Author: Michael Vlessides
Anesthesiology News
There is now a tool to help predict which patients are at greatest risk for unplanned readmission after ambulatory surgery.
“Readmission is often regarded as a measure of poor perioperative patient care and can also be a significant economic burden for both hospitals and patients,” said Maria PatrocÍnio, MD, a research fellow in anesthesia, critical care and pain medicine at Massachusetts General Hospital and Beth Israel Deaconess Medical Center, in Boston. “Although some studies have looked at readmission, they are very specific in terms of the population they looked at. There is not yet a generalized tool that can be applied to the broader population.”
Given this gap, Dr. PatrocÍnio and her colleagues sought to create a tool that could estimate the risk for readmission within 30 days of ambulatory surgery. “We looked at ambulatory surgery because it’s a time where we can actually identify patients who should be admitted to the hospital instead of being readmitted later on,” she said. “So it can actually be seen as a technique to prevent unplanned readmissions and its associated economic burden.”
As Dr. PatrocÍnio reported, 681 patients (2.4%) were found to have unplanned readmission within 30 days of surgery. As the Table illustrates, the final prediction tool was divided into four categories: patient characteristics, patient comorbidities, anesthesia-related characteristics and surgical-related characteristics.
| Table. Elements of the ROAMS Score, With Points Allotted for Each Predictor | |
| Characteristic | Score |
|---|---|
| Patient Characteristics | |
| BMI <18 kg/m2 | 5 |
| BMI >35 kg/m2 | 1 |
| ASA II | 3 |
| ASA III | 6 |
| ASA IV | 10 |
| ASA emergency status | 12 |
| Patient Comorbidities | |
| Leukemia/lymphoma | 1 |
| Beta-blocker use within 1 month | 3 |
| Liver disease | 3 |
| Chronic heart failure | 4 |
| History of DVT | 4 |
| Migraine 1 year prior | 4 |
| Solid tumor | 4 |
| Anesthesia-Related Characteristics | |
| High-dose long-acting opioid use | 2 |
| Nonuse of regional anesthesia | 4 |
| Surgical-Related Characteristics | |
| Duration of surgery (point per hour) | 2 |
| Sessler score ≥25 | 7 |
| Medium-risk surgical servicea | 4 |
| High-risk surgical serviceb | 9 |
| a Includes radiology, gastroenterology, pain, burns, orthopedics, plastic surgery, thoracic surgery, transplant surgery and urology. b Includes acute care surgery, neurosurgery and vascular surgery. BMI, body mass index; DVT, deep vein thrombosis; ROAMS, Readmission Of AMbulatory Surgical patients | |
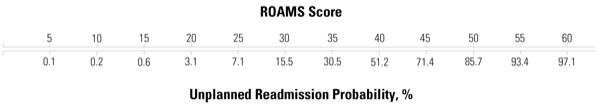
The Readmission of AMbulatory Surgical patients score, or ROAMS score, as the researchers call the predictive model, is a cumulative score that tallies up these various risk factors and provides a subsequent probability of readmission (Figure). For example, a ROAMS score of 20 coincides with an unplanned readmission probability of only 3.1%, whereas scores of 40 and 60 coincide with unplanned readmission probabilities of 51.2% and 97.1%, respectively.
Age, Surprisingly, Not a Factor
When applying the score model to the study group, the investigators found it had promising predictive utility, with an area under the curve of 0.80 (95% CI, 0.78-0.81). Of interest, the strongest predictors of readmission were ASA physical status III and IV, emergency status, high procedural severity (Sessler score >25), high-risk surgical service, and history of chronic heart failure, deep vein thrombosis, migraine within the past year and solid tumor.
The presentation garnered lively discussion when presented at the 2018 annual meeting of the International Anesthesia Research Society (abstract AMB55). “I see that age was excluded as a risk factor in your model,” said Chizoba Mosieri, MBBS, an associate professor of anesthesiology and the director of neurosurgical anesthesia at LSU Health Shreveport, in Louisiana.
“We initially included age as a predictor for readmission,” Dr. PatrocÍnio replied. “However, after doing the stepwise factors regression, we saw that it actually didn’t add anything to the model. Therefore we did not include it.”
“How many points or what percentage probability do you need to suggest that a patient should be considered an inpatient?” asked session moderator Jose Humanez, MD, an assistant professor of anesthesiology and perioperative medicine at the University of Alabama at Birmingham Hospital.
“That’s hard to say,” commented senior investigator Matthias Eikermann, MD, PhD, the director of research in the Critical Care Division at Massachusetts General Hospital, and a professor of anesthesia at Beth Israel Deaconess Medical Center. “We believe it should be taken into account based on individual hospital management strategies. So what is the readmission rate that you are able to accept? I guess that depends on many factors, including reimbursement strategies.
“This is a tool to help us determine the likelihood of readmission,” Dr. Eikermann added. “What the clinician does with that is beyond the scope of this study. Nevertheless, I think one of the implicit implications of this work is looking at exactly what you’re doing and perhaps identify some patterns that you would like to change.”
“In the end,” Dr. PatrocÍnio concluded, “the ROAMS [score] could help identify patients at risk for readmission after ambulatory surgery. Maybe it can help us think more thoroughly if certain patients should actually be inpatients instead of being discharged after ambulatory surgery.”

