Anesthesiology News
Associate Professor, Anesthesiology
Wake Forest School of Medicine
Winston-Salem, North Carolina
Wake Forest School of Medicine
Winston-Salem, North Carolina
Angioedema is an immunologic disorder that results in the rapid progression of localized subcutaneous or submucosal swelling that typically affects the face, lips, tongue, and pharynx.1,2Some common symptoms associated with angioedema include upper airway obstruction and/or difficulty swallowing, and the disorder also may affect the lower airway.3
In certain cases, angioedema may resolve on its own or with the administration of over-the-counter medications.7,8 However, the condition also may quickly become life-threatening if swelling increases and oxygenation and ventilation become impaired. Patients with angioedema usually present to the emergency department (ED) with different progressions of airway compromise.
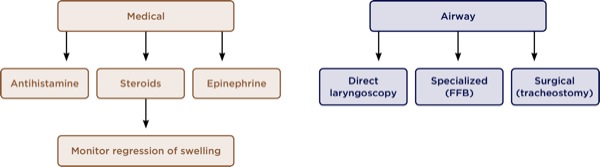
The condition may be treated in one of several ways: medical treatment with administration of antihistamines, epinephrine, and/or steroids; supportive airway management with supplemental oxygen; and, in more severe cases, airway management intervention with specialized devices or even a surgical airway (Figure 1).8
Airway management of patients with angioedema depends on the initial extent of the swelling and the patient’s airway indices. If the patient presents with a normal airway classification—good aperture of oral cavity, full neck range of motion and thyromental distance—with swelling, then airway management may differ from a patient who presents with inadequate range of motion and decreased thyromental distance in addition to swelling in the oral cavity.
Regardless of the airway indices and degree of swelling, proper objective evaluation of the progression of swelling over time is most critical and must be done quickly. Depending on the evaluation and perceived difficulty with intubation, the decision to intervene with airway management, as well as when and how to intervene (ie, with which airway device), may be challenging.
Once angioedema has been treated medically and swelling has reduced, there may not be a need to intervene with airway management. Once the decision to intervene has been established, the airway device and best technique must be chosen.
There are many different options for airway management that depend on the patient’s condition. Conventional bag-mask ventilation and direct or video laryngoscopy for intubation versus insertion of a flexible fiber-optic bronchoscope (FFB) nasally may be performed safely. If the airway indices are not adequate and progression of swelling is very rapid, then performing a cricothyrotomy or a tracheostomy may be required.
The current practice for evaluation of the status of swelling and airway patency for patients with angioedema includes the standard airway indices, such as Mallampati classification (I-III), oral aperture, and thyromental distance.9 These subjective measures, however, may not be accurate or may be difficult to discern as time goes on.
A newer, objective method includes taking pictures over time while quickly analyzing them with digital imaging software to track the progression/regression of the swelling. A patient presented to the ED of a small community hospital—Lexington Medical Center (part of Wake Forest Baptist Health), in Lexington, North Carolina—with an enlarged tongue, difficulty swallowing, and trouble speaking. After a history and initial assessment of the patient, lisinopril was discontinued in case this was a reaction to an ACE inhibitor, and the patient was admitted for further medical treatment and potential airway management.
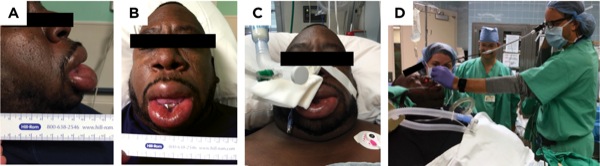
During examination of the patient, the ED physician noticed the severity of the tongue swelling; as a result, anesthesiology was consulted for airway assessment and intervention. Upon examination, the patient’s airway indices were measured: Mallampati class III, good oral aperture with an extremely swollen tongue, a thyromental distance of 3 fingerbreadths, and adequate neck extension (Figure 2).

Over time, the tongue swelling decreased with respect to the oral cavity, and the amount of unoccupied space increased significantly. The patient then became more asymptomatic, and there was consensus after several hours that intubation for definitive airway management was unnecessary.
Case presented as a medically challenging case at the 2016 annual meeting of the American Society of Anesthesiologists; Chicago, IL.
A 48-year-old man presented to the ER with severe angioedema of the oral cavity. After evaluation by the ED physician, anesthesiology was consulted, and initial medical management with diphenhydramine and epinephrine was administered. The patient was taking enalapril and sulfamethoxazole-trimethoprim for his current otitis media, which may have been the cause of the angioedema. At the time of initial consult, swelling was severe with an extremely limited mouth opening, and the patient was unable to communicate well.
Digital imaging was not required, as the tongue occupied nearly the entire oral cavity and there was not enough time to evaluate further (Figure 3). Therefore, written consent was obtained for photographs and urgent and definitive airway management was decided, and the patient was brought to the operating room (OR).
A consult was obtained from an ear, nose, and throat (ENT) surgeon as a backup in case of unsuccessful nasal intubation. An antisialagogue was administered with no other medications, and the upper airway (nasopharynx) was topicalized with lidocaine 5% ointment applied to both nares with a gloved finger. An FFB was used to intubate nasally; topicalization of the vocal cords and trachea with lidocaine 4% was administered via the instrument channel of the FFB using an epidural catheter. The patient was successfully intubated through the left nare in the OR.
After intubation, midazolam was administered and an infusion of dexmedetomidine was started. The patient was transported to the ICU, and later transferred to the main campus where he was safely extubated 4 days later.
Case presented as a medically challenging case at the 2017 annual meeting of the American Society of Anesthesiologists; Boston, MA.
Angioedema with severe swelling may become life-threatening and require urgent airway management. Rapid assessment of the airway and monitoring of the regression or progression of swelling are important in order to decide whether to intervene.
In addition, it may be difficult to identify the point at which the tongue swelling becomes severe enough to necessitate intubation. Digital imaging may provide a more objective and reliable measure to assist in determining whether airway management is needed. Close monitoring of the patient’s airway is imperative in order to choose which airway device and technique should be used if intervention is required. Depending on the oral aperture, the limitations of the airway devices due to the space available in the oral cavity should be considered. The key is knowing when to intervene in order to avoid a surgical airway (Figure 4).
Specialized airway devices, such as an FFB, may be safe alternatives to a surgical airway in the management of severe cases of angioedema. It is also imperative to consider the location within the hospital where airway management is to be performed (Figure 5). In less severe cases, the ED may be appropriate for airway management involving resolution after medications are administered; however, the OR provides a controlled environment with necessary equipment (ie, specialized airway devices) and an ENT surgeon as a potential backup if a surgical airway is required.
References
- Zuraw B, Bingham CO III. An overview of angioedema: clinical features, diagnosis, and management. In: Feldweg AM, ed. Waltham, MA: UpToDate; 2016.
- Moellman JJ, Bernstein JA, Lindsell C, et al. A consensus parameter for the evaluation and management of angioedema in the emergency department. Acad Emerg Med. 2014;21(4):469-484.
- Ishoo E, Shah UK, Grillone GA, et al. Predicting airway risk in angioedema: staging system based on presentation. Otolaryngol Head Neck Surg. 1999;121(3):263-268.
- Chiu AG, Newkirk KA, Davidson BJ, et al. Angiotensin-converting enzyme inhibitor-induced angioedema: a multicenter review and an algorithm for airway management. Ann Otol Rhinol Laryngol. 2001;110(9):834-840.
- Guyer AC, Banerji A. ACE inhibitor-induced angioedema. In: Feldweg AM, ed. Waltham, MA: UpToDate; 2016.
- Kamil RJ, Jerschow E, Loftus PA, et al. Case-control study evaluating competing risk factors for angioedema in a high-risk population. Laryngoscope. 2016;126(8):1823-1830.
- Barbara DW, Ronan KP, Maddox DE, et al. Perioperative angioedema: background, diagnosis, and management. J Clin Anesth. 2013;25(4):335-343.
- Chan NJ, Soliman AM. Angiotensin converting enzyme inhibitor-related angioedema: onset, presentation, and management. Ann Otol Rhinol Laryngol. 2015;124(2):89-96.
- Rosenblatt W. Angioedema – the decision to manage the airway should be definitive. Airway eLearning. 2016.
- Leech P, Riley ZD, Johnson KN, et al. Digital imaging software to assess the anatomic structures of the oral cavity in patients with thyroid masses; pilot study evaluating intubation and oxygenation difficulties when using videolaryngoscopy. Anesth Analg. 2016;122(5S suppl 3):S-18.