Author: Michael Vlessides
Anesthesiology News
A survey has uncovered wide variability in how orthopedic surgeons interpret their patients’ postoperative opioid consumption after total knee arthroplasty (TKA).
The survey, performed at Stanford Health Care, also found that, on average, surgeons are quite accurate when estimating their patients’ true perioperative opioid use.
“This research originated from a [quality improvement] project here at Stanford where we compared medical records at our hospital system with our state’s prescription drug monitoring database [CURES] to better understand local patient demographics and opioid use patterns specific to our institution’s orthopedic surgery department,” said Theresa Lii, MD, a resident at Stanford Health Care, in Stanford, Calif.
Estimates Accurate on Average, but Disparate
As reported at the 2019 annual meeting of the American Academy of Pain Medicine (abstract 114), the researchers surveyed 36 orthopedic surgery residents, fellows and attendings at the institution. Respondents were asked to estimate the percentage of patients using opioids in the month before undergoing their TKA, as well as one to three months postoperatively.
Patients’ mean ASA physical status was 2.6±0.5; they consumed a mean of 165.0±180.8 morphine milligram equivalents during their inpatient stay.
As the Table illustrates, surgeons’ mean estimates of patient opioid consumption tracked closely with actual postoperative opioid prescription fills, which the researchers used as a surrogate for opioid consumption.
| Table. Patient Opioid Consumption Over Time | ||
| Surgeons’ Estimates | Actual Use | |
|---|---|---|
| Within 30 days of surgery, % | 23.5±18.9 | 14.8 |
| One month after surgery, % | 53.6±23.9 | 51.3 |
| Two months after surgery, % | 23.7±12.4 | 22.75 |
| Three months after surgery, % | 12.5±7.7 | 16.4 |
The survey also found there was no association between surgeons’ level of training and the accuracy or bias of their estimates.
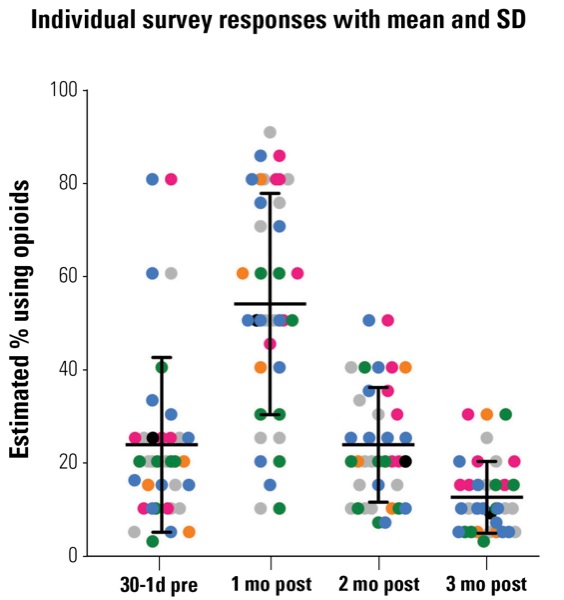
Yet as accurate as the surgeons may have been on average, the investigators were surprised by the wide variation in their responses. “If you look at the data point scatterplot, they’re all over the place,” Dr. Lii said in an interview with Anesthesiology News (Figure). “You have some surgeons who believe that none of their patients need opioids and subsequently estimate very low numbers of patients who use opioids. And then, some surgeons think their patients are in pain all the time and all of them need opioids.”
These results help illustrate areas of improvement for opioid stewardship, ones that likely apply to other institutions across the country. “At other institutions, some orthopedic surgeons may be overprescribing large, long prescriptions for their patients, who may fill the prescription and have full bottles sitting around the house, at risk of being diverted.”
More Education Needed
The disparities highlighted by the survey help illustrate the possible roles that education and cooperation may play in addressing the nation’s opioid crisis. “If you could educate surgeons on their patients’ opioid use patterns, then you could likely reduce variation in surgeon expectations,” Dr. Lii explained. “And once surgeons know what to expect from their patients in this respect, then they may be able to identify which patients require more and longer use of opioids than the average patients.
“That could prompt early referral to possible pain management specialists to pursue nonsurgical, nonopioid treatment of persistent pain,” she added. “And these pain specialists might even have the patients embark on a supervised opioid taper as they use other modalities to treat their pain.”
Andre P. Boezaart, MD, PhD, a professor of anesthesiology and orthopaedic surgery at the University of Florida, in Gainesville, found the study’s results surprising. “Personally, I would have guessed that surgeons may be more out of tune than these researches found,” he said. “I am sure anesthesiologists will fare much worse than the surgeons on the same questions, because they obviously do not really know the patients and the surgeries as well as the surgeons do.”
As Dr. Boezaart discussed, surgeons at high-volume institutions would be intimate with opioid requirements after total joint arthroplasties. “I would like to see the results of the same study with less known surgical procedures, such as spine surgery, where regional anesthesia does not play such a pivotal role,” he said.
Dr. Boezaart also expressed surprise that surgeons’ level of training and seniority were not a factor in this study. “I guess these numbers would look totally different in less academic settings,” he added.


Leave a Reply
You must be logged in to post a comment.