Author: Bob Kronemyer
Anesthesiology News
A multimodal analgesic approach to post–cesarean delivery pain management decreased the number of opioid tablets prescribed at discharge by 52%, according to a retrospective chart review presented at PAINWeek 2018.
The multimodal approach at Mount Sinai Hospital, in Chicago, consisted of analgesics with various mechanisms of action for an additive or synergistic effect in order to minimize opioid use. Nonopioid medications included nonsteroidal anti-inflammatory drugs, acetaminophen and gabapentin. For patient pain scores that were 7 and higher on a 10-point scale, hydromorphone was also part of the regimen.
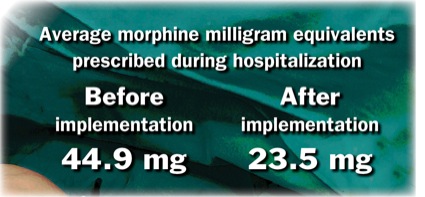
The records of 155 women before implementation of the pain management approach and 166 patients after implementation, from January to March 2018, found the average morphine milligram equivalents prescribed during hospitalization were 44.9 and 23.5 mg, respectively.
Multimodal analgesia was also associated with a decrease of one-half day in hospital length of stay.
“Before we designed the study, Mount Sinai Hospital was concerned with the high use of patient-controlled analgesia with morphine in post–cesarean section patients,” said co-investigator Lelas Shamaileh, a student at the University of Illinois in Chicago who is simultaneously pursuing a doctor of pharmacy and master of science in nutrition.
“The hospital was looking for alternative modalities for pain control,” Ms. Shamaileh said. However, the study authors discovered there were no concrete guidelines for pain management, specifically in the post–cesarean section patient population.
“We looked into the American Pain Society guidelines and enhanced recovery after surgery, both of which recommended multimodal analgesia,” Ms. Shamaileh said. “While there was literature to support multimodal analgesia in other operative settings, there was not strong data looking at this approach in this specific patient population. We felt our study would help the hospital find a way to decrease opiate use while also contributing data where there is a need for it.”
Ms. Shamaileh was pleasantly surprised that the study showed a reduction in length of hospital stay. “I anticipated that we would see adequate pain control because in our approach, we provided patients with around-the-clock pain management and because I saw from other studies that nonopiates used this way were effective for patients recovering from other surgeries,” she said. “I therefore anticipated that our strategy would have a positive impact on clinical practice. But I did not expect that our patients would be ambulating faster, and I did not anticipate the subsequent economic benefit—the reduction in length of stay gave us a projected annual savings of $4.8 million.”
“We hope to slowly implement this postoperative analgesic approach throughout all of surgery and continue contributing to the discussion on multimodal analgesia by sharing our experiences,” she said.
Striking a Balance
Ellen Battista, DNS, ANP, PNP, the owner of Pain Treatment Consultants of Western New York in Amherst, said the study’s findings reflect positive results for lowering average morphine milligram equivalents and decreasing the number of opioid tablets prescribed. “This study adds to our clinical knowledge of postoperative management in this population,” she said.
“Future research in this population is needed to evaluate the transition from inpatient to outpatient as it relates to a woman’s recovery, length of duration of pain treatment and possible effects/side effects,” she said.
A multimodal pain approach needs to be tailored to the individual woman’s clinical situation, according to Ms. Battista. “Women at childbearing age are typically younger, thus putting them theoretically more at risk of opioid addiction.”
Ms. Battista said risk assessment should be initiated at the time of admission for additional factors, such as current use of opioids; past addictions; smoking history; family history of opioid or other addictions, including those currently abusing; sexual abuse history; and mental health status.
“The stratification of risk is intended not to prohibit care to the patient, but rather strategize proper and effective treatment—inpatient and outpatient,” Ms. Battista said. “The patient should also be evaluated consistently for adequate control of pain and treatment modified to reflect the individual’s clinical needs.”
During hospitalization and at the appropriate time, patients should be informed of the risks and benefits of adequate pain management. “And prior to discharge, the patient and family need to be educated about safe storage of medications, disposal of drugs and the unintended consequences of drug sharing,” Ms. Battista said.
Furthermore, if pain persists longer than clinically expected, the patient should return for evaluation. “Undertreatment of pain has as many consequences as overtreatment of pain,” said Ms. Battista. “And the health care provider needs to closely monitor the clinical situation.”


Leave a Reply
You must be logged in to post a comment.