Anesthesiology News
Department of Anesthesiology
Yale School of Medicine
New Haven, Connecticut
Department of Surgery
Yale School of Medicine
New Haven, Connecticut
VA Connecticut Healthcare System
Department of Anesthesiology
Yale School of Medicine
New Haven, Connecticut
Introduction
With increasing frequency we encounter surgical patients with histories of chronic pain and/or opiate use disorder. Providing these patients with optimal perioperative pain control presents us with complex issues that require a fresh appraisal of our anesthetic approach.1 The literature suggests that the anesthetic ketamine, at subanesthetic doses, is an efficacious treatment for chronic pain syndromes, especially those that are neuropathic in nature.2 As a derivative of phenylpiperidine, it is structurally similar but safer for clinical use than phencyclidine, which has been shown to cause psychosis and agitation.2 Although ketamine has multiple sites of action, its principal mechanism, which confers strong analgesic capability, is inhibition of the N-methyl-d-aspartate (NMDA) receptor. The NMDA receptor is upregulated in chronic pain states at the dorsal horn synapses, leading to central sensitization, a phenomenon implicated in the development of pain from an acute process to a chronic state.3
Antagonism of NMDA receptors may reduce the generation of spontaneous pain, hyperalgesia, and allodynia resulting from central sensitization.4 Numerous studies have been conducted on the long-term effects of ketamine administration for patients in outpatient settings, and for hospitalized patients with acute pain. However, there is a paucity of literature specifically addressing the use of ketamine in the perioperative period and its potential for providing significant relief of chronic neuropathic pain in addition to alleviation of acute pain while decreasing opioid usage.5
Adequate intraoperative management of pain is vital because intractable pain following surgery may lead to the development of chronic pain.6 Development of a new pain generator during the perioperative period is particularly undesirable in patients with preexisting chronic pain states. In this case report, we describe the care for a patient with longstanding chronic neuropathic pain of the upper and lower extremities undergoing a substantial ventral herniorrhaphy. This patient received intraoperative ketamine and experienced significant pain relief of the upper- and lower-extremity neuropathy following surgery. This led to the initiation of a postoperative ketamine infusion that reduced opiate requirements, while also providing long-term post-discharge pain reduction. We advocate the use of perioperative ketamine not only for acute pain relief following surgery, but also for alleviation of preexisting neuropathic pain. The patient has provided written consent to publish this case report.
Materials and Methods
A 66-year-old man, with a body mass index of 34.5 kg/m2 and a past medical history of hypertension, hyperlipidemia, chronic obstructive pulmonary disease, obstructive sleep apnea compliant on nightly bilevel positive airway pressure, lumbar spine compression fracture, rheumatoid arthritis, osteoarthritis, past alcohol dependence and a previous ventral hernia repair, presented for explantation of a ventral mesh after developing a seroma and subsequent wound dehiscence of skin overlying the mesh. Eight years prior to this procedure, he developed alcoholic peripheral neuropathy with pain scored at 8/10 in his lower extremities. His medications for chronic pain included gabapentin 800 mg three times daily for neuropathy, etanercept (Enbrel, Immunex) for rheumatoid arthritis, and meloxicam. He had been hospitalized for an opioid overdose 1 year prior to the surgical procedure discussed, and since that hospitalization, has not been prescribed opioids. Additionally, the patient was concerned about opiate usage in the perioperative period.
On the day of surgery, the patient reported his “usual” stocking-glove paresthesia and allodynia with a pain score of 8/10. Acetaminophen 1 g was administered preoperatively. Using a sterile technique, an epidural was placed with a 17-gauge needle at the T10-T11 level, and a patient-controlled epidural analgesia pump was set up with bupivacaine 0.0625% and hydromorphone 10 mcg/mL; 8 cc continuous, 3 cc demand dose, and a lockout interval of 20 minutes. General anesthesia was induced with propofol, ketamine, and fentanyl, and an endotracheal tube was placed.
Intraoperatively, the patient was maintained on sevoflurane and hourly ketamine boluses. He received a total of 50 mg of ketamine during an operating time of 3 hours, therefore averaging 0.17 mg/kg per hour of ketamine. The patient had no intraoperative complications.
Postoperatively, the patient received acetaminophen 1 g every 6 hours in addition to his preoperative gabapentin dose. On postoperative day 0, he reported a pain score of 3/10 in his upper extremities, reduced from 8/10 prior to the procedure. On postoperative day 1, an IV ketamine infusion was started at a dose of 0.3 mg/kg per hour and subsequently, because of visual hallucinations, was titrated down to 0.2 mg/kg per hour. At that time, the patient reported improvement in his upper-extremity neuropathy with a pain score of 0/10. On postoperative day 3, the ketamine infusion and epidural were discontinued. A follow-up telephone interview on postoperative day 12 found that the patient had 0/10 pain in the upper extremities and 3-4/10 pain in his lower extremities while the pain medications were unchanged from the preoperative regimen.
Discussion
First introduced in the 1960s, ketamine possesses unique pharmacologic properties and has a wide spectrum of clinical application in the medical field. However, it is encumbered by a reputation for recreational use. Many providers hesitate to administer ketamine and some patients are unsure about accepting ketamine as a therapeutic intervention. Nevertheless, situations in which ketamine is quite useful are numerous and diverse. Some examples of this include ketamine as an induction agent in patients with severe hypotension, in patients with reactive airway disease, in children with congenital heart disease with right-to-left shunts, in burn victims undergoing dressing changes, as a sedative or analgesic in critical care, in peripheral nerve blocks, for electroconvulsive therapy, and even as a treatment to reduce suicidal ideation.7The use of ketamine is expanding into the realm of chronic pain, with evidence in the literature describing both an opioid-sparing effect and improved overall quality of pain control compared with opioid therapy.
The chronic pain patient population poses many challenges in the perioperative period. Special attention must be given to intraoperative pain management because inadequate pain control may lead to creation of a new source of chronic pain.8 Postoperative pain management is also of great importance, especially in this population, as many chronic pain patients may have developed tolerance to opioids. Even more dire is the risk for opioid use disorder relapse from exposure to peri- and postoperative opioids.
Ketamine is a superlative choice for intra- and postoperative analgesia in the chronic pain population, as it opposes the phenomenon of central sensitization and prevents development of persistent pain. Ketamine has also been cited as useful in preventing severe hyperalgesia states from repeated administration of large doses of opioids following surgery. Relapse of opioid use disorder is a real concern in these patients following surgery, when acute and chronic pain states may exhibit synergism and necessitate increasing doses of opioids.
The patient in the case described had a history of chronic neuropathic pain and prior opioid use disorder. Accordingly, his pain management plan was an appropriately opioid-sparing and multimodal technique that included ketamine. Interestingly, long-lasting effects were observed in his chronic neuropathic pain. His case draws attention to the potential of perioperative pain management using ketamine infusion, having far-reaching effects postoperatively. This care plan exemplifies the potential benefit that anesthesiologists can have in opiate use reduction efforts.9Importantly, both the patient and the surgical team were highly satisfied with the additional benefit of chronic pain reduction in the perioperative period, an unexpected and welcome deviation from their expectations.
After this index case, several of our surgical colleagues made requests for the use of ketamine infusions for their chronic pain surgical patients. These patients all benefited in a similar manner as the case discussed. In addition, several patients with chronic pain and opioid use disorder undergoing joint replacement have benefited from the use of multiday ketamine infusions. The incorporation of ketamine infusions in our perioperative pain management plan is fast becoming our standard practice.
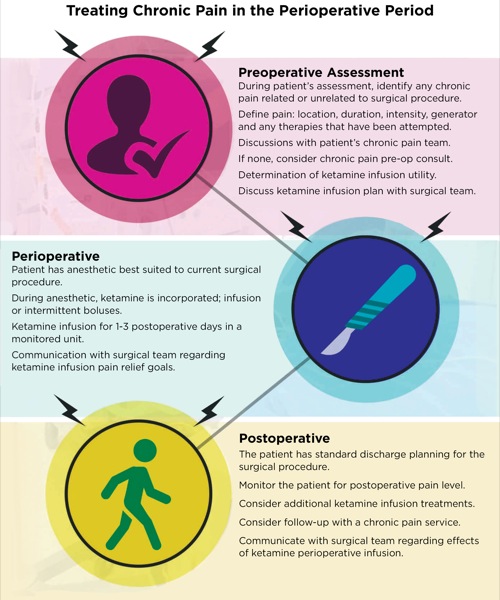
The therapeutic intervention described here fits seamlessly into the concept of the perioperative surgical home, which features integrated pain management as a cornerstone for patient recovery and satisfaction.10 To illustrate this perioperative practice strategy, we developed an infographic (Figure) for a proposed protocol to screen patients who would be suitable for perioperative ketamine infusions, provide a framework for intraoperative management, and suggest coordination with pain management post-discharge for follow-up. We hope to publish further research on the efficacy of this protocol in successfully treating pain in opioid-dependent and chronic pain patients undergoing surgery.
Disclaimer: The views expressed are solely those of the authors and do not reflect the official policy or position of the West Haven Veterans Affairs Hospital, or the US Veterans Health Administration.
References
- Center for Behavioral Health Statistics and Quality (CBHSQ). 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016.
- Maher D, Chen L, Mao J. Intravenous ketamine infusions for neuropathic pain management: a promising therapy in need of optimization. Anesth Analg. 2017;124(2):661-674.
- Niesters M, Martini C, Dahan A. Ketamine for chronic pain: risks and benefits. Br J Clin Pharmacol. 2013;77(2):357-367.
- Subrananiam K, Subramaniam B, Steinbrook R. Ketamine as an adjuvant analgesic to opioids: a quantitative and qualitative systematic review. Anesth Analg. 2004;99(2):482-495.
- Kurdi M, Theerth K, Deva R. Ketamine: current applications in anesthesia, pain, and critical care. Anesth Essays Res. 2014;8(3):283-290.
- Lavand’homme P. The progression from acute to chronic pain. Curr Opin Anesthesiol. 2011;24(5):545-550.
- Hocking G, Cousins M. Ketamine in chronic pain management: an evidence-based review. Anesth Analg. 2004;97(6):1730-1739.
- Niesters M, Martini C, Dahan A. Ketamine for chronic pain: risks and benefits. Br J Clin Pharmacol. 2014;77(2):357-367.
- Clark D, Schumacher M. America’s opioid epidemic: supply and demand considerations. Anesth Analg. 2017;125(5):1667-1674.
- Kash B, Zhang Y, Cline K, et al. The perioperative surgical home (PSH): a comprehensive review of US and non-US studies shows predominantly positive quality and cost outcomes. Milbank Q. 2014;92(4):796-821.


Leave a Reply
You must be logged in to post a comment.