Author: Michael Vlessides
Anesthesiology News
Adherence to a data-driven maximum surgical blood order schedule (MSBOS) for open and radical prostatectomies can help reduce unnecessary preoperative blood orders and procedure-related costs.
To help determine the efficacy of the MSBOS in potentially reducing preoperative blood orders and associated costs for the two procedures, Visagie and her colleagues compared data from pre- and post-MSBOS periods. Their data review comprised 4,903 patients who underwent radical prostatectomy (2,584 open; 2,319 robotic) at the institution between 2010 and 2016.
Patients were categorized by type of procedure and relevant time period, either pre-MSBOS (2010-2011) or post-MSBOS (2013-2016). Those presenting in 2012—the MSBOS transition period—were excluded from the analysis. Several factors were quantified, including the frequency of preoperative blood orders (type and crossmatch 2 units); compliance with MSBOS guidelines; and cost differences between the two study periods.
Blood Orders Markedly Change
At the 2019 annual meeting of the International Anesthesia Research Society (abstract E31), Visagie reported that robotic prostatectomy became much more popular over the course of the study, increasing from 13% of all radical prostatectomies in 2010 to 56% in 2016.
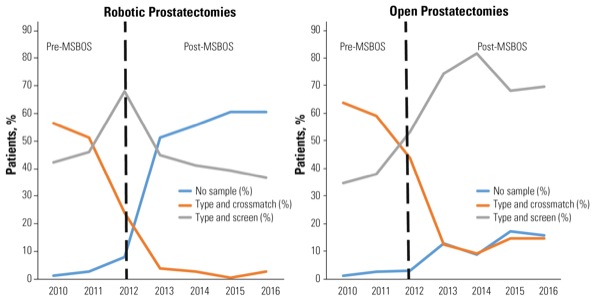
The analysis also found that after implementation of the MSBOS, preoperative blood orders changed markedly. Indeed, in robotic prostatectomy, orders changed from type and crossmatched with 2 units saved (53.1%) to no sample (56.3%; Figure).
“If you look at the pre-MSBOS period, we were ordering ‘type and crossmatch 2 units’ for robotic procedures, which is not ideal since these procedures are rarely or never transfused,” explained Visagie, who worked under the tutelage of Steven M. Frank, MD, the medical director of the institution’s Bloodless Medicine and Surgery Program.
In open procedures, on the other hand, orders changed from type and crossmatch 2 units (61.6%) to type and screen (74.6%).
Although compliance with the MSBOS guidelines is far from perfect, the researchers were nevertheless encouraged by their results to date. “At our institution, 90% of the blood is ordered by residents,” Visagie noted. “This is likely because residents want to play it safe and have something ready. It makes sense for them, but it’s not the best situation from an efficiency standpoint.”
Adherence to the MSBOS also resulted in significant cost savings. Indeed, in open radical prostatectomy, the average preoperative blood order cost per case fell from $47.31 to $35.36. Similarly, per-case blood order costs for robotic procedures fell from $45.89 pre-MSBOS to $17.21 after implementation.
Other institutions looking to implement similar programs can begin with an MSBOS published by the researchers in 2013 (Anesthesiology 2013;118[6]:1286-1297). Yet as Visagie noted, using data from an institutional anesthesia information management system is even better.
“I think it’s a great starting point if they have data available,” she told Anesthesiology News.
“Then comes education,” she continued, “because after you analyze your performance, you need to educate providers. For example, for radical prostatectomies we educated people that it’s definitely not ideal to be ordering a type and crossmatch.
“You also need to know who is ordering the blood at your institution,” she said. “For us it was the residents, and that’s why we directed our educational efforts at them. And since we get new residents every year, the educational process is continual. It’s not something you do one time only.”
Prostatectomies a Good Start
For Zeev N. Kain, MD, MBA, the Chancellor’s Professor at the University of California, Irvine, and president of the American College of Perioperative Medicine, the study helped highlight the importance of value-based care in the perioperative setting. “It makes total sense to me. The excessive ordering of lab test results always leads to more blood orders and erroneous conclusions and treatments.
“So when we build our perioperative surgical home models and enhanced recovery models, the first step is to look at all the tests we’re ordering and determine what we’re going to do with those results,” said Dr. Kain, who is a member of the editorial advisory board of Anesthesiology News. “It’s great that these researchers started with radical prostatectomy, but it really needs to be done with every type of surgery and every type of test.
“So this is a good program that uses the same logic we’ve been trying to incorporate into perioperative value-based care for the past five years,” Dr. Kain added. “It’s got a different name, but the conceptual framework is the same.”


Leave a Reply
You must be logged in to post a comment.