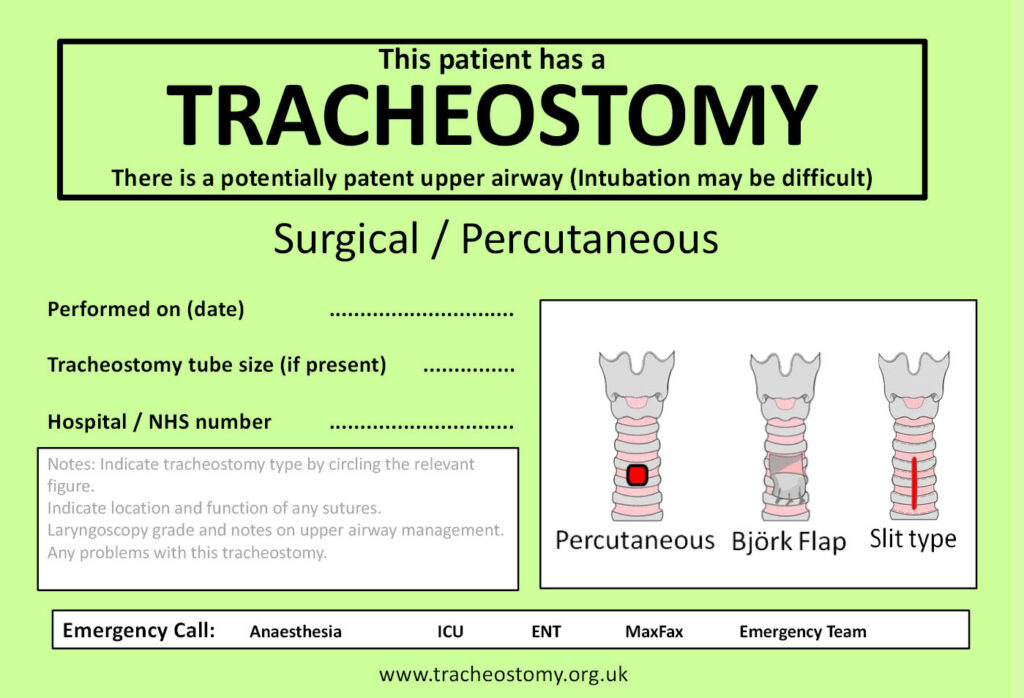
Figure 4: Tracheostomy bedside sign. Used with permission from Brendan McGrath and the National Tracheostomy Safety Project.
PATIENTS PRESENTING TO THE OPERATING ROOM WITH A TRACHEOSTOMY IN PLACE
For the patient presenting to the operating room with an existing tracheostomy, there are multiple considerations for management.12 The first priority is obtaining a “tracheostomy history” (including whether there is a patent upper airway, maturity of trach, etc). Next assessment of the ventilation needs during the procedure is required. The simplest situation is a cuffed tracheostomy that will not be in the surgical field, which can be used without any modifications. If the tracheostomy is uncuffed, it could potentially be used if the patient will be spontaneously breathing and positive pressure ventilation is not indicated. The decision is determined by the need for positive pressure ventilation during the procedure. If the tracheostomy tube will be in the surgical field, it may need to be replaced with an endotracheal tube that is placed either orally or via the tracheostomy stoma.
If the tracheostomy tube needs to be exchanged, the factors described previously in this article can be used to influence the decision as to whether to intubate the patient orally or use the stoma in the neck. For oral intubation, the cuff of the endotracheal tube should be placed just beyond the stoma site to allow a seal to be created with the trachea. If the stoma site is to be used, a wire-reinforced endotracheal tube may be selected to minimize the risk of kinking. The tracheal stoma site is typically placed between the 2nd–4th tracheal ring. The distance from the stoma to the carina is approximately 6.5 cm so caution must be used to ensure that the endotracheal tube does not enter the mainstem bronchus.13 Ausculation of bilateral breath sounds after endotracheal tube insertion confirms proper position and facilitates adjustment if needed
If there is a concern for difficult placement of the endotracheal tube into the stoma such as with a fresh stoma, an airway exchange catheter can be used to facilitate the exchange of a tracheostomy tube.14 The exchange catheter can minimize the risk of placing the endotracheal tube into a false passage in the subcutaneous tissue. Some brands of tube exchangers have an open channel which allows the insufflation of oxygen during the exchange to minimize desaturation.
SPECIAL CONSIDERATIONS: LARYNGECTOMY PATIENTS
Patients with a total laryngectomy or “neck breathers” require special considerations. In these patients, the larynx is surgically removed, and the trachea is sutured to the skin of the anterior neck. The end result is the trachea no longer communicates with the oropharynx so the patients cannot be orally intubated or mask ventilated. This is a significant safety risk for these patients if respiratory distress occurs. A survey of otolaryngologists demonstrated that over half of these clinicians had experienced a situation where health care providers attempted to orally intubate or mask ventilate patients with a total laryngectomy. When this occurred, the reported mortality rate was 26%.15
To minimize the risk of harm for patients with laryngectomies, they must be distinguished from patients with a patent upper airway. One method to do this is with a bedside sign specific for laryngectomy patients (Figure 5) and placing an alert in the patient’s chart.16 If a patient with a total laryngectomy experiences respiratory distress, an oxygen mask should be applied to the stoma site. If mask ventilation is indicated, a pediatric mask can be placed over the stoma and ventilation provided. Most patients with a total laryngectomy do not have a cuffed tracheostomy tube in place. If the patient needs positive pressure ventilation, a cuffed tracheostomy tube can be exchanged for the uncuffed tracheostomy tube or an appropriately sized endotracheal tube can be inserted into the stoma in the neck. The tube should advance easily into the trachea since these patients typically have a reasonably sized stoma. It should be noted that during laryngectomy the trachea is sutured to the skin, so it is more difficult for a clinician to advance the endotracheal tube into a false passage even after the sutures have been removed.17 It can be helpful to have algorithms for laryngectomy management at the bedside in a fashion similar to patient’s with tracheostomies for easy reference (Figure 6).16
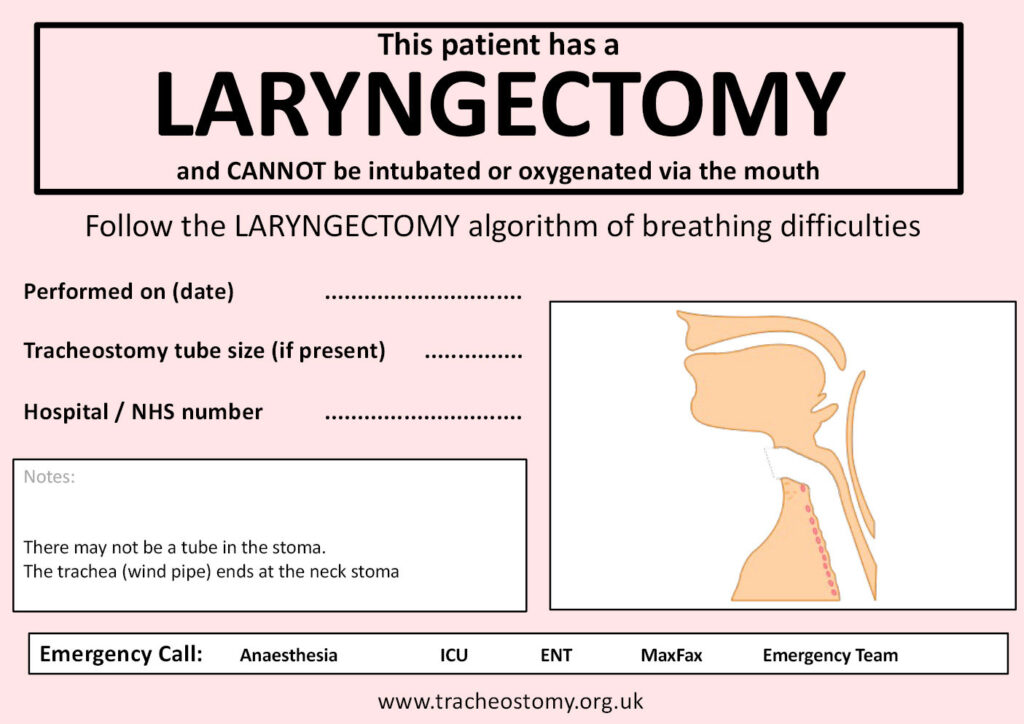
Figure 5: Laryngectomy bedside sign. Used with permission from Brendan McGrath and the National Tracheostomy Safety Project.
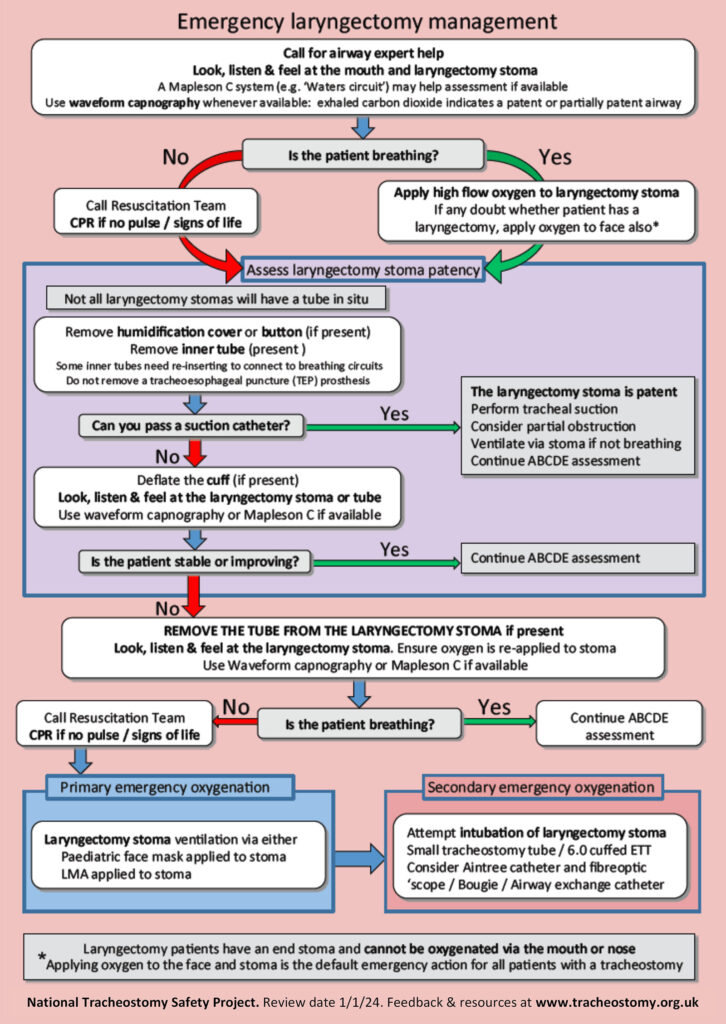
Figure 6: Laryngectomy management algorithm. Used with permission from Brendan McGrath and the National Tracheostomy Safety Project.
CONCLUSION
Patients with a tracheostomy are commonly encountered in clinical practice, and complications can occur. By understanding the recommended management steps, these complications can usually be managed to ensure that patients do not suffer harm related related to their artificial airway. Bedside signs can be an effective method provide pertinent information related to the airway and to assist providers with the recommended steps if the surgical airway is not functioning properly.
REFERENCES
- Mitchell RB, Hussey HM, Setzen G, et al. Clinical consensus statement: tracheostomy care. Otolaryngol Head Neck Surg. 2013;148;6–20. PMID: 22990518.
- Spataro E, Durakovic N, Kallogjeri D, Nussenbaum B. Complications and 30-day hospital readmission rates of patients undergoing tracheostomy: a prospective analysis. Laryngoscope. 2017;127:2746–2753. PMID: 28543108.
- Shah RK, Lander L, Berry JG, et al. Tracheotomy outcomes and complications: a national perspective. Laryngoscope. 2012;122;25–29. PMID: 22183625.
- De Leyn P, Bedert L, Delcroix M, et al. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg. 2007; 32;412–421. PMID: 17588767.
- McGrath BA, Bates L, Atkinson D, Moore JA. Multidisciplinary guidelines for the management of tracheostomy and laryngectomy airway emergencies. Anaesthesia. 2012; 67;1025–1041. PMID: 22731935.
- Rosero EB, Corbett J, Mau T, Joshi GP. Intraoperative airway management considerations for adult patients presenting with tracheostomy: a narrative review. Anesth Analg. 2021; 132;1003–1011. PMID: 33369928.
- Bontempo LJ, Manning SL. Tracheostomy emergencies. Emerg Med Clin N Am. 2019;37.1:109–119. PMID: 30454773.
- Rajendram R, Khan M, Joseph A. Tracheostomy tube displacement: an update on emergency airway management. Indian J Respir Care. 2017; 6:800–806. https://www.ijrc.in/doi/pdf/10.4103/ijrc.ijrc_12_17. Accessed March 30, 2025.
- Bodenham A, Bell D, Bonner S, et al. Standards for the care of adult patients with a temporary tracheostomy; standards and guidelines. Intensive Care Society. 2014; 29-32. https://www.wyccn.org/uploads/6/5/1/9/65199375/ics_tracheostomy_standards__2014_.pdf. Accessed March 30, 2025.
- Stamou D, Papakostas K, Turley A. Airway loss after recent tracheostomy: use of digital confirmation. Anaesthesia. 2010;65.2:214–215. PMID: 20402858.
- National Tracheostomy Safety Project. Green algorithm.Review date 1/1/24. https://tracheostomy.org.uk/storage/files/NTSP_GREEN_Algorithm_Double_sided_2.pdf. Accessed March 30, 2025.
- Lewith H, Athanassoglou V. Update on management of tracheostomy. BJA Education. 2019;19:370–376. PMID: 33456860.
- Cinar U, Halezeroglu S, Okur E, et al. Tracheal length in adult human: the results of 100 autopsies. Int J Morphol. 2016;34:232–236. https://www.scielo.cl/pdf/ijmorphol/v34n1/art33.pdf. Accessed March 30, 2025.
- Patiño MA, Truong DT, Truong A, Cata JP. Do not burn your airway bridge: a technique to safely exchange a tracheostomy tube for a tracheal tube. A&A Practice. 2016;7: 155–157. PMID: 27467904.
- Brenner MJ, Cramer JD, McGrath BA, et al. Oral intubation attempts in patients with a laryngectomy: a significant safety threat. Otolaryngol Head Neck Surg. 2021; 164:1040–1043. PMID: 33048019.
- National Tracheostomy Safety Project. Red algorithm. Review date 1/1/24. https://tracheostomy.org.uk/storage/files/NTSP_RED_Algorithm_Double_sided_2.pdf. Accessed March 30, 2025.
- Stephens M, Montgomery J, Urquhart CS. Management of elective laryngectomy. BJA Education. 2017;17: 306–311. https://www.semanticscholar.org/paper/Management-of-elective-laryngectomy-Stephens-Montgomery/1271ac04d7272d87201fa71c82f71e70036400f8. Accessed March 30, 2025.

