Hemoglobin level may not tell the whole story in cases of preoperative anemia. Instead, classifying anemia based on the size of red blood cells might predict clinical outcomes following elective cardiac surgery, a recent analysis concluded. Despite not having the most severe anemia, patients with macrocytic anemia had the highest risk for needing red blood cell (RBC) transfusions and experiencing postoperative complications.
“When evaluating patients, we recommend that clinicians not look at anemia as one condition but consider the size of the red blood cell for accurate risk assessment and targeted intervention,” said Lu Dai, MSc, at Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, in Ohio. “Valuable information may be lost when normocytic, microcytic and macrocytic anemia is studied as one homogeneous disease.”
As Ms. Dai reported, anemia, a common preoperative condition, is independently associated with adverse outcomes following surgery. It’s also linked to a number of downstream risks.
“Anemic patients are less likely to tolerate acute hemodilution during surgery, perioperative phlebotomy and surgical blood loss,” Ms. Dai said. “These factors predispose patients to red blood cell transfusions, which in turn further heighten the risk for poor outcomes.”
Although traditionally anemia is studied just by examining hemoglobin level or analyzing its severity, the investigators further classified anemia according to mean corpuscular volume (MCV) to see whether RBC size is predictive of different outcomes following surgery. From January 2010 to January 2014, there were 10,589 adult patients who underwent elective cardiac surgery at the Cleveland Clinic.
Ms. Dai and her colleagues defined anemia as a hemoglobin level less than 13 g/dL for men and less than 12 g/dL for women (Figure 1). The researchers then classified anemia by MCV: less than 80 femtoliters (fL) indicated microcytic (small average RBC size) anemia, 80 to 100 fL indicated normocytic (normal RBC size) anemia, and greater than 100 fL indicated macrocytic (abnormally large hemoglobin) anemia.
Hemoglobin Level Not The ‘Whole Story’
As Ms. Dai reported at the 2017 annual meeting of the International Anesthesia Research Society (abstract 1497), preoperative anemia was common in this cohort of patients, with 2,715 (26%) classified as anemic. Among patients with preoperative anemia, 2,365 (22%) were normocytic, 219 (2.1%) microcytic and 131 (1.2%) macrocytic.
“When we looked at hemoglobin levels, we saw that the microcytic group had the lowest median hemoglobin, which means they had the most severe anemia,” said Ms. Dai, who noted that median hemoglobin levels were 14.2 g/dL in nonanemic patients, 11.5 g/dL in normocytic, 11.2 g/dL in macrocytic and 10.7 g/dL in microcytic patients.
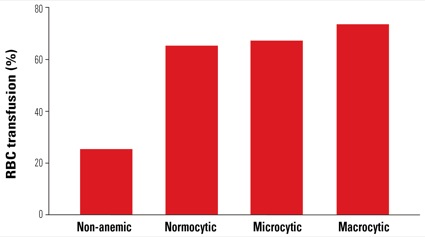
Transfusion rates also differed between groups. Compared with nonanemic patients, those with anemia had a higher odds ratio for receiving RBC transfusion, with macrocytic patients having the highest odds (Figure 2).
“This was interesting because macrocytic patients didn’t have the most severe anemia, but somehow they had the highest rate of transfusion,” Ms. Dai said.
Investigators also examined clinical outcomes after surgery, including prolonged ventilation, renal failure, in-hospital death and other complications (a composite of infection, vascular complications, stroke, coma, paralysis, pulmonary embolism, renal dialysis and gastrointestinal complications). Compared with nonanemic patients, those with normocytic anemia had higher risks for renal failure, other complications and in-hospital death (Figure 3).
“Surprisingly, those with microcytic anemia did not have higher risk of postoperative complications despite having the most severe anemia, i.e., the lowest median hemoglobin level,” Ms. Dai said.
“In fact, the microcytic group had the lowest risk of preoperative and postoperative atrial fibrillation. Those with macrocytic anemia, on the other hand, had higher risks of cardiac arrhythmias, renal failure, other complications and hospital death.”
The moderator of the session, Nancy Nussmeier, MD, a cardiac anesthesiologist at Massachusetts General Hospital, in Boston, asked whether a sample size of 131 macrocytic anemia patients was large enough to attain statistical significance.
“That was definitely a limitation of our study, as we initially tried to fit models that adjusted for several comorbidities,” Ms. Dai said. “Because of the small number of patients with macrocytic anemia, however, our logistic regression analysis adjusted for hemoglobin transfusion alone. We’re currently using more advanced methods to analyze these data, and propensity score matching has consistently shown us that macrocytic anemia is associated with the worst outcomes.
“A lot of these patients were put on bypass, and it’s possible that the larger red blood cells get more damaged with this technique or the duration of bypass is longer for macrocytic anemia,” Ms. Dai said. “It would be interesting to look at those data.”
“What jumps out to me is just how many patients undergoing elective surgery are anemic,” Dr. Nussmeier said. “Perhaps more attention should be paid to preoperative correction because anemia, regardless of the type, affects outcome.”




Leave a Reply
You must be logged in to post a comment.