Author: Kim Mander
Anesthesiology News
An enhanced recovery pathway consisting of an evidence-based clinical care pathway significantly improved outcomes in patients undergoing esophagectomy, including reducing hospital length of stay (LOS) and increasing the rate of ambulation on day 1.
Discussing the basis of their program, researchers from Stanford School of Medicine and Stanford Hospital and Clinics, in California, said although enhanced recovery programs for esophagectomy are not new, there is a lack of consensus on the perioperative care of these patients because of insufficient evidence. “We sought to implement an evidence-based care pathway to reduce variation in postoperative treatment, enhance patient experience, and discharge at least 40% of patients who undergo an esophagectomy procedure by [postoperative day 7].”
The esophagectomy clinical pathway that was used in this study was developed by a multidisciplinary clinical team that included thoracic surgery, general surgery, anesthesiology, nursing, physical therapy and the hospital’s value-based care team.
“Patient demographic information, operative type, postoperative complications, and LOS were compared using student t-test and logistic regression between the two groups,” the researchers explained. Patients who had achalasia or major concurrent procedures were excluded from the analysis.
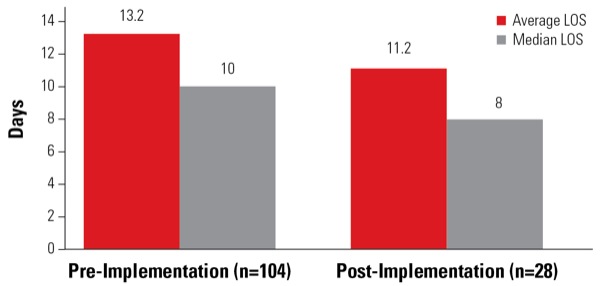
Presenting their results at the 2018 annual meeting of the American Society for Enhanced Recovery (abstract 36), Amy Lu, MD, MPH, a clinical assistant professor in the Department of Anesthesiology, Perioperative and Pain Medicine at Stanford University, said the enhanced recovery approach had proven to be promising, with a reduction in LOS (pre-implementation average, 13.2±9.0 days; post-implementation average, 11.2±9.6 days; P<0.01) (Figure) and lower rates of postoperative morbidities, albeit not statistically significant (Table). The enhanced recovery program increased ambulation rates on postoperative day 1. Patient demographics, postoperative complication rate, mortality rate and readmission rate did not differ significantly between the groups.
| Table. Demographic Information and Enhanced Recovery Process Measures Pre- and Post-Implementation | |||
| Pre-Implementation (n=104) | Post-Implementation (n=28) | P Value | |
|---|---|---|---|
| Age (year) | 65.5±9.8 | 62.3±10.9 | 0.278 |
| Male | 75% | 86% | 0.230 |
| BMI (kg/m2) | 25.7±4.8 | 24.6±4.2 | 0.288 |
| Reoperation | 9.6% | 7.1% | 0.686 |
| Post-op wound infection | 11.50% | 7.10% | 0.503 |
| Post-op pneumonia | 8.70% | 3.60% | 0.361 |
| Post-op prolonged ventilation >48 hours | 6.90% | 0% | 0.154 |
| Post-op renal failure | 1.90% | 0% | 0.460 |
| Post-op UTI | 6.90% | 3.60% | 0.946 |
| Post-op DVT | 1.00% | 0.00% | 0.602 |
| Post-op sepsis/septic shock | 8.70% | 14.30% | 0.375 |
| Discharge mortality | 1.00% | 0.00% | 0.602 |
| Discharge home | 92% | 89% | 0.608 |
| Readmission within 30 days after discharge | 4.80% | 0% | 0.237 |
| BMI, body mass index; DVT, deep ?vein thrombosis; UTI, urinary tract infection | |||
Dr. Lu told Anesthesiology News that when patients were not discharged within the targeted LOS for their enhanced recovery pathway, it was usually because they had multiple comorbidities and medical complications. “We decided to be conservative and include all patients undergoing esophagectomy on the pathway, rather than only include those who were less medically complex,” she explained.
She added that the esophagectomy pathway was one of approximately 10 enhanced recovery pathways currently being used at Stanford. The others are for colorectal, spine, gynecologic oncology and cardiac surgeries, as well as pancreatic resections and hepatectomies.


Leave a Reply
You must be logged in to post a comment.