AUTHOR: Carin A. Hagberg, MD, FASA
Anesthesiology News
Management of the difficult airway remains one of the most relevant and challenging clinical situations encountered by anesthesia practitioners, as major adverse consequences can occur if the airway is not secured in a timely fashion. This edition of “Current Concepts in the Management of the Difficult Airway” marks the 16th anniversary of this review of airway devices and techniques that are currently available to manage both routine and difficult airways, regardless of setting.
Alternative Airway Devices
A common factor preventing successful tracheal intubation is the inability to visualize the vocal cords during the performance of DL. Many devices and techniques are now available to circumvent the problems typically encountered with a difficult airway using conventional DL.
Endotracheal Tubes/Guides
Advances in ET design have been made to facilitate both passage of the ET, such as the Parker Flex-Tip (Salter Labs), and tracheal intubation in narrowed airways, such as the Tritube (Ventinova Medical BV) and the Shiley Microlaryngeal ET (Medtronic). Several ET guides have been used to aid in intubation or extubation, including both reusable/disposable and solid/hollow introducers, stylets, and tube exchangers (Table–1).
Table–1. Endotracheal Tube Guides
| Name (Manufacturer) |

Description
|
Aintree Intubation Catheter
(Cook Medical) |
Polyethylene 19 Fr AEC allows passage of a FIS through its lumen. Has 2 distal side holes and is packaged with Rapi-Fit adapters. Color: light blue. |
| Arndt Airway Exchange Catheter Set (Cook Medical) |
Polyethylene 14 Fr AEC with a tapered end, multiple side ports, packaged with a stiff wire guide, bronchoscope port, and Rapi-Fit adapters. Color: yellow. |
Cobra Introducer
(Occam Design) |
15 Fr airway intubation guide with telescoping extension. Coudé tip and 3 side holes. Color: orange. |
Cobralet
(Occam Design) |
15 Fr airway intubation guide with hollow interior channel. Color: orange. |
| Cook Airway Exchange Catheter (Cook Medical) |
8.0, 11, 14, and 19 Fr polyethylene designs facilitate exchange of single-lumen tube or DLT of ≥4.0 mm ID. The DLT versions are EF with soft tips. Colors: yellow, green; soft tip is purple. |
| Cook Staged Extubation Set (Cook Medical) |
Soft-tipped marked extubation wire to maintain continuous airway access, wire holder and Tegaderm for securement, soft-tipped Reintubation Catheter, Rapi-Fit adapters to assist in oxygen delivery, if necessary. Available outside of US only. |
CoPilot VL Disposable Bougie
(Dilon Technologies) |
14 Fr polyethylene single-use ET introducer with coudé tip. Color: orange. |
CoPilot VL Rigid Intubation Stylet
(Dilon Technologies) |
Reusable CoPilot VL intubation stylet. |
D-BLADE Stylet
(KARL STORZ) |
Reusable stylet designed especially for the C-MAC reusable and single-use adult D-BLADE. Individually peel packed in boxes of 10. |
Flexible Tip Bougie
(Sharn Anesthesia) |
Steerable ET introducer with soft, flexible, and controllable tip. Ideal when there is a great view but advancing the ET is still a problem. |
Frova Intubating Introducer
(Cook Medical) |
Polyethylene 8.0 and 14 Fr AEC with angled distal tip with 2 side ports. Has hollow lumen and is packaged with a stiffening cannula and removable Rapi-Fit adapters. 14 Fr also packaged in box of 10. Colors: 8 Fr, yellow; 14 Fr, blue. |
| i-Bougie (VBM) |
Single-use 14 Fr introducer with angled tip and hollow lumen for oxygenation. Color: orange. |
Insight Rigid Stylet
(Bell Medical) |
Reusable and sterilizable. Designed to work with GlideScope, C-MAC, and Insight VL. |
| Introes Pocket Bougie (BOMImed) |
Single-use 14 Fr (4.7 mm) malleable ET introducer made from special blend of Teflon. Packaged in box of 10. |
| METTS Muallem ET Tube Stylet (VBM) |
Single-use 8.0, 12, 14 Fr stylet; malleable, but with soft and atraumatic coudé tip. Color: green. |
OptiShape
(Teleflex) |
Reusable, sterilizable, semirigid stylet with optimal shape memory for indirect intubation procedures. |
| Pocket Introducer (VBM) |
Single-use 15 Fr Introducer with coudé tip. Color: blue. |
Portex Single-Use Bougie
(Smiths Medical) |
15 Fr, PVC ET introducer with coudé tip. Has a hollow lumen that discourages reuse and is provided sterile. Color: ivory. |
| Portex Tracheal Tube Introducer (Smiths Medical) |
15 Fr ET introducer made from a woven polyester base, with a coudé tip (angled 35 degrees at its distal end). Also known as the gum elastic bougie. Color: golden brown. |
Rhinoguard
(Davis Medical) |
ET introducer/dilator. |
| RPiS (Rapid Positioning intubation Stylet) (Airway Management Enterprises) |
Single-use flexible stylet with tip that allows 180-degree flexion and retroflexion. Tip protrudes 5 cm from the end of ET. Color: blue. |
| S-Guide (VBM) |
Single-use 15 Fr stylet, malleable, with atraumatic coudé tip and hollow for oxygenation. |
| VBM Introducer (VBM) |
Single-use 15 Fr introducer with coudé tip and hollow for oxygenation. Color: orange. |
| VBM Tube Exchanger (VBM) |
Single-use 11, 14, and 19 Fr tube exchanger that is hollow to allow oxygenation. Color: blue. |
Vie Scope
(Adroit Surgical) |
Allows for a straight line-of-sight view with 360 degrees maximal illumination to pass a bougie between the vocal cords. Provides the ability to intubate the patient when awake in trauma situations both in the hospital and in the field. Single use. |
Voir Bougie
(Adroit Surgical) |
Single-use 15 Fr polyethylene ET introducer with formable tip. Colored safety bands: Light blue bougie with green and red safety depth marking bands gives the user immediate depth insertion distance for rapid and safe intubation. |
Lighted Stylets
Lighted stylets, when used alone, are a blind technique of intubation, as they rely on transillumination of the tissues of the anterior neck to demonstrate the location of the ET. These devices can be used with either DL or VL to allow direct visualization of the airway (Table–2).
Viewing Optical Stylets
Viewing optical stylets provide a view from the tip of the ET. Whereas the view from a VL is at the end of the laryngoscope, viewing optical stylets provide a view from the tip of the ET for steering the ET through the cords. The stylet size for this device allows it to be placed within an ET as an independent instrument, or as an adjunct to VL or DL. Additionally, some can be used to place an ET through intubating supraglottic ventilatory devices for visualization of ET placement through the SGA (Table–2). As an alternative to a viewing optical stylet placed inside the ET tip, the VivaSight-SL (ETView, Ambu) is a single-use ET with an integrated camera at the tip of the tube to provide a view for steering the ET through the cords. When in place, it provides continuous real-time monitoring of tube position (Table–2).
Table–2. Stylets
| Name (Manufacturer) |

Description
|
| Lighted Stylets |
Aaron Surch-Lite
(Bovie Medical Industries) |
10-in sterile, single-use, flexible stylet. |
AincA Lighted VideoStylet
(Anesthesia Associates) |
Easily malleable, lighted stylet with adjustable ET holder. Shapes and guides ET while forwardly illuminating passage. Completely reusable device consisting of removable handle with xenon bulb. |
Tube-Stat Oral Intubation Stylet
(Medtronic) |
Similar to AincA lighted VideoStylet. |
| Vital Signs Light Wand Illuminating Stylet (GE Healthcare) |
Similar to AincA lighted VideoStylet. |
| Viewing Optical Stylets |
| AincA VideoStylet (Anesthesia Associates) |
Easily malleable, video imaging stylet with built-in ET holder. Shapes and guides ET while forwardly illuminating the passage and providing full-color image. Completely reusable device consisting of removable VideoStylet and attached rechargeable LCD monitor. |
| APA Stylet (AAM Healthcare) |
Designed for use with the APA VL, works with the APA U-DAB (non-channeled difficult airway blade) to facilitate laryngoscopy in challenging intubations. Available in reusable, sterilizabled format. |
| Brambrink Intubation Endoscope (KARL STORZ) |
High-resolution semirigid fiber-optic stylet with a 40-degree curved shape at distal end, 40× magnification, fixed eyepiece, movable ET holder, and an insufflation port. |
| C-MAC Video Stylet (KARL STORZ) |
A high-resolution chip at the distal end of the endoscope. The tip can be angulated anteriorly by up to 90 degrees, which helps in the narrow conditions of the oral cavity. The patented active bend mechanism can be used with an attached ET and supports at the same time the passive return. Intuitive handling with universal C-MAC System interface for C-MAC Monitor (8403 ZXK) and C-MAC PM (8403 XD). |
| Clarus Levitan (Clarus Medical) |
Portable high-resolution fiber optics enclosed in a malleable stainless steel stylet provide a view from the tip of ET. Built-in tube stop to hold ET in place with integral oxygen port for oxygen insufflation during intubation. Assist with DL/VL like regular stylet to provide an added view from the tip of the tube, or can be used independently as an easier-to-learn, less expensive alternative to FIS. Also malleable to be used through intubating supraglottic ventilatory devices. Optional adapter uses smartphones to transform optics to video. |
| Clarus Pocket Scope (Clarus Medical) |
Conveniently sized, easy-to-clean, and cost-effective (reusable) flexible stylet that has a patented, deflected, nondirectable tip. Optional adapter uses smartphones to transform optics to video. Often used to confirm placement and patency of airways. |
| Clarus Shikani (Clarus Medical) |
Viewing stylet: high-resolution, stainless steel, malleable fiber-optic stylet. Has adjustable tube stop and integral oxygen port for oxygen insufflation. Assist with DL/VL like regular stylet to add a view from the tip of the tube. Or used independently as an easier-to-learn, less expensive alternative to bronchoscope. Also malleable for use through intubating supraglottic ventilatory devices. Optional adapter uses smartphones to transform optics to video. |
Clarus Video Stylet 3000V
(Clarus Medical) |
Malleable rigid stylet scope with attached LCD screen and adjustable curve shape provides view from end of stylet; built-in tube stop to hold ET in place with integral oxygen port for oxygen insufflation during intubation. Assist with DL/VL like regular stylet to provide view from the tip of the tube or used as independent device as an easier, less expensive alternative to FIS. Also malleable to be used through intubating supraglottic ventilatory devices. |
GlideRite Rigid Stylet
(Verathon) |
Reusable, sterilizable, rigid stylet specifically designed to work with GlideScope unique angle VL; provides improved maneuverability in ET placement. |
Insight Lighted Video Stylet
(Bell Medical) |
Malleable rigid stylet video scope with attached HD video display and adjustable curve shape provides view from end of stylet; built-in tube stop to hold ET in place with integral oxygen port for oxygen insufflation during intubation. |
J-Wand
(D R Burton Healthcare Products) |
Semirigid intubating stylet that can be used with both video and standard laryngoscopy equipment. Flexible angled introducer tip to facilitate ET placement. Oxygenation port built into handle enables providers to perform apneic oxygenation techniques during intubation process. |
| Viewing Optical Stylets |
| SensaScope (Acutronic Medical Systems) |
Hybrid S-shaped, semirigid fiber-optic intubation video stylet. Has a 3-cm steerable tip with video chip that can be flexed in sagittal plane 75 degrees in both directions with lever at proximal end of device. Has no working channel. |
| VivaSight-SL (ETView/Ambu) |
Single-use ET with an integrated camera at the tip. Image is displayed on a monitor via a cable. |
Table–3. Flexible Intubation Scopes
| Name (Manufacturer) |

Description
|
| aScope 3 Large (Ambu) |
Single-use FIS. OD: 5.8 mm; working channel ID: 2.8 mm. |
| aScope 3 Regular (Ambu) |
Single-use FIS. OD: 5.0 mm; working channel ID: 2.2 mm. |
| aScope 3 Slim (Ambu) |
Single-use FIS. OD: 3.8 mm; working channel ID: 1.2 mm. |
| aScope 4 Broncho Large (Ambu) |
Single-use FIS. OD: 5.8 mm; working channel ID: 2.8 mm. |
| aScope 4 Broncho Regular (Ambu) |
Single-use FIS. OD: 5.0 mm; working channel ID: 2.2 mm. |
| aScope 4 Broncho Slim (Ambu) |
Single-use FIS. OD: 3.8 mm; working channel ID: 1.2 mm. |
FIVE S Scope – Single-Use Flexible Intubation Video Endoscope
(KARL STORZ) |
New single-use FIVE S is compatible with the C-MAC Video Intubation Platform. Similar to the reusable FIVE Scope, the distal chip provides 300,000 pixels resolution and a wide angle of view, and its rigid sheath easily maneuvers to facilitate intubation in even the most challenging situations. |
Flexible Intubation Video Endoscope
(KARL STORZ) |
Compact, mobile endoscope. The FIVE Scope complements the C-MAC video intubation devices. All components, such as a camera control unit, camera head, light cable and light source, are already included in the C-MAC system. Distal chip technology enhances image quality, field of view, and aspect ratio to facilitate intubation. |
Insight Flexible Video Endoscope
(Bell Medical) |
Has a universal HD Insight Color Display that is 3.5 in and stores 70 h of video and 80,000 photos. Multiple-diameter FIS to work with infants and adults. |
Video Laryngoscopes
Video-assisted techniques have become pervasive in various surgical disciplines, as well as in anesthesiology. As more VLs are introduced into clinical practice, and as airway managers become more skillful with the technique of video-assisted laryngoscopy, it could well become standard procedure for patients with known or suspected difficult airways. It also may become the standard for routine intubations as the equipment and users’ skills improve and the cost of the devices decreases, with the potential for important savings in time and decreased morbidity in patients. It is beyond the scope of this review to discuss all of the laryngoscopes that have been manufactured; thus, only some of the most recently developed blades are described (Table–4).
Table–4. Video Laryngoscopes
| Name (Manufacturer) |

Description
|
Airtraq Avant
(Prodol Meditec;
distributed by Teleflex) |
Disposable VL that provides a magnified angular view of the glottis without alignment of oral, pharyngeal, and tracheal axes. Includes a guiding channel to both hold and direct ET toward the vocal cords. Reusable optic piece (up to 50 intubations) and anti-fog heater resists lens clouding. Disposable blade and eyecup. MRI conditional use. Also, optional camera and smartphone adapter. |
| Airtraq SP (Prodol Meditec; distributed by Teleflex) |
The SP model is single use with all the features of the Avant but fully disposable. Optional camera has an integrated touch screen and can be attached to all Airtraq models. It records and can connect via Wi-Fi to smartphone/iPad/iPhone/PC. |
APA
(AAM Healthcare) |
Offers continuous oxygen delivery during laryngoscopy, MAC and MIL style blades for use in pediatric, adult, and difficult airway patients. APA VL’s modular design, along with its 3.5-in monitor, allows the user to choose the airway management technique required based on each patient. A disposable cover for the device is also available to protect it from contamination risks and a stylet to assist laryngoscopy. |
C-MAC
(KARL STORZ) |
Instant-on, battery-powered VL with standard-shaped interchangeable MAC and MIL blades for neonates through obese adults as well as a difficult airway blade (D-BLADE) for very anterior airways. Blades house high-resolution CMOS distal chip and LED technology. Real-time viewing on 7-in LCD monitor. Dörges D-BLADE has angle of view with approximately 80-degree acute curvature design. |
| C-MAC Pocket Monitor (KARL STORZ) |
Highly portable rescue device, 3.5-in monitor fits directly on all C-MAC premium class reusable and single-use blades and the C-MAC Video stylet. LCD 4.3 ratio high-resolution screen works in direct sunlight; rechargeable and removable lithium ion battery lasts 1 h; ergonomic screen can be moved in several directions and folded away for transport; fully immersible. Offers video and still picture recording conveniently located at the laryngoscope handle. |
C-MAC S
(KARL STORZ) |
The highly versatile, reusable S-Imager can be used with the C-MAC 7-in LCD monitor or portable 3.5-in Pocket Monitor. Both modalities offer video and still picture recording conveniently located at the laryngoscope handle. Anti-fog feature. Uses single-use blades. Imager is available in adult and pediatric sizes. |
CoPilot VL+
(Dilon Technologies) |
Portable VL designed to be used in multiple settings for every intubation. Rechargeable lithium polymer battery provides >2 h continuous use. Durable and portable. |
GlideScope AVL
(Verathon) |
Features a digital color monitor with integrated real-time recording, snapshot and on-screen playback capability. Video Batons incorporate the Reveal anti-fog mechanism to resist lens fogging. Six single-use blade options. |
GlideScope Go
(Verathon) |
GlideScope Go is the new hand-held, high-resolution VL system. Durable, portable, and intuitive, it uses the portfolio of fully disposable, single-use blades, designed to maximize first-pass success and minimize infection rates in routine and difficult intubation, in patients ranging from neonates to large adults. |
GlideScope Ranger
(Verathon) |
Portable VL designed for EMS and military paramedics. Compact and rugged. Operational in seconds. Video Batons incorporate the Reveal anti-fog mechanism to resist lens fogging. Six single-use stat options. |
| GlideScope Titanium Reusable (Verathon) |
GlideScope Titanium system features high-resolution, full-color digital camera and monitor for real-time viewing and recording; features durable, lightweight titanium construction with built-in Reveal anti-fog mechanism; streamlined, low-profile blade designs; and snapshot and on-screen playback features. |
GlideScope Titanium Spectrum Single-Use
(Verathon) |
GlideScope Spectrum Single-Use is the newest-generation VL from Verathon, featuring cutting-edge advances in lighting and camera technology and offers a comprehensive range of sizes for your smallest to largest patients, difficult to routine airways in a unique, fully disposable blade design. |
Insight VL
(Bell Medical) |
One of 6 airway devices that use the universal HD Insight video display. Insight video display fits flexible endoscopes, rigid lighted stylet, and VL. The displays are interchangeable on all Insight devices. |
IntuBrite VLS 6600 Portable
(Salter Labs) |
IntuBrite VLS 6600 uses a unique DUAL LED lighting system for exceptional clarity and anatomic definition. Large, high-resolution color display with vertical tilt adjustment. Video recording and still shot capability. Compatible range of reusable blades and single-use sheaths for neonates to adult patients. Durable aluminum and stainless steel handle and blade construction for demanding environments that require portability. |
IntuBrite VLS 8800
(Salter Labs) |
IntuBrite VLS 8800 makes the benefits of video laryngoscopy accessible to all intubations in a high-quality system. Video recording and still shot capability. Compatible with a range of reusable blades and single-use sheaths for neonates to adult patients. |
| i-view (Intersurgical) |
Single use, fully disposable VL incorporating a MAC blade to allow direct and indirect view. Ergonomic design provides an optimal view in a variety of light conditions. |
| King Vision (Ambu) |
Durable, fully portable digital VL with a high-quality reusable display and disposable blades. Hand-held, on-board display avoids cables and encourages patient focus; disposable blades incorporate camera and light source so fresh optics for each use. |
| King Vision aBlade (Ambu) |
Reusable video adapter attaches to the existing display to allow use of lower-cost aBlades. Durable, fully portable digital VL with a high-quality reusable display and disposable aBlades. Hand-held, on-board display avoids cables and encourages patient focus. |
| McGrath MAC (Medtronic) |
Portable VL intubation platform designed for routine use. Equipped with either disposable MAC blades or hyperangulated blades for more anterior airways. Durable (drop tested to 2 m) and submersible. Screen displays minute-by-minute battery life countdown for improved reliability. |
| VividTrac (Fujifilm/SonoSite) |
Video intubation device that works on many computer systems equipped with USB II port as a standard USB camera, using available video camera applications on Windows, Mac, and Linux systems. Alternatively, automated video display software (VividVision) can be downloaded. |
Indirect Rigid Fiber-Optic Laryngoscopes
These laryngoscopes were designed to facilitate tracheal intubation in the same population that would be considered for flexible scope intubation (FSI), such as patients with limited mouth opening or neck movement. Relative to the flexible intubation scopes (FIS), they are more rugged in design, control soft tissue better, allow for better management of secretions, are more portable (with the exception of the new portable FIS), and are not as costly. Intubation can be performed via the nasal or oral route and can be accomplished in awake or anesthetized patients (Table–5).
Table–5. Specialty Rigid Laryngoscopes
| Name (Manufacturer) |

Description
|
| Dörges Emergency Laryngoscope Blade (KARL STORZ) |
Developed in Europe as a universal blade that combines features of both the MAC and MIL laryngoscope blades. |
| Modified MAC Blades |
| AincA Flex-Tip Fiber-Optic Laryngoscope Blade (Anesthesia Associates) |
Flexible tip or levering fiber-optic MAC laryngoscope blades designed with a hinged tip controlled by a lever at the proximal end. Designed to fit standard handles. |
AincA Macintosh Viewing Prism
(Anesthesia Associates) |
An optically polished viewing prism for attachment to most MAC laryngoscope blades (conventional OR fiber-optic). Effectively repositions the practitioner’s viewpoint to the forward portion of the MAC curve via a 30-degree refraction without inverting the image. Clips to the vertical flange of the MAC to “look around the curve of the blade.” |
| NOVALITE Flex-Tip Fiber Optic Blade (NOVAMED USA) |
Designed with an integrated fiber-optic bundle for maximized light transmission and optimal task illumination. Using advanced XENON light technology, NOVALITE fiber-optic laryngoscopes deliver enhanced illumination for safer intubations. |
| NOVALITE MRI Conditional Laryngoscope (NOVAMED USA) |
Featuring NOVAMED “ULTRA BRITE” fiber-optic laryngoscope technology to afford clinicians a solution for intubations within the magnetic resonance (MR) environment—ensuring improved response time, enhanced patient safety, and minimized risk for trauma. |
Vie Scope
(Adroit Surgical) |
Allows for a straight line-of-sight view with 360 degrees maximal illumination to pass a bougie between the vocal cords. Provides the ability to intubate the patient when awake in trauma situations both in the hospital and in the field. Single use. |
Supraglottic Ventilatory Devices
The LMA (Laryngeal Mask Airway; Teleflex) is the single most important development in airway devices in the past 25 years. Since its introduction into clinical practice, it has been used in more than 300 million patients worldwide. Other supraglottic ventilatory devices are available for routine or rescue situations. The most recently developed supraglottic ventilatory devices have a gastric channel or are intended to be used as a conduit for FIS (Table–6).
Table–6. Supraglottic Ventilatory Devices
| Name (Manufacturer) |

Description
|
| AES Ultra (AES) |
All-silicone laryngeal mask with standard cuff valve. |
| AES Ultra Clear (AES) |
Silicone cuff and PVC tube, laryngeal mask with standard cuff valve. |
| AES Ultra EX (AES; distributed by Anesthesia Associates) |
All-silicone, multiple-use laryngeal mask. |
| AES Ultra Flex EX (AES; distributed by Anesthesia Associates) |
All-silicone, wire-reinforced, multiple-use laryngeal mask. |
| air-Q (Cookgas) |
Hypercurved intubating laryngeal airway that resists kinking, and removable airway connector. Anterior portion of mask is recessed; larger mask cavity allows intubation using standard ETs. air-Q removal after intubation is accomplished by using air-Q reusable removal stylet. |
| air-Q Blocker (Cookgas) |
Combines the features of air-Q Disposable laryngeal mask, with an additional soft, flexible guide tube located to the right of the breathing tube. This channel provides access to the esophagus with a NGT or Blocker tube that allows clinicians to vent, suction, and further block the esophagus. |
| air-Q Disposable (Cookgas) |
Hypercurved intubating laryngeal airway with removable color-coded connectors. Anterior portion of mask is recessed; larger mask cavity allows intubation using standard ETs. air-Q removal after intubation is accomplished by using air-Q reusable removal stylet. |
| air-Q SP (Cookgas) |
Combines features of the air-Q reusable laryngeal masks with added advantage of a self-pressurizing mask. No inflation line or pilot balloon is needed. PPV or spontaneously breathing patients inflate the mask during the uptake of ventilation. |
| air-Q SP Disposable (Cookgas) |
Combines features of the air-Q disposable laryngeal masks with added advantage of a self-pressurizing mask. No inflation line or pilot balloon is needed. PPV or spontaneously breathing patients inflate the mask during the uptake of ventilation. |
Aura40
(Ambu) |
Same design as the Ambu AuraOnce, but reusable. |
Aura40 Straight
(Ambu) |
Same design as the Ambu AuraStraight, but reusable. |
| AuraFlex (Ambu) |
Disposable wire-reinforced flexible laryngeal mask. |
| AuraGain (Ambu) |
Second-generation laryngeal mask, featuring anatomic curve for rapid placement, gastric access for suction and decompression of the stomach via a gastric tube, and integrated direct intubation capability for management of expected or unexpected difficult airway. |
| Aura-i (Ambu) |
A laryngeal mask with built-in curve and bite blocker designed as a conduit for optical tracheal intubation. |
AuraOnce
(Ambu) |
A laryngeal mask with a special built-in curve that replicates natural human anatomy. It is molded in 1 piece with an integrated inflation line and no epiglottic bars on the anterior surface of the cuff. |
AuraStraight
(Ambu) |
A straight laryngeal mask featuring a single-mold design and an extra-soft, thin cuff which easily conforms to the airway. |
Block Buster Intubating Laryngeal Mask Airway
(Bell Medical) |
Multifunctional intubating SGA made with silicone. |
i-gel
(Intersurgical) |
A second-generation, single-use SGA with a non-inflating cuff, designed to mirror the perilaryngeal anatomy, with an integral bite block, buccal cavity stabilizer, and gastric channel. Also incorporates wide-bore airway channel for use as a conduit for intubation with flexible scope guidance (sizes 3-5). |
| i-gel O2 Resus Pack (Intersurgical) |
A second-generation, single-use SGA with a supplementary oxygen port designed to facilitate ventilation during CCR. A color-coded hook ring is used to secure the airway support strap and aids in size identification. Non-inflating cuff that mirrors the perilaryngeal anatomy, with an integral bite block, buccal cavity stabilizer, and gastric channel. The pack contains an i-gel O2, a sachet of lubricant, and an airway support strap. |
| KING LT-D (Ambu) |
Disposable, single-lumen tube with 2 low-pressure cuffs. Intended for insertion into upper esophagus with ventilatory openings aligned with tracheal inlet; distal cuff seals the esophagus and the proximal cuff seals the oropharynx. |
| KING LTS-D (Ambu) |
Disposable double-lumen laryngeal tube with separate ventilation and gastric access channels. Intended for insertion Into upper esophagus with ventilatory openings aligned with the tracheal Inlet; distal cuff seals the esophagus and the proximal cuff seals the oropharynx. |
LMA Classic
(Teleflex) |
Safe, general-purpose airway for routine elective inpatient and outpatient surgical procedures. |
LMA Classic Excel
(Teleflex) |
Has the benefits of LMA Classic, and its improved design facilitates intubation. |
LMA Fastrach
(Teleflex) |
Designed to facilitate blind intubation without moving head or neck, allowing for single-handed insertion. Allows continuous ventilation between intubation attempts. |
LMA Flexible
(Teleflex) |
Has a reinforced airway tube that allows it to be positioned away from the surgical field while maintaining a good seal. |
LMA Gastro with Cuff Pilot Technology
(Teleflex) |
LMA specifically designed to give clinicians control of their patients’ airways while facilitating direct endoscopic access via the integrated endoscope channel. Once placed, the LMA Gastro Airway facilitates end-tidal CO2monitoring throughout the procedure to support patient safety. |
LMA ProSeal
(Teleflex) |
Double-cuff design enables seal pressures ≥30 cm H2O to be achieved, and the drain tube separates the alimentary and respiratory tracts. |
LMA Protector with Cuff Pilot Technology
(Teleflex) |
Second-generation SGA with silicone cuff designed to achieve an oropharyngeal seal equivalent to the LMA ProSeal Airway (>30 cm H20). Combines a pharyngeal chamber and dual gastric drainage channels, designed specifically to minimize gastric insufflation and facilitate gastric access. |
LMA Supreme
(Teleflex) |
Combines features of previous LMAs to provide increased safety and ease of use. The higher seal pressure and gastric access provide a higher degree of safety. Designed to channel fluids away from the airway in the unlikely event of active or passive regurgitation and allows for diagnostic positioning. |
LMA Unique
(Teleflex) |
Original, single-use LMA with design based on LMA Classic. Available with or without syringe and lubricant. |
LMA Unique EVO with Cuff Pilot Technology
(Teleflex) |
First-generation, silicone cuffed LMA that offers ET intubation capabilities. |
LMA Unique with Cuff Pilot Technology
(Teleflex) |
A versatile, single-use, first-generation laryngeal mask with a medical-grade silicone cuff and integrated cuff pressure manometer. |
| Portex Clear PVC, Oral/Nasal, Soft Seal Cuff Tracheal Tubes (Smiths Medical) |
Similar in shape to the first-generation laryngeal mask, but differs in its 1-piece design, in which the cuff is softer and there is no “step” between the tube and the cuff, an integrated inflation line, no epiglottic bars on the anterior surface of the cuff, and a wider ventilation orifice. |
| Shiley (Medtronic) |
A disposable, cost-effective LM airway with integrated cuff inflation line. Designed to form a low-pressure seal around the laryngeal inlet and maintain a secure airway. |
| Shiley Esophageal Endotracheal Airway, Double Lumen (Medtronic) |
A disposable DLT that combines the features of a conventional ET with those of an esophageal obturator airway. Has a large proximal latex oropharyngeal balloon and a distal esophageal low-pressure cuff with 8 ventilatory holes in between. |
Soft-Seal
(Smiths Medical) |
Similar in shape to the first-generation laryngeal mask, but differs in its 1-piece design, in which the cuff is softer and there is no “step” between the tube and the cuff, an integrated inflation line, no epiglottic bars on the anterior surface of the cuff, and a wider ventilation orifice. |
Solus Curve
(Intersurgical) |
A single-use SGA designed for those who prefer the insertion characteristics of a curved device. Includes a classic cuff shape, integral inflation line, and a high-quality valve. |
Solus Flexible
(Intersurgical) |
A range of single-use SGA with a wire-reinforced tube, permitting flexion without kinking. Includes a classic cuff shape, integral inflation line, and a high-quality valve. |
Solus MRI Safe
(Intersurgical) |
A range of single-use SGA fitted with specially tested nonferrous valves, guaran-teed not to interfere with the magnet in an MRI scanner. The plastic valve has been selected to ensure full reliability throughout the shelf life of each device. |
Solus Satin
(Intersurgical) |
A range of single-use SGA with a softer airway tube to provide more flexibility. Provides a classic cuff shape, an integral inflation line, and a high-quality valve. |
Solus Standard
(Intersurgical) |
A range of single-use SGA featuring a low-friction material, classic cuff shape, integral inflation line, and a high-quality valve. |
Special Airway Techniques
Awake Intubation
For managing patients in whom a difficult airway is suspected or anticipated, securing the airway before induction of general anesthesia adds to the safety of anesthesia and helps minimize the possibility of major complications, including hypoxic brain damage and death. To perform awake intubation, the patient must be adequately prepared for the procedure. Good topical anesthesia is essential to obtund airway reflexes and can be provided by various topical agents and administrative devices (Table–7). Other relatively new devices can be used to best position patients and maintain an open airway during awake intubation (Table–8).
Table–7. Devices for Special Airway Techniques
| Name (Manufacturer) |

Description
|
| Awake Intubation |
Break-Away Airway
(Bell Medical) |
Intubation airway designed for use with a FIS for difficult intubation. The airway acts as an intubation guide to direct the scope. Once ET is inserted, the airway easily spreads or breaks away from the ET, allowing for the airway to be removed from the patient’s mouth. |
Capnography and Oxygen Mask for Procedural Sedation, POM Mask
(Bell Medical) |
Designed for delivering high concentrations of oxygen and monitoring end-tidal CO2 during procedural or conscious sedation cases, such as upper GI, ERCP, EUS, and EGD. |
EZ-Spray EZ-100
(Alcove Medical) |
Atomizer that delivers a 15- to 60-micron mist of medication in a cost-effective, easy to use, disposable unit. |
LMA MADgic
(Teleflex) |
Mucosal atomization device that incorporates a small flexible, malleable tube with an internal stiffening stylet that connects to 3-mL syringe. |
LMA MADgic Airway
(Teleflex) |
For difficult and awake airways requiring a FIS, the device combines atomized topical anesthetic and oxygen delivery in an innovative and elegantly designed flexible scope–compatible oral airway. |
LMA MAD Nasal
(Teleflex) |
Disposable, compact atomizer for delivery of medications to the nose and throat in a fine, gentle mist. |
| LMA MADomizer Bottle Atomizer (Teleflex) |
Bottle atomizer comes with a positive displacement pump for delivering a variety of medications to the nose and hypopharynx. |
Model 15-RD Glass Atomizer
(DeVilbiss Healthcare) |
Metal atomizer; includes glass receptacle (for liquid), pair of metal outlet tubes extending from metal atomizing nozzle, and adjustable tip for directing spray to inaccessible areas of the throat. Can be used with or without RhinoGuard tip cover. |
| Retrograde Intubation |
| Cook Retrograde Intubation Set (Cook Medical) |
Available as a complete set in 6.0, 11, or 14 Fr. The 14 Fr version includes Airway Exchange Catheter with Rapi-Fit adapters allow for delivery of oxygen. |
| Face Mask Ventilation and Nasal Oxygenation |
Comfort Flo
(Teleflex) |
Heated Humidified High Flow Nasal Cannula Therapy (HH-HFNCT) |
Endoscopy Mask
(VBM) |
Face mask with diaphragm to allow simultaneous ventilation and endoscopy. |
Ergomask
(Tuoren Medical Inc/Richard’s Medical) |
Mask with asymmetrical dome with a contoured ridge and a colored marker for finger placement. |
Flow-Safe II+ Disposable BiLevel CPAP System
(Mercury Medical) |
Disposable BiLevel CPAP system with deluxe mask with comfortable head harness, including a color-coded manometer for verifying BiLevel CPAP or CPAP pressure. Flow-Safe II+ works with standard flowmeters that can deliver >10 cm H2O CPAP pressure or approximately 10 cm H2O IPAP pressure at 15 L/min. The Bilevel CPAP switch allows clinicians to provide either therapy mode. |
Flow-Safe II EZ CPAP System
(Mercury Medical) |
System includes an integrated nebulizer that requires only 1 oxygen source to run both the CPAP and nebulizer devices. CPAP system includes color-coded manometer for verifying CPAP pressure and pressure-relief system. Flow-Safe II EZ works with standard flowmeters that can deliver >10 cm H2O at 15 L/min. Higher flow pressures may be necessary when running both CPAP and the nebulizer. |
Optiflow THRIVE System
(Fisher & Paykel Healthcare) |
Humidified oxygenation system with heated inspiratory tubing and anatomically designed high-flow nasal cannula. Packaged in box of 10. |
Super NO2VA Nasal PAP Ventilation System
(Vyaire Medical) |
Nasal mask capable of delivering noninvasive PPV when connected to an anesthesia circuit or Mapleson circuit utilizing low fresh gas flows from simple wall oxygen. |
| Transtracheal Jet Ventilation |
AincA Manual Jet Ventilator
(Anesthesia Associates) |
Portable jet ventilation device with thumb depression mechanism that initiates controlled burst of oxygen flow. Customizable assembly includes DISS inlet connection, 5 ft of inlet tubing, flow control knob, on/off thumb control, internal filter, back pressure gauge, and 2 ft of outlet hose ending in a luer-lock male fitting. Connects to any tool or port that has a luer-lock female connection (ie, malleable stylets, various adapters, etc). |
AincA MRI Conditional 3.0-Tesla Jet Ventilator
(Anesthesia Associates) |
Similar to AincA Manual Jet Ventilator but certified MRI conditional–compatible for use in units ≤3.0 Tesla strength. |
GO-PAP
(Pulmodyne) |
Emergency disposable CPAP device, with integrated nebulization. |
Manual Jet Ventilator
(Instrumentation Industries) |
Complete set includes an on/off valve, 6 ft of high-pressure tubing, and 4 ft of small-bore tubing. |
Manujet III
(VBM) |
Complete set including 13-ft high-pressure hose assembly with oxygen DISS fittings, 40-degree small-bore tube assembly (with luer lock fitting) and 3 jet ventilation catheters (13, 14, and 16 G). |
O2-MAX
(Pulmodyne) |
Emergency disposable CPAP device, with integrated nebulization. |
O2-MAX Trio
(Pulmodyne) |
Emergency disposable CPAP device, with integrated nebulization. |
Transtracheal Catheter
(Acutronic Medical System) |
Small jet needle for puncturing the trachea in an emergency for use with jet ventilation. |
Table–8. Positioning Devices
| Name (Manufacturer) |

Description
|
Chin-UP Airway Support Device
(Dupaco; distributed by Mercury Medical) |
Hands-free airway support device used to lift up patient’s chin and hold it in position to keep the airway open. |
Face-Cradle Prone Support System
(Mercury Medical) |
Fully adjustable cushion set accommodates most adult head sizes. |
Pi’s Pillow
(American Eagle Medical) |
A foam base and removable pad that supports the head in full extension position (sniffing) and maintains proper alignment of the upper airway during airway management. |
Rapid Airway Management Positioner (RAMP)
(Airpal Patient Transfer Systems) |
Air-assisted medical device that can be inflated to transfer and position patients for various procedures. |
Troop Elevation Pillow
(CR Enterprises; distributed by Mercury Medical) |
Foam positioning device that quickly achieves the H.E.L.P. Includes many accessories (head cradle, arm board pads, and TEPA). An impermeable barrier cover is also offered for infection control and to protect the product. |
Atomizing devices currently available for delivering topical anesthesia to nasal, oral, pharyngeal, laryngeal, and tracheal tissues include the DeVilbiss Model 15-RD Glass Atomizer (DeVilbiss Healthcare), the LMA MADgic (Teleflex) atomizer, and the LMA MADgic Airway (Teleflex; Table–7). Although any technique of tracheal intubation can be performed under topical anesthesia, FSI is most commonly used.
Flexible Scope Intubation
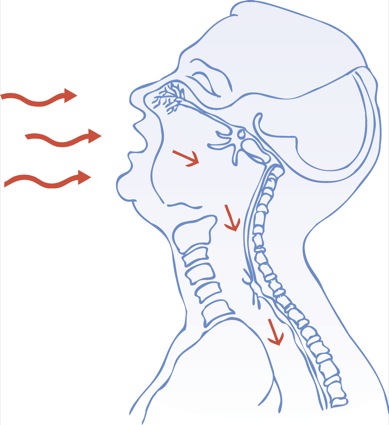
FSI is a very reliable approach to difficult airway management and assessment. It has a more universal application than any other technique. It can be used orally or nasally for both upper and lower airway problems and when access to the airway is limited, as well as in patients of any age and in any position.
Technological advances—including improved optics, battery-powered light sources, better aspiration capabilities, increased angulation capabilities, and improved reprocessing procedures—have been developed. The Airway Mobilescope (MAF; Olympus) is a portable, flexible endoscope with expanded viewing and recording capability, incorporating a monitor, LED light source, battery, and recording device in a single unit. Also available is the Ambu aScope 3 and aScope 4 Broncho, disposable, sterile, portable, flexible endoscopes with a fully functional suction/working channels (Table–3).
Rescue techniques, such as DL and placing a retrograde guidewire through the suction channel, may be performed if the glottic opening cannot be located with the scope, or if blood or secretions are present. Insufflation of oxygen or jet ventilation through the suction channel may provide oxygen throughout the procedure, and allow additional time when difficulty arises in passing the ET into the trachea.
Retrograde Intubation
Retrograde intubation (Table–7) is an excellent technique for securing a difficult airway either alone or in conjunction with other airway techniques. Every anesthesia care provider should be skilled in employing this simple, straightforward technique. It is especially useful in patients with limited neck mobility that is associated with cervical spine pathology or in those who have suffered airway trauma. Cook Medical has 2 retrograde intubation sets: a 6.0 Fr for placing tubes at least 2.5 mm ID, and a 14.0 Fr for placing tubes at least 5.0 mm ID.
Transtracheal Jet Ventilation (TTJV) and Small–Gauge Lumen Ventilation
TTJV is a well-accepted method for securing ventilation in rigid and interventional bronchoscopy, and there are several commercial manual jet ventilation devices available (Table–7). An AincA MRI Conditional 3.0 Tesla manual jet ventilator (Anesthesia Associates) is also now available to enable TTJV in the MRI suite for both planned and emergency procedures (Table–7). The Ventrain (Ventinova Medical B.V.) is a single-use ventilation device specifically designed for difficult or obstructed airway situations, allowing ventilation through small–gauge lumens. Ventrain is not a traditional jet ventilator: Its ventilation is not based on a continuous high pressure to induce inspiration; instead it is based on a continuous and bidirectional gas flow, inducing both inspiration and expiration. Thus, Ventrain not only supplies oxygen during the inspiration phase, but also actively removes gas from the lungs with Expiratory Ventilation Assistance (EVA). Ventrain enables adequate ventilation through small–gauge lumen catheters, as well as in situations when the airway is obstructed.
Cricothyrotomy
Cricothyrotomy (Table–9), a lifesaving procedure, is the final option for “cannot-intubate, cannot-ventilate” patients according to all airway algorithms, whether they concern prehospital, ED, ICU, or surgical patients. In adults, needle cricothyrotomy should be performed with catheters at least 4 cm and no more than 14 cm in length. A 6.0 Fr reinforced fluorinated ethylene propylene Emergency Transtracheal Airway Catheter (Cook Medical) has been designed as a kink-resistant catheter for this purpose. Percutaneous cricothyrotomy involves using the Seldinger technique to gain access to the cricothyroid membrane. Subsequent dilation of the tract permits passage of the emergency airway catheter. Surgical cricothyrotomy is performed by making incisions through the cricothyroid membrane using a scalpel, followed by the insertion of an ET. This is the most rapid technique and should be used when equipment for the less invasive techniques is unavailable and speed is particularly important.
Table–9. Cricothyrotomy Devices
| Name (Manufacturer) |

Description
|
| Needle Cricothyrotomy |
Emergency Transtracheal Airway Catheter
(Cook Medical) |
6 Fr reinforced fluorinated ethylene propylene catheter. |
| Percutaneous Cricothyrotomy |
Control-Cric
(Pulmodyne) |
Contents include a Cric-Knife, which is a dual-sided 10-mm scalpel with integrated sliding tracheal hook, and a Cric-Key, which is a cuffed 5.5-mm cric tube, with a preloaded stylet to allow for tactile feedback of the tracheal rings. |
Melker Cuffed Emergency Cricothyrotomy Catheter Set
(Cook Medical) |
Complete set including syringe (10 cc), 2- to 18-G introducer needles with TFE catheter (short and long), 0.038-in diameter Amplatz extra-stiff guidewire with flexible tip, scalpel, curved dilator with radiopaque stripe, and PVC airway catheter. Also available in a Special Operations kit, which includes all of the above in a slip peel pouch and 2 airway catheters. |
Pertrach Emergency Cricothyrotomy Kit
(Pulmodyne) |
Contents include 2 splitting needles, cuffed or uncuffed trach tube, dilator with flexible leader, twill tape, syringe, extension tube, and scalpel (optional). |
| Quicktrach I Quicktrach II (VBM) |
Complete set includes airway catheter, stopper, needle, and syringes that come preassembled. Quicktrach I (without cuff) Quicktrach II (with cuff) |
| Surgical Cricothyrotomy |
| Melker Surgical Cricothyrotomy Set (Cook Medical) |
Cuffed cricothyrotomy tube, scalpel, tracheal hook Trousseau dilator, and blunt, curved dilator in compact package for convenient storage. |
Melker Universal Cuffed Emergency Cricothyrotomy Catheter Set
(Cook Medical) |
Same as Melker Cuffed Emergency Cricothyrotomy Catheter Set for percutaneous technique. Also includes for surgical technique: tracheal hook, safety scalpel, Trousseau dilator, and blunt curved dilator. |
Rüsch Easycric
(Teleflex) |
Complete Seldinger-based cricothyrotomy set, premounted EasyCric tube and dilator (hydrophilic coated, anatomically shaped). |
ScalpelCric
(VBM) |
Scalpel cricothyrotomy set “stab-twist-bougie-tube” |
Surgicric
(VBM) |
Surgical cricothyrotomy set. Surgicric I: rapid 4-step technique; Surgicric II: classic surgical technique; Surgicric III: Seldinger technique |
Tracheostomy
Tracheostomy (Table–10) establishes transcutaneous access to the trachea below the level of the cricoid cartilage. Emergency tracheostomy may be necessary when acute airway loss occurs in children under the age of 10 years or those whose cricothyroid space is considered too small for cannulation, as well as in individuals whose laryngeal anatomy has been distorted by the presence of pathologic lesions or infection.
Percutaneous dilatational tracheostomy is the most commonly performed tracheostomy technique, yet it is still considered invasive and can cause trauma to the tracheal wall. Translaryngeal tracheostomy, a newer tracheostomy technique, is considered safe and cost-effective, and can be performed at the bedside. It may be beneficial in patients who are coagulopathic. Surgical tracheostomy is more invasive, and should be performed on an elective basis and in a sterile environment.
Table–10. Tracheostomy Devices
| Name (Manufacturer) |

Description
|
| Percutaneous Dilatational Tracheostomy |
| Blom Tracheostomy Tubes (Pulmodyne) |
Available in 4 sizes. Each size offers the choice of nonfenestrated and uncuffed tubes, as well as fenestrated cuffed/uncuffed tubes along with other standard inner cannulas. |
| Ciaglia Blue Rhino G2 and Blue Dolphin BT Balloon-Assisted Percutaneous Tracheostomy Introducers (Cook Medical) |
Complete kit includes 24, 26, and 28 Fr loading dilators and Shiley 6 or 8 percutaneous disposable dual-cannula tracheostomy tube. Tray version available that includes lidocaine/epinephrine, connector, chlorhexidine skin prep, drape, needle driver, and suture. |
| Laserjet Catheter (Acutronic Medical Systems) |
Double-lumen jet catheter. |
| Portex Ultraperc Percutaneous Dilation Tracheostomy Kit (Smiths Medical) |
Complete set with or without a tracheostomy tube. |
| Shiley Flexible Adult Tracheostomy Tube (Medtronic) |
Each size features the choice of cuffed (with the patented TaperGuard cuff technology) or uncuffed versions. |
| Shiley TracheoSoft XLT Extended-Length Tracheostomy Tubes (Medtronic) |
Available in 4 ISO sizes (5, 6, 7, and 8 mm ID). Each size offers the choice of cuffed or uncuffed stylets, and proximal or distal extensions. Disposable inner cannula; replacements sold in packages of 10. |
| Weinmann Tracheostomy Exchange Set (Cook Medical) |
Includes Cook Airway Exchange Catheter, Tracheostomy loading dilators, and a Blue Rhino dilator for redilation if necessary. |
| Surgical Tracheostomy |
| Surgical tracheostomies are performed by making a curvilinear skin incision along relaxed skin tension lines between sternal notch and cricoid cartilage. A midline vertical incision is then made dividing strap muscles, and division of thyroid isthmus between ligatures is performed. Next, a cricoid hook is used to elevate the cricoid. An inferior-based flap or Bjork flap (through second and third tracheal rings) is commonly used. The flap is then sutured to the inferior skin margin. Alternatives include a vertical tracheal incision (pediatric) or excision of an ellipse of anterior tracheal wall. Finally, the tracheostomy tube is inserted, the cuff is inflated, and it is secured with tape around the neck or stay sutures. |
Conclusion
Most airway problems can be solved with relatively simple devices and techniques, but clinical judgment born of experience is crucial to their application. As with any intubation technique, practice and routine use will improve performance and may reduce the likelihood of complications. Each airway device has unique properties that may be advantageous in certain situations, yet limiting in others. Specific airway management techniques are greatly influenced by individual disease and anatomy, and successful management may require combinations of devices and techniques.
Recommended Reading
- ASA Difficult Airway Algorithm. Anesthesiology. 2013;118(2):251-270.
- Artime C, Daily W, Hagberg CA. The Difficult Airway: A Practical Guide. New York, NY: Oxford University Press; 2013.
- Hagberg CA, ed. Benumof’s Airway Management, 4th Edition. Philadelphia, PA: Elsevier; 2018.
- Agro F, Barzoi G, Montecchia F. Tracheal intubation using a Macintosh laryngoscope or a GlideScope in 15 patients with cervical spine immobilization (letter). Br J Anaesth. 2003;90(5):705-706.
- Aoyama K, Nagaoka E, Takenaka I, et al. The McCoy laryngoscope expands the laryngeal aperture in patients with difficult intubation. Anesthesiology. 2000;92(6):1855-1867.
- Audenaert SM, Montgomery CL, Stone B, et al. Retrograde-assisted fiberoptic tracheal intubation in children with difficult airways. Anesth Analg. 1991;73(5):660-664.
- Aziz M, Abrons RO, Cattano D, et al. First-attempt intubation success of video laryngoscopy in patients with anticipated difficult direct laryngoscopy: a multicenter randomized controlled trial comparing the C-MAC D-Blade versus the GlideScope in a mixed provider and diverse patient population. Anesth Analg. 2016;122(3):740-750.
- Borg PA, Hamaekers AE, Lacko M, et al. Ventrain for ventilation of the lungs. Br J Anaesth. 2012;109(5):833-834.
- Brimacombe J, Keller C, Hörmann C. Pressure support ventilation versus continuous positive airway pressure with the laryngeal mask airway: a randomised, crossover study of anesthetized adult patients. Anesthesiology. 2000;92(6):1621-1623.
- Cavallone LF, Vanucci A. Extubation of the difficult airway and extubation failure. Anesth Analg. 2013;116(2):368-383.
- Cavus E, Neumann T, Doerges V, et al. First clinical evaluation of the C-MAC D-Blade video laryngoscope during routine and difficult intubation. Anesth Analg. 2011;112(2):382-385.
- Cook T, Woodall N, Frerk C, et al. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011;106(5):617-631.
- Cook T, Woodall N, Frerk C, et al. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. Br J Anaesth. 2011;106(5):632-642.
- Cooper RM. Use of a new videolaryngoscope (GlideScope) in the management of a difficult airway. Can J Anesth. 2003;50(6):611-613.
- Corley A, Caruana L, Barnett A, et al. Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth. 2011;107(6):998-1004.
- Davis L, Cook-Sather SD, Schreiner MS. Lighted stylet tracheal intubation: a review. Anesth Analg. 2000;90(3):745-756.
- Dörges V, Ocker H, Wenzel V, et al. The laryngeal tube: a new simple airway device. Anesth Analg. 2000;90(5):1220-1222.
- Enk D. Gas flow reversing element. Patent US 8,950,400 B2. United States Patent and Trademark Office; February 10, 2015.
- Enk D, Busse H, Meissner A, et al. A new device for oxygenation and drug administration by transtracheal jet ventilation. Anesth Analg. 1998;86(25):S203.
- Frass M, Kofler J, Thalhammer F, et al. Clinical evaluation of a new visualized endotracheal tube (VETT). Anesthesiology. 1997;87(5):1262-1263.
- Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115(6):827-848.
- Gaitini LA, Vaida SJ, Somri M, et al. A comparison of the Cobra, Perilaryngeal Airway, and Laryngeal Mask Airway Unique in spontaneously breathing adult patients. Anesthesiology. 2004;101:A518.
- Gomez-Rioz M, Freire-Vila E. The Totaltrack: an initial evaluation. Br J Anaesth. 2015;115(5):799-800.
- Gorback MS. Management of the challenging airway with the Bullard laryngoscope. J Clin Anesth. 1991;3(6):473-477.
- Groves N, Tobin A. High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care. 2007;20(4):126-131.
- Gupta B, McDonald JS, Brooks JH, et al. Oral fiberoptic intubation over a retrograde guidewire. Anesth Analg. 1989;68(4):517-519.
- Hamaekers AE, Borg PA, Enk D. Ventrain: an ejector ventilator for emergency use. Br J Anaesth. 2012;108(6):1017-1021.
- Hauswald M, Hauswald EK. Percutaneous cricothyroid jet ventilation using repetitive airway obstruction: a quick and simple way to ventilate the “impossible” airway. Acad Emerg Med. 2016;23(9):e16-e17.
- Hooshangi H, Wong DT. Brief review: the Cobra Perilaryngeal Airway (CobraPLA and the Streamlined Liner of Pharyngeal Airway (SLIPA) supraglottic airways. Can J Anaesth.2008;55(3):177-185.
- Kristensen MS, de Wolf MWP, Rasmussen LS. Ventilation via the 2.4 mm internal diameter Tritube® with cuff – new possibilities in airway management. Acta Anaesthesiol Scand. 2017;61(6):580-589.
- Kristensen M. The Parker Flex-Tip Tube versus a standard tube for fiberoptic orotracheal intubation: a randomized double-blind study. Anesthesiology. 2003; 98(2):354-358.
- Lorenz V, Rich JM, Schebesta K, et al. Comparison of the EasyTube and endotracheal tube during general anesthesia in fasted adult patients. J Clin Anesth. 2009;21(5):341-347.
- Miller CG. Management of the difficult intubation in closed malpractice claims. ASA Newsletter. 2000;64(6):13-19.
- Moore A, Gregoire-Bertrand F, Massicotte N, et al. I-gel versus LMA-Fastrach supraglottic airway for flexible bronchoscope-guided tracheal intubation using a Parker (GlideRite) endotracheal tube: a randomized controlled trial. Anesth Analg. 2015;121(2):430-436.
- Noppens RR. Ventilation through a “straw”: the final answer in a totally closed upper airway? Br J Anaesth. 2015;115(2):168-170.
- Patel P, Verghese C. Delayed extubation facilitated with the use of a laryngeal mask airway in the intensive care unit. Anaesthesia. 2000;55(4):396.
- Paxian M, Preussler NP, Reinz T, et al. Transtracheal ventilation with a novel ejector-based device (Ventrain) in open, partly obstructed, or totally closed upper airways in pigs. Br J Anaesth. 2015;115(2):308-316.
- Ritchie J, Williams A, Gerard C. Evaluation of a humidified nasal high-flow oxygen system, using oxygraphy, capnography and measurement of upper airway pressures. Anaesth Intensive Care. 2011; 39(6):1103-1110.
- Willemsen MG, Noppens R, Mulder AL, Enk D. Ventilation with the Ventrain through a small lumen catheter in the failed paediatric airway: two case reports. Br J Anaesth. 2014;112(5):946-947.
- Xue FS, Cheng Y, Li RP. Awake intubation with video laryngoscope and fiberoptic bronchoscope in difficult airway patients. Anesthesiology. 2013;118(2):462-463.
- Zamora J, Nolan R, Sharan S, et al. Evaluation of the Bullard, GlideScope, Viewmax, and Macintosh laryngoscopes using a cadaver model to simulate the difficult airway. J Clin Anesth. 2011;23(1):27-34.
- Zaouter C, Calderon J, Hemmerling TM. Videolaryngoscopy as a new standard of care. Br J Anaesth. 2015;114(2):181-183.
| Abbreviation Key |
| AEC |
airway exchange catheter |
| AHA |
American Heart Association |
| ARDS |
acute respiratory distress syndrome |
| ASA |
American Society of Anesthesiologists |
| AVL |
Advanced Video Laryngoscope |
| BAL |
bronchoalveolar lavage |
| BMI |
body mass index |
| BVM |
bag-valve-mask |
| CCD |
charge-coupled device |
| CCR |
cardiocerebral resuscitation |
| CMOS |
complementary metal oxide semiconductor |
| CO2 |
carbon dioxide |
| CPAP |
continuous positive airway pressure |
| CPR |
cardiopulmonary resuscitation |
| CPV |
Cuff Pilot Valve |
| DAB |
difficult airway blade |
| DCI |
direct-coupled interface |
| DISS |
diameter index safety system |
| DL |
direct laryngoscopy |
| DLT |
double-lumen tube |
| ED |
emergency department |
| EF |
extra firm |
| EGD |
esophagogastroduodenoscopy |
| EMS |
emergency medical services |
| ENT |
ear, nose, and throat |
| EPAP |
expiratory positive airway pressure |
| ERCP |
endoscopic retrograde cholangiopancreatography |
| ET |
endotracheal tube |
| EUS |
endoscopic ultrasound |
| EVA |
expiratory ventilation assistance |
| FDA |
US Food and Drug Administration |
| FiO2 |
fraction of inspired oxygen |
| FIS |
flexible intubation scope |
| FIVE |
Flexible Intubation Video Endoscope |
| Fr |
French |
| FSI |
flexible scope intubation |
| GI |
gastrointestinal |
| GVL |
GlideScope Video Laryngoscope |
| HD |
high-definition |
| HDMI |
High-Definition Multimedia Interface |
| HELP |
Head Elevated Laryngoscopy Position |
| HFNCT |
high-flow nasal cannula therapy |
|
| HH-HFNCT |
heated humidified high-flow nasal cannula therapy |
| ICU |
intensive care unit |
| ID |
internal diameter |
| ILMA |
intubating laryngeal mask airway |
| IPAP |
inspiratory positive airway pressure |
| ISO |
International Organization for Standardization |
| IV |
intravenous |
| LCD |
liquid crystal display |
| LED |
light-emitting diode |
| LM |
laryngeal mask |
| LMA |
Laryngeal Mask Airway |
| LT |
laryngeal tube |
| MAC |
Macintosh |
| MIL |
Miller |
| MRI |
magnetic resonance imaging |
| NGT |
nasogastric tube |
| NICU |
neonatal intensive care unit |
| NTSC |
National Television System Committee |
| OD |
outer diameter |
| OG |
orogastric |
| OR |
operating room |
| PAP |
positive airway pressure |
| PEEP |
positive end-expiratory pressure |
| PICU |
pediatric intensive care unit |
| POM |
procedural oxygen mask |
| PPV |
positive-pressure ventilation |
| PSI |
pounds per square inch |
| PVC |
polyvinyl chloride |
| PVP |
polyvinylpyrrolidone |
| RDT |
Remote Diagnostic Technologies |
| RTCA |
Radio Technical Commission for Aeronautics |
| SGA |
supraglottic airway |
| TEE |
transesophageal echocardiography |
| TEP |
Troop Elevation Pillow |
| TEPA |
Troop Elevation Pillow Addition |
| TFE |
tetrafluoroethylene |
| TTJV |
transtracheal jet ventilation |
| U-DAB |
unchanneled difficult airway blade |
| USB |
universal serial bus |
| UV |
ultraviolet |
| VL |
video laryngoscope/laryngoscopy |
| VLM |
video laryngeal mask |
|