Ensuring patient safety during surgical procedures remains at the forefront of quality improvement initiatives, as supported by APSF. In addition to administering and monitoring anesthesia, clinicians manage patient vital signs and overall well-being throughout the surgery, often in a very distracting environment.1 This is only made possible with the crucial help of medical alarms. These alarms are designed to alert the clinician and other medical staff to changes in patient vital signs, such as a drop in blood pressure or a decrease in oxygen saturation. However, clinicians often need to filter out the extraneous stimuli of the operating room to recognize and respond to these alarms. There are many disturbances that can draw the clinician’s attention away from the patient, including equipment delays, personal conversations, and pager/electronic device use.1 Furthermore, without the added confirmation of the patient’s subjective experience, clinicians must rely strictly on the data presented by the monitor, highlighting the importance of accurate and clinically actionable alarms. Medical alarms are an essential component of the clinician’s toolkit and help to ensure the safety of patients undergoing surgical procedures.
Alarm fatigue occurs when a user becomes desensitized to alarms due to excessive, non-actionable or invalid alarms, ultimately resulting in a delayed or no response.2,3 Alarm fatigue contributes to missed alarms and medical errors resulting in death, increased clinical workload and burnout, and interference with patient recovery—making it a safety issue that spans clinician to patient.4 The multifaceted approach to alarm fatigue should include consistent equipment, delaying alarm activation, and reducing alarm volume.2 In this article, we highlight the continued need for patient safety, and recent clinical and engineering advances in mitigating alarm fatigue.
Alarms are made to alert staff to a significant clinical change or a required action, though many can be nonactionable or invalid. Nonactionable alarms are alarms that require no action by the clinical care team and have been measured to comprise up to 85% of clinical alarms.5 In addition to nonactionable alarms, alarm fatigue can result from frequent invalid alarms.6 Invalid alarms occur due to device artifact or error, such as an electrocardiogram reporting ventricular tachycardia when the patient is actually in sinus rhythm and has a loose electrocardiogram lead. Invalid alarm rates have been measured to range from 85% to 99.4% of all clinical alarms.7 When alarms are consistently nonactionable or invalid, the priority for a user to respond may be lost or replaced with exasperation, accumulating in desensitization and dissatisfaction among health care staff.8 While individual personality traits and workload are not easily modifiable, alarm tones and thresholds are, making alarm research and innovation the key to decreasing alarm fatigue and desensitization.
These various factors converge to exacerbate alarm fatigue and subsequent effects of nonoptimal medical alarms. Fortunately, there are efforts underway from safety organizations, clinical workflow, and engineering innovations to prevent and combat these workplace and patient risks.
PATIENT SAFETY
The APSF recommends the use of medical alarms to help improve patient safety and reduce the risk of adverse events during the administration of anesthesia and perioperative period.9 Similarly, the American Society of Anesthesiologists Equipment and Facilities Committee (of which author, Joseph Schlesinger, is a member) prioritizes workplace safety and plans to release an “Alarm Position Statement” in late 2023. Additionally, addressing alarm fatigue and alarm impact on patients has been a focus for safety regulatory bodies. Alarm fatigue has been named a Top 10 safety priority for The Joint Commission every year since 2013.10 ECRI (originally founded as the Emergency Care Research Institute) has named missed alarms and alarm overload as a “Top 10 Health Technology Hazard” every year from 2012 to 2020.11 In 2011, the Association for the Advancement of Medical Instrumentation (AAMI) held a Medical Device Alarms Summit focused on alarm challenges, patient safety, and alarm research. Since then, AAMI has provided a variety of webinars and research grants to support the investigation and innovation of alarm fatigue prevention.
These patient safety-focused organizations remain dedicated to the improvement of the clinical environment, with a primary focus on innovating medical alarms. As a result of their dedicated safety initiatives and through the efforts of researchers around the globe, numerous advancements in medical practice and alarm design have been accomplished and are still underway.
CHANGES TO WHEN ALARMS SOUND
An effective adjustment to clinical alarms has consisted of individualizing alarm parameters2 to increase precision. Individualizing parameters consists of modifying the threshold of an alarm to reflect an individual patient’s physiologic status as compared to an unmodified default clinical alarm setting. Adjustments include alarm threshold tightening, adding delay periods between detection and alarm, disabling nonactionable alarms, and adjusting volume based on priority. These adjustments have been shown to reduce alarm rates (specifically nonactionable)12 and perceived workload.13 Evidence-based software has been developed to assist in safe and effective personalized thresholds. For example, Halley Ruppel, PhD, RN, and colleagues utilized and evaluated the impact of an alarm parameter customization software in an ICU.14 They found that the alarm parameter customization software significantly reduced the number of alarms by up to 16%, and the duration of alarms by up to 13%. This key study has shown that alarm parameter customization can have a profound impact on the alarm atmosphere and function in a hospital, especially for clinicians who frequently respond to alarms.
CHANGES TO HOW ALARMS SOUND
In addition to adjusting when an alarm sounds, innovating how an alarm sounds is an opportunity to make them more learnable, communicative, and tolerable. For anesthesia professionals, alarms are frequently concurrent and occur during procedures that require visual attention, making the need to have clear and communicative alarms critical.
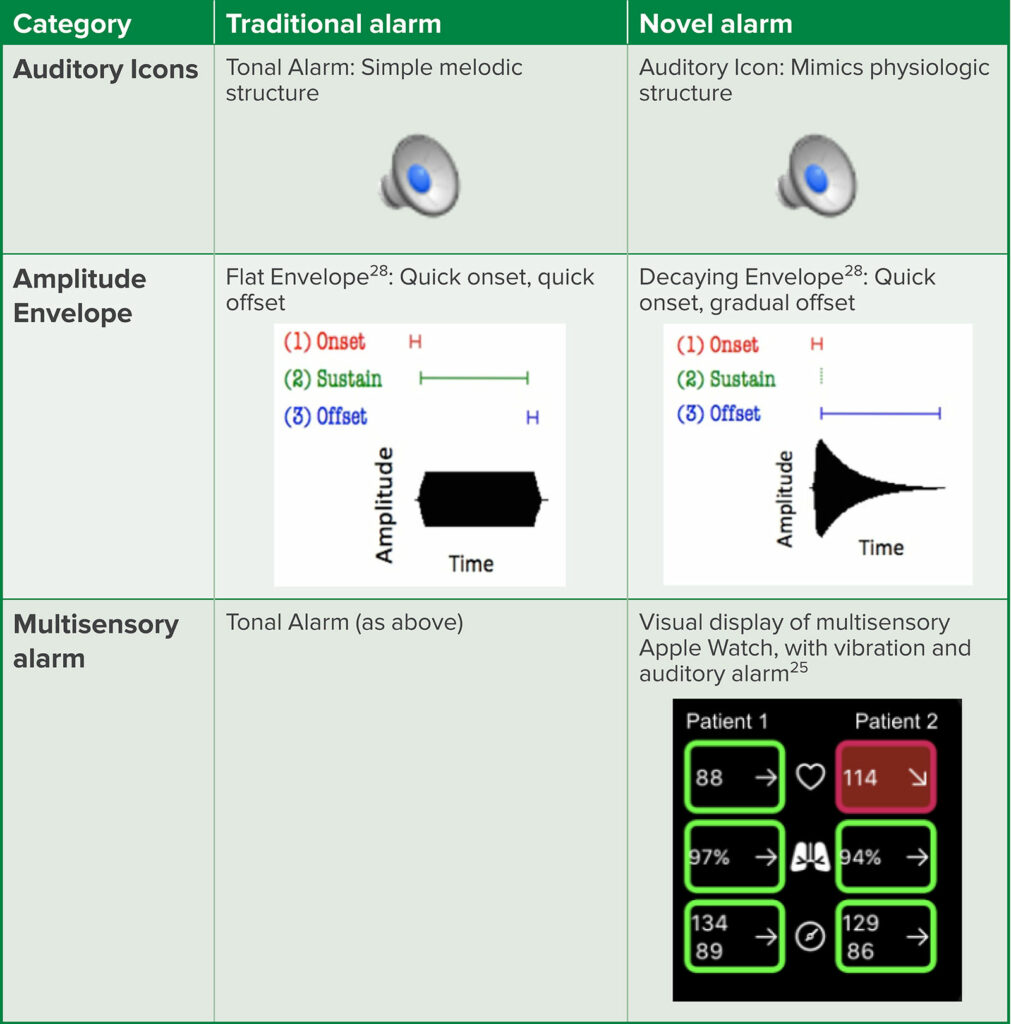
In 2006, the International electrotechnical commission (IEC) established an international standard for medical alarms 60601-1-8.15 However, alarms that abided by the IEC 60601-1-8 were difficult to learn and distinguish from concurrent alarms, as they used the same melodic structure, offering little individualizing detail between simultaneous alarms.16,17 As a result, a group of researchers created auditory icons as an alternative to the standard auditory alarms. Auditory icons mimic and/or represent the parameter that they are monitoring. For example, instead of the monotone beeping of a standard heart rate monitor, an auditory icon sounds like the “lub-dub” of a heartbeat (Table 1, additional IEC icons available for listening). These auditory icons were found to be easier to learn and more localizable than the traditional alarms tested.18 During clinical simulations, participants performed better when using auditory icons, including the ability to discriminate between simultaneous alarms and to identify alarm type.19 As a result of this strong supporting evidence, the IEC updated the 60601-1-8 in 2020 to include auditory icons as a supported medical auditory alarm.20 By incorporating auditory icons, alarm systems can optimize their notification designs in an evidence-based manner.
Table 1: Comparison of Traditional vs Novel Alarm Design.
In addition to alarms being difficult to discriminate, annoyance with the alarm sound itself has also been documented as a contributor to alarm fatigue in clinicians.21 Amplitude envelope describes the “structure” of a sound—where a flat envelope (that of a typical alarm) would have a quick onset and offset, a decaying envelope (such as the noise of clinking wine glasses) has a quick onset, followed by a gradual alarm decline (Table 1). The literature has shown that using a decaying amplitude envelope significantly reduces alarm annoyance without interfering with learning or performance—while also preserving an alarm’s melodic and rhythmic structure.22,23
Even simpler than re-engineering the auditory alarm structure, decreasing the volume at which an alarm is delivered has shown great benefits. At baseline, hospitals are noted to regularly exceed the World Health Organization’s recommendations for the clinical environment volume; however, alarms delivered at lower volumes may still elicit similar accuracy of alarm identification. One study found that participant performance in interpreting and responding to patient crises had a minimal difference when an alarm was delivered at a volume 11 dB below the background noise, compared with the typical 4 dB above background noise.24 Furthermore, devices, such as the Dynamic Alarm Systems for Hospitals, or D.A.S.H., have been developed and patented to regulate alarm volume based on the surrounding noise level.25,26 These systems provide important benefits to improve the auditory environment’s saturation with unnecessarily loud alarms.
Traditionally, medical alarms have relied primarily on the auditory sense, with partial notification through visual stimuli, such as a monitor. Multisensory alarms provide alerts using different senses, such as sound, light, and vibration, making them more noticeable in a busy operating room environment. Using multiple senses allows clinicians to respond to changes in a patient’s condition more rapidly and take appropriate action, improving patient safety and outcomes. Multisensory alarms also provide the opportunity to use wearable notification systems, such as an ankle band or smart watch (Table 1). When combining tactile (similar to vibration), visual and auditory stimuli into a wearable smart watch, undergraduate participants showed better accuracy, reaction time, and decreased mental workload in feasibility studies.27 Studies are currently underway with clinical end-users to confirm the workflow and performance benefit. Based on these and more studies, integration of multisensory alarm devices is feasible and may relieve the auditory burden of the medical environment and increase the overall quality of care and patient safety.
Research and engineering teams dedicated to the modernization and innovation of medical alarms through auditory icons, adjustments to alarm character, and use of multisensory devices are crucial contributors to the prevention of alarm fatigue.
CONCLUSION
Anesthesia professionals play a critical role in monitoring a patient’s vital signs and adjusting the anesthetic care as needed to ensure the patient remains in a safe and stable condition. They are also trained to respond quickly to medical emergencies that may arise during a procedure. Both roles require medical alarms to be safe and effective. This constant vigilance is essential to ensuring the best possible outcomes for patients undergoing medical procedures, making alarm design and optimization critical.
Patients in all medical settings rely on clinicians to care for and react to all their medical needs. Currently, the demanding workplace environment challenges staff with suboptimal alarm technology, contributing to alarm fatigue and burnout. By focusing on patient and provider safety, clinical workflow, and alarm technology, researchers, and policy makers can transform the medical alarm realm into one that is evidence-based and personnel-focused.
REFERENCES
- Nasri BN, Mitchell JD, Jackson C, et al. Distractions in the operating room: a survey of the healthcare team. Surg Endosc. 2022;1–10. PMID: 36070145
- Ruskin KJ, Bliss JP. Alarm fatigue and patient safety. APSF Newsletter. 2019;34(1). https://www.apsf.org/article/alarm-fatigue-and-patient-safety/. Accessed March 17, 2023.
- Sendelbach S, Funk M. Alarm fatigue: a patient safety concern. AACN Adv Crit Care. 2013;24:378–386. PMID: 24153215
- Winters BD, Cvach MM, Bonafide CP, et al. Technological distractions (Part 2): a summary of approaches to manage clinical alarms with intent to reduce alarm fatigue. Crit Care Med. 2018;4:130–137. PMID: 29112077
- Siebig S, Kuhls S, Imhoff M, et al. Intensive care unit alarms—how many do we need? Crit Care Med. 2010;38:451–456. PMID: 20016379
- Bonafide CP, Localio AR, Holmes JH, et al. Video analysis of factors associated with response time to physiologic monitor alarms in a children’s hospital. JAMA Pediatr. 2017;171:524. PMID: 28394995
- Schondelmeyer AC, Brady PW, Goel VV, et al. Physiologic monitor alarm rates at 5 children’s hospitals. J Hosp Med. 2018;13:396–398. PMID: 29694462
- Deb S, Claudio D. Alarm fatigue and its influence on staff performance. IIE Trans Healthc Syst Eng. 2015;5:183–196. doi:10.1080/19488300.2015.1062065
- The Joint Commission. (2014–2022). National patient safety goals. The Joint Commission. https://www.jointcommission.org/standards/national-patient-safety-goals/. Accessed February 21, 2023.
- Perioperative Patient Safety Priorities—Anesthesia Patient Safety Foundation. https://www.apsf.org/patient-safety-priorities/. Accessed March 14, 2023.
- ECRI Institute. Top 10 health technology hazards report. 2012–2020. https://www.ecri.org/landing-2020-top-ten-health-technology-hazards. Accessed February 21, 2023.
- Sowan AK, Gomez TM, Tarriela AF, et al. Changes in default alarm settings and standard in-service are insufficient to improve alarm fatigue in an intensive care unit: a pilot project. JMIR Hum Factors. 2016;3:e1. PMID: 27036170
- Shanmugham M, Strawderman L, Babski-Reeves K, Bian L. Alarm-related workload in default and modified alarm settings and the relationship between alarm workload, alarm response rate, and care provider experience: quantification and comparison study. JMIR Hum Factors. 2018;5:e11704. PMID: 30355550
- Ruppel H, De Vaux L, Cooper D, et al. Testing physiologic monitor alarm customization software to reduce alarm rates and improve nurses’ experience of alarms in a medical intensive care unit. Cortegiani A, ed. PLoS ONE. 2018;13:e0205901. PMID: 30335824
- International Electrotechnical Commission (IEC), ed. Medical electrical equipment—part 1–8: general requirements for basic safety and essential performance – collateral standard: general requirements, tests and guidance for alarm systems in medical electrical equipment and medical electrical systems. 2.1.; 2012. https://webstore.iec.ch/publication/2599. Accessed February 21, 2023.
- Sanderson PM, Wee A, Lacherez P. Learnability and discriminability of melodic medical equipment alarms. Anaesthesia. 2006;61:142–147. PMID: 16430567
- Edworthy J, Page R, Hibbard A, et al. Learning three sets of alarms for the same medical functions: a perspective on the difficulty of learning alarms specified in an international standard. Appl Ergon. 2014;45:1291–1296. PMID: 24209498
- Edworthy J, Hellier E, Titchener K, et al. Heterogeneity in auditory alarm sets makes them easier to learn. Int J Ind Ergon. 2011;41:136–146. doi:10.1016/j.ergon.2010.12.004
- Edworthy JR, Parker CJ, Martin EV. Discriminating between simultaneous audible alarms is easier with auditory icons. Appl Ergon. 2022;99:103609. PMID: 34700191
- International Electrotechnical Commission (IEC), ed. Medical electrical equipment—part 1–8: general requirements for basic safety and essential performance—collateral standard: general requirements, tests and guidance for alarm systems in medical electrical equipment and medical electrical systems. 2.2.; 2020. https://webstore.iec.ch/publication/2599. Accessed February 21, 2023.
- Edworthy J, Hellier E. Fewer but better auditory alarms will improve patient safety. Qual Saf Health Care. 2005;14:212–215. PMID: 15933320
- Sreetharan S, Schlesinger JJ, Schutz M. Decaying amplitude envelopes reduce alarm annoyance: exploring new approaches to improving auditory interfaces. Appl Ergon. 2021;96:103432. PMID: 34120000
- Foley L, Schlesinger JJ, Schutz M. Improving detectability of auditory interfaces for medical alarms through temporal variation in amplitude envelope. Br J Anaesth. 2023; 130:351-359. PMID: 36658020
- Schlesinger JJ, Baum Miller SH, Nash K, et al. Acoustic features of auditory medical alarms—an experimental study of alarm volume. J Acoust Soc Am. 2018;143:3688. PMID: 29960450
- Greer JM, Burdick KJ, Chowdhury AR, Schlesinger JJ. Dynamic Alarm Systems for Hospitals (D.A.S.H.). Ergon Des Q Hum Factors Appl. 2018;26:14–19. doi:10.1177/
1064804618769186 - Schlesinger JJ, Garcia A, Mitchell V, Turley F. Dynamic alarm system for reducing alarm fatigue. U.S. Patent No. 9,870,678. January 16, 2018.
- Burdick KJ, Gupta M, Sangari A, Schlesinger JJ. Improved patient monitoring with a novel multisensory smartwatch application. J Med Syst. 2022;46:83. PMID: 36261739
- Sreetharan,S, Schlesinger JJ, Schutz M. Designing effective auditory interfaces: exploring the role of amplitude envelope. Proceedings of the ICMPC15/ESCOM10, Graz, Austria. 2018;23–28. https://maplelab.net/wp-content/uploads/2018/12/Sreetharan-2018.pdf. Accessed February 21, 2023.


Leave a Reply
You must be logged in to post a comment.