Authors: Krishnakumar S et al
Cureus 17(7): e87989. doi:10.7759/cureus.87989
Abstract
Emergency below-knee amputation (BKA) in patients with significant comorbidities and coagulopathy presents formidable anesthetic challenges, as a central neuraxial blockade and general anesthesia are frequently contraindicated. We report the case of a 57-year-old female patient with uncontrolled diabetes mellitus, chronic kidney disease, coronary artery disease, and an elevated international normalized ratio (INR) of 1.6, necessitating urgent BKA for a septic diabetic foot ulcer. Ultrasound-guided peripheral nerve blocks (PNBs, popliteal sciatic and femoral) have been successfully employed to achieve effective intraoperative anesthesia and postoperative analgesia without bleeding complications or hemodynamic instability. This case underscores the safety and efficacy of ultrasound-guided PNBs as the preferred anesthetic strategy in high-risk patients with coagulopathy, offering a safer alternative to conventional methods and minimizing perioperative morbidity.
Introduction
Below-knee amputation (BKA) is a critical surgical intervention for limb-threatening conditions such as diabetic foot infections complicated by sepsis or osteomyelitis [1]. In emergency settings, patients with multiple comorbidities, including cardiovascular disease, renal impairment, and coagulopathy, pose significant anesthetic challenges. Central neuraxial blockade is contraindicated in patients with elevated international normalized ratio (INR) due to the risk of spinal hematoma, whereas general anesthesia may exacerbate hemodynamic instability in patients with compromised cardiac function [2,3]. Ultrasound-guided peripheral nerve blocks (PNBs) have transformed regional anesthesia by enabling precise visualization of neural and vascular structures and reducing complications even in anticoagulated patients [4,5]. This case report details the successful application of ultrasound-guided PNBs in a high-risk patient undergoing emergency BKA, highlighting their role as safe and effective anesthetic modalities in complex clinical scenarios.
Case Presentation
A 57-year-old female patient, weighing 71 kg, presented with a two-month history of a non-healing diabetic foot ulcer on the right foot, complicated by severe neuropathic pain, cellulitis, osteomyelitis, and systemic sepsis, necessitating urgent BKA. She reported an inability to ambulate for one month. Her medical history included poorly controlled diabetes mellitus (30 years), chronic kidney disease (one year), coronary artery disease with heart failure (15 years), spinal tuberculosis, and systemic hypertension (one year). Medications included insulin (human mixtard 8 units subcutaneously thrice daily), aspirin 75 mg daily, clopidogrel 75 mg daily, ramipril 2.5 mg daily, and sodium bicarbonate 500 mg daily.
On examination, the patient was conscious, oriented, febrile (temperature 37.8°C), tachypneic (respiratory rate 24 breaths/minute), and tachycardic (heart rate 112 beats/minute). She maintained 97% oxygen saturation at 5 L/min via a non-rebreathing mask but was hypotensive (blood pressure 90/60 mmHg, measured in the left arm, supine). Physical findings included bilateral pitting pedal edema, pallor, and coarse crepitations on chest auscultation. The right lower limb exhibited edema, blackish discoloration, and a nonhealing ulcer over the medial malleolus with absent peripheral pulses.
Laboratory investigations revealed hemoglobin of 9 g/dL, an INR of 1.6, and a normal platelet count (2.73 × 10^9/L). The bleeding time (two minutes 35 seconds) and clotting time (four minutes 45 seconds) were within normal limits. Renal function was impaired (urea, 73 mg/dL; creatinine, 1.6 mg/dL), and hypoalbuminemia (2.3 g/dL). Chest radiography showed bilateral pleural effusion, as evidenced by the blunted costodiaphragmatic angles. Electrocardiography demonstrated T-wave inversions in leads V1-V6 and left axis deviation. Echocardiography revealed global left ventricular hypokinesia, severe left ventricular dysfunction, mild tricuspid regurgitation, moderate pulmonary artery hypertension (41 mmHg), and an ejection fraction of 33%. The summary of patient comorbidities and risk profile is mentioned in Table 1.
Given the patient’s elevated INR, antiplatelet therapy, comorbidities, central neuraxial blockade, and general anesthesia were contraindicated. Ultrasound-guided popliteal sciatic and femoral nerve blocks (PNBs) were planned. The patient was classified as having American Society of Anesthesiologists (ASA) physical status IVe, and informed consent was obtained, acknowledging the risk of intraoperative major adverse cardiac events.
Standard ASA monitors (electrocardiogram, pulse oximetry, non-invasive blood pressure) were used, and an arterial line was secured in the right radial artery for invasive blood pressure monitoring. Supplemental oxygen (5 L/min) was administered, and minimal sedation was achieved with midazolam 0.5-1 mg and fentanyl (50 µg) intravenously.
The patient was positioned prone for a popliteal sciatic nerve block. A high-frequency linear ultrasound probe was placed at the popliteal fossa to identify the popliteal artery and to trace the bifurcation of the sciatic nerve. A 22-gauge Quincke spinal needle was inserted using the in-plane technique, and 20 mL of 0.25% bupivacaine was injected after negative aspiration. For the femoral nerve block, the patient was repositioned supine, and the probe was placed below the inguinal ligament to visualize the femoral artery and vein. Using the same needle and technique, 15 mL of 0.25% bupivacaine was administered after negative aspiration (Table 2).
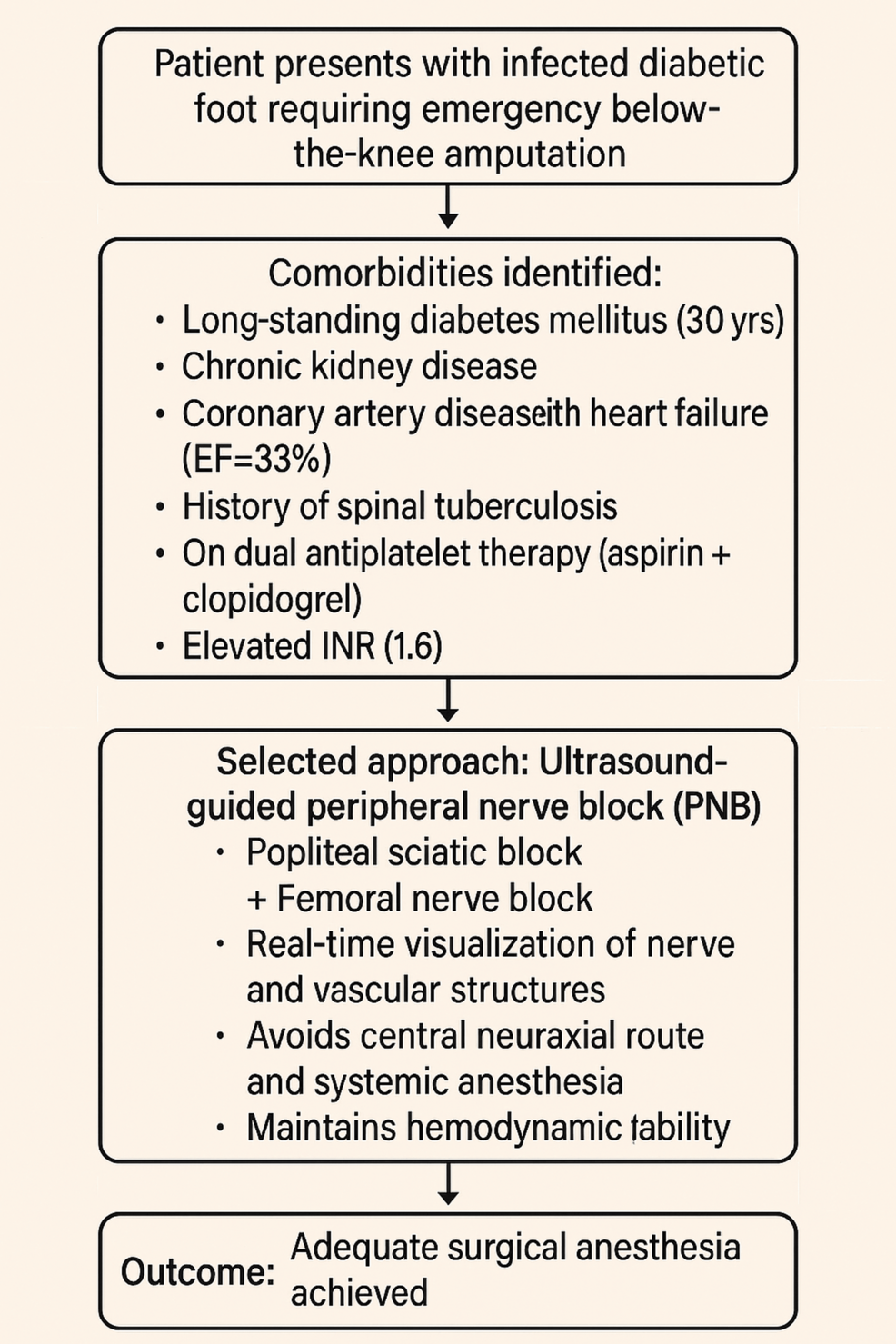
The workflow diagram (Figure 1) outlines the decision-making process for anesthetic management in a high-risk diabetic patient requiring emergency BKA. The patient had multiple comorbidities, including heart failure, chronic kidney disease, and spinal TB, and was on antiplatelet therapy with elevated INR, ruling out general and neuraxial anesthesia due to high risks. A landmark-based PNB was also unsuitable due to bleeding risks. Ultimately, an ultrasound-guided PNB was chosen for its safety, real-time visualization, and hemodynamic stability. This approach provided effective surgical anesthesia and analgesia without complications, demonstrating an individualized, risk-based anesthetic strategy in complex clinical settings.
Emergency BKA in high-risk patients with coagulopathy and multiple comorbidities requires meticulous anesthetic planning to optimize the perioperative outcomes. In this case, the patient’s elevated INR (1.6), antiplatelet therapy, severe cardiac dysfunction, and history of spinal tuberculosis contraindicated central neuraxial blockade and general anesthesia. Ultrasound-guided PNBs provide a safe and effective alternative, aligning with evidence from clinical studies supporting their use in complex scenarios [4,5,6].
Central neuraxial blockade is contraindicated in patients with an INR > 1.5, as outlined by the American Society of Regional Anesthesia and Pain Medicine (ASRA) guidelines, due to the risk of spinal or epidural hematoma, which can result in permanent neurological deficits [7]. General anesthesia was deemed high-risk in this patient, given her severe left ventricular dysfunction and hypotension. Induction agents and mechanical ventilation may reduce systemic vascular resistance and myocardial contractility, potentially precipitating cardiovascular collapse [8,9]. Additionally, the patient’s history of spinal tuberculosis likely caused vertebral deformities, complicating neuraxial needle placement and increasing the risk of technical failure [10].
Ultrasound-guided PNBs offer significant advantages in these cases. High-frequency ultrasound enables real-time visualization of neural and vascular structures, ensuring precise local anesthetic deposition and minimizing complications such as intravascular injection or nerve injury [4]. A systematic review by Joubert et al., conducted in Canada, analyzed observational studies and case reports and reported a bleeding complication rate of only 0.82% in anticoagulated patients undergoing PNBs, underscoring their safety in surgical settings [11]. Similarly, Ferraro et al., in a Brazilian case series involving orthopedic surgeries, demonstrated that ultrasound-guided PNBs are effective in anticoagulated patients, with negligible bleeding risk due to the direct visualization of vascular structures [5]. In contrast, landmark-based techniques, as studied by Maier et al. in a German cohort of patients undergoing lumbar sympathetic blocks, were less precise and associated with higher complication rates, including severe bleeding in anticoagulated patients [12].
Popliteal sciatic and femoral nerve blocks provided comprehensive anesthesia for BKA, covering the sciatic and femoral nerve distributions. Bupivacaine (0.25%) was selected for its prolonged duration of action, ensuring sustained intraoperative and postoperative analgesia, as supported by a systematic review by Gadsden et al., conducted in the United States, which evaluated local anesthetic concentrations in peripheral nerve blocks [13]. The absence of intraoperative hemodynamic changes and effective pain control (NPIS scores of 0 at four hours and three at 24 hours) highlights the efficacy of this approach. Furthermore, ultrasound guidance mitigated bleeding risks, despite the patient’s elevated INR and antiplatelet therapy, consistent with findings from a large cohort study by Chelly et al. conducted in the United States, which reported favorable outcomes with ultrasound-guided PNBs in high-risk surgical patients undergoing orthopedic procedures [14]. A retrospective study by Patel et al., performed in the United Kingdom, further supports the safety of PNBs in anticoagulated patients, noting minimal hemorrhagic complications in emergency surgeries [15].
This case has limitations, including its single-patient nature, which limits generalizability, and the lack of long-term follow-up data on functional recovery or infection resolution. However, successful intraoperative and immediate postoperative outcomes align with emerging evidence supporting ultrasound-guided PNBs in anticoagulated patients [16]. Future research should focus on prospective multicenter studies to establish standardized protocols for PNBs in high-risk populations, addressing optimal local anesthetic dosing, block techniques, and long-term safety.
Conclusions
Ultrasound-guided PNB represents a safe and effective anesthetic strategy for emergency BKA in high-risk patients with coagulopathy and multiple comorbidities. By facilitating the precise administration of local anesthetics and minimizing bleeding risks, this approach offers a superior alternative to central neuraxial blockade and general anesthesia, reducing perioperative morbidity and mortality. This case highlights the transformative potential of ultrasound-guided PNBs in complex surgical scenarios and advocates for their broader adoption in clinical practice. Further prospective studies are warranted to develop evidence-based guidelines for its use in patients receiving anticoagulation therapy.
References
- Adams CT, Lakra A: Below-knee amputation. StatPearls [Internet]. StatPearls Publishing , Treasure Island, FL; 2025.
- Neuraxial anesthesia and peripheral nerve blocks in patients on anticoagulant therapy. (2025). Accessed: 2025: https://www.nysora.com/topics/foundations-of-regional-anesthesia/patient-management/neuraxial-anesthesia-peripheral-n….
- Kaul TK, Tayal G: Anesthetic considerations in cardiac patients undergoing non-cardiac surgery. Indian J Anaesth. 2007, 51:280-6.
- Marhofer P, Greher M, Kapral S: Ultrasound guidance in regional anaesthesia. Br J Anaesth. 2005, 94:7-17. 10.1093/bja/aei002
- Martins LE, Ferraro LH, Takeda A, Munechika M, Tardelli MA: Ultrasound-guided peripheral nerve blocks in anticoagulated patients – case series. Braz J Anesthesiol. 2017, 67:100-6. 10.1016/j.bjane.2015.06.005
- Neal JM, Barrington MJ, Brull R, et al.: The second ASRA practice advisory on neurologic complications associated with regional anesthesia and pain medicine: executive summary 2015. Reg Anesth Pain Med. 2015, 40:401-30. 10.1097/AAP.0000000000000286
- Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT: Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine evidence-based guidelines (fourth edition). Reg Anesth Pain Med. 2018, 43:263-309. 10.1097/AAP.0000000000000763
- Swamy SN, Madhusudhana R: Attenuation of hemodynamic responses to endotracheal extubation with different doses of diltiazem with lignocaine: a placebo-controlled study. Anesth Essays Res. 2018, 12:428-33. 10.4103/aer.AER_28_18
- Wijeysundera DN, Beattie WS, Karkouti K, Neuman MD, Austin PC, Laupacis A: Association of echocardiography before major elective non-cardiac surgery with postoperative survival and length of hospital stay: population based cohort study. BMJ. 2011, 342:d3695. 10.1136/bmj.d3695
- Kearsley R, Elliott S, Smith C, Stocks G: The use of separate-level neuraxial anaesthesia for caesarean delivery in a patient with a history of spinal tuberculosis. Anaesth Rep. 2020, 8:e12051. 10.1002/anr3.12051
- Joubert F, Gillois P, Bouaziz H, Marret E, Iohom G, Albaladejo P: Bleeding complications following peripheral regional anaesthesia in patients treated with anticoagulants or antiplatelet agents: A systematic review. Anaesth Crit Care Pain Med. 2019, 38:507-16. 10.1016/j.accpm.2018.12.009
- Maier C, Gleim M, Weiss T, Stachetzki U, Nicolas V, Zenz M: Severe bleeding following lumbar sympathetic blockade in two patients under medication with irreversible platelet aggregation inhibitors. Anesthesiology. 2002, 97:740-3. 10.1097/00000542-200209000-00032
- Gadsden J, Hadzic A, Gandhi K, Shariat A, Xu D, Maliakal T, Patel V: The effect of mixing 1.5% mepivacaine and 0.5% bupivacaine on duration of analgesia and latency of block onset in ultrasound-guided interscalene block. Anesth Analg. 2011, 112:471-6. 10.1213/ANE.0b013e3182042f7f
- Chelly JE, Szczodry DM, Neumann KJ: International normalized ratio and prothrombin time values before the removal of a lumbar plexus catheter in patients receiving warfarin after total hip replacement. Br J Anaesth. 2008, 101:250-4. 10.1093/bja/aen132
- Patel PM, Leemputte MC, McCarthy RJ, Benzon HT: Retrospective analysis of peripheral nerve blocks in patients on anticoagulants and antiplatelet agents. Reg Anesth Pain Med. 2022, 47:372-4. 10.1136/rapm-2021-103054
- Liu SS, Ortolan S, Sandoval MV, Curren J, Fields KG, Memtsoudis SG, YaDeau JT: Cardiac arrest and seizures caused by local anesthetic systemic toxicity after peripheral nerve blocks: should we still fear the Reaper?. Reg Anesth Pain Med. 2016, 41:5-21. 10.1097/AAP.0000000000000329