Author: Michael Vlessides
Anesthesiology News
Patients undergoing hip fracture fixation surgery who received spinal anesthesia had reduced 90-day mortality relative to those receiving general anesthesia, in a new study. The study also found spinal anesthesia to be superior to general anesthesia with respect to rates of pulmonary embolism, major blood loss and hospital length of stay.
“Hip fracture incidence continues to rise, due largely to our aging population,” said Sarah Tierney, MD, a regional anesthesia fellow at the University of Toronto. “Despite advances in health care, the mortality rate following hip fracture fixation has remained unchanged since the mid-1990s, with an annual incidence of approximately 30%.
“When spinal anesthesia is used over general anesthesia, it’s been shown that significant physiological benefits occur, including greater hemodynamic stability, lower incidence of respiratory events, less cognitive dysfunction in the immediate perioperative period, increased perioperative analgesia and decreased blood loss,” Dr. Tierney said. “Despite this, previous studies have been unable to show a strong mortality benefit for spinal anesthesia in patients undergoing hip fracture repair.”
Dr. Tierney and her colleagues used the institution’s electronic database to identify 2,591 patients who underwent hip fracture fixation between Jan. 1, 2003, and Dec. 31, 2015. A variety of clinical, laboratory and outcome data were extracted and mortality data were obtained from the hospital’s discharge database. The study was a propensity score, matched-pairs cohort study.
The main comparison was between spinal and general anesthesia, and the primary outcome was 90-day, in-hospital mortality. Secondary outcomes included 30- and 60-day mortality, hospital stay, pulmonary embolism, major blood loss and major acute cardiac events.
A total of 883 patients in the spinal anesthesia group were matched to patients in the general anesthesia group.
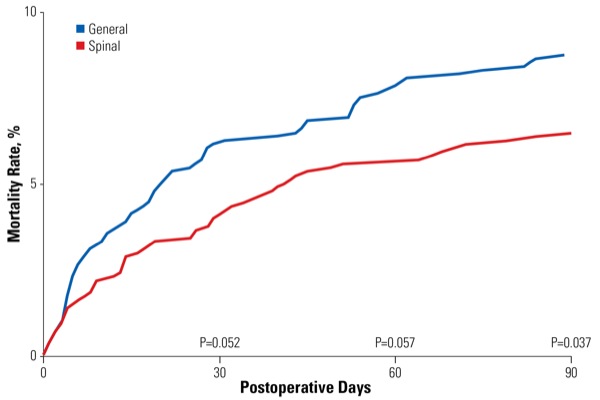
Reporting at the 2018 Joint World Congress on Regional Anesthesia and Pain Medicine and annual meeting of the American Society of Regional Anesthesia and Pain Medicine (abstract 4877), the investigators revealed that patients who received general anesthesia had a greater 90-day mortality (8.6%) than those who received spinal anesthesia (6.3%; P<0.001). Mortality did not differ significantly at the 30- and 60-day time points (Figure).
“The difference in 90-day mortality corresponded to a number-needed-to-treat of 44 patients, and an absolute risk reduction of 2.3%,” Dr. Tierney said. “Interestingly, although causes of death were varied, the spinal cohort was less likely to die from a cardiac event [19.7%] than patients who received general anesthesia [30.3%], but were more likely to die from respiratory events and sepsis. Nevertheless, our study was not adequately powered to assess for these outcomes.”
Spinal anesthesia was also found to result in significantly decreased rates of pulmonary embolism (0.5% vs. 2.3%; P<0.001) and major blood loss (4.8% vs. 7.7%; P<0.001). No differences were found between groups with respect to length of stay or major cardiac events.
“This is a very interesting study about a timely and relevant topic, especially given our increasing elderly population,” said session moderator Jaime Baratta, MD, a clinical assistant professor of anesthesiology at Thomas Jefferson University in Philadelphia. “Quite a few studies are being performed in this regard. Were you able, in your matched cohort, to control for patients in whom neuraxial anesthesia was contraindicated?”
“Some of those confounders may have balanced out when we controlled for things like pulmonary risk factors,” Dr. Tierney replied. “But it wasn’t necessarily controlled for in the study.” Dr. Tierney noted that there are multiple ongoing randomized controlled trials looking at quality of life and functional outcomes, such as return to home, return to function and days spent in rehabilitation facilities. Hopefully those will be published in the literature in the next year or two.”


Leave a Reply
You must be logged in to post a comment.