Pract Pain Manag. 2021;21(4).
Treatment adherence strategies, including motivational interviewing and case vignettes.
Furthermore, approximately half of the medications that are filled result in inappropriate administration of the wrong dose, frequency, or duration. This translates into significant US healthcare costs. Barriers to medication adherence include increased age, impaired cognition related to disease, commitment to therapy selected, substance abuse, mental health disorders, drug costs, and much more.¹˒²
Medication Adherence in Patients with Chronic Pain
An estimated 20.4% of adults in the United States reported chronic pain in 2016. Chronic pain contributes to increased healthcare costs and often results in decreased productivity. Chronic pain is a common reason for adults to seek medical care and attention. Chronic pain can contribute to limitations in daily activities, reduced mobility, decreased quality of life, opioid dependence, anxiety, or depression.³ Chronic pain management may consist of multimodal treatment approaches, which can contribute to medication nonadherence. Multimodal treatment approaches use multiple types of pain medications for pain management. Complications of nonadherence to chronic pain regimens include adverse drug reactions, undertreated pain, and medication use disorders.
Medication Adherence Studies
A systematic review evaluated chronic, non-malignant pain and medication nonadherence. The review included a total of 25 articles. The studies used a variety of methods to report adherence such as self-reporting, urine screening, structured interview, and electronic monitoring. Nonadherence ranged from 8% to 62%. Categories identified as determinants for nonadherence included socio-economic, healthcare team, condition-related, therapy-related, patient-related pain severity, polymedication, type of medication, dosing frequency, and caregiver-patient relationships.⁴
A cross-sectional study was conducted with a 37-item, self-administered questionnaire among 100 patients aged 65 years or greater that included a direct question about adherence to prescribed analgesics. Around 57% of patients answered that they did not follow the medication instructions exactly as prescribed.⁵
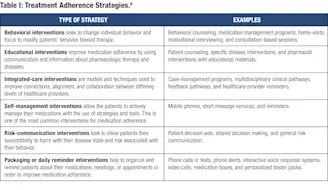
Medication Adherence Strategies
There are multiple strategies already identified to improve medication adherence.A review assesseddifferent interventional areas to increase medication adherence. The areas encompassed behavioral interventions,educational interventions, integrated-care, self-management,risk communication, and packaging or daily reminders. These areas all have many different and unique methods of developing better medication adherence. Examples of these techniques are listed below by category in Table I.⁶
See also, PPM’s Clinician Guide on drug monitoring and medication adherence.
Motivational Interviewing for Treatment Adherence
Motivational interviewing is a counseling method that involves the use of four guiding principles to increase patient motivation and change behavior. These principles are represented by the acronym RULE, which stands for:
-
resist the righting reflex
-
understand the patient’s motivations
-
listen with empathy
-
empower the patient⁷
The Substance Abuse and Mental Health Services Administration published a series containing an overview centered on motivational interviewing and techniques.⁸
A two-arm, cluster randomized trial evaluated the effectiveness of motivational interviewing in improving medication adherence for older patients being treated by polypharmacy. Participants had a chronic disease and were older than 65 years of age. Polypharmacy was defined as taking greater than or equal to 5 medications or greater than or equal to 12 daily doses for at least 6 months. Scheduled visits were at baseline, at 15 to 20 days in the patient’s home, at 3 months in a healthcare setting, and at 6 months in the patient’s home. Office visits averaged about 15 minutes in duration and home visits averaged 45 to 60 minutes in duration. Effectiveness of motivational interviewing was assessed by videotaping participants in a simulated encounter.
Two evaluators independently scored the interviews using the CICAA and EVEM tools. The CICAA is a rating scale created to evaluate patient-centered generic skills. The EVEM was designed to evaluate specific motivational interviewing skills. Medication adherence was calculated using the formula (number of tablets consumed/total number of tablets) x 100. Adherence was described as average adherence percentage greater than 80% and less than 110%. The study randomized 154 patients and ended with 147 patients, 81 in the control group and 66 in the experimental group. Baseline adherence was 39.3% in the control group and 47.1% in the experimental group. From the intention-to-treat analysis, the rate of adherence in the control group was 71.4% compared to 56% in the experimental group (P < 0.001). Along with motivational interviewing, other variables such as female gender and higher education levels improved medication adherence.⁷
A meta-analysis analyzed 17 studies, totaling 4,221 participants, focusing on adults with chronic diseases, which were defined as diseases with generally slow progression and long duration. The meta-analysis evaluated motivational interviewing characteristics and results on effect size. Pooled results showed that motivational interviewing had a positive effect on medication adherence as compared to usual care (P = 0.003). Coaching the interventionists and face-to-face delivery had a positive effect when compared to phone-based motivational interviewing. The analysis was not able to assess the effects for mean duration of motivational interviewing sessions or interventionist training.⁹
A prospective study assessed motivational interviewing in patients with diabetes mellitus or hypertension whofilled an angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker within a Medicare Advantage Plan. The intervention consisted of 6 motivational interviewing phone calls by pharmacy students, over 6 months. A summary of the interaction, barriers, and plans to achieve therapy goals were recorded after phone calls. Refill histories were assessed to calculate adherence rates, which were established as proportion of days covered (PDC). To calculate PDC, the total days’ supply of angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker was divided by the 180 days in the study.
Results showed that patients who received more than 2 follow-up phone calls were more likely to become adherent (OR: 1.53; 95% [CI] = 1.02 to 2.28, P = 0.009) and were less likely to discontinue therapy (OR: 0.29; 95% CI= 0.15 to 0.54; P < 0.001) when compared to patients who received no motivational interviewing. Adherence was compared between baseline and post-intervention. Patients with heart failure or depression were statistically less likely to adhere to medication.¹⁰
Practical Takeaways
Medication adherence will always be a problem in the patient population. Perfect adherence is desired, but highly unrealistic. Clinicians need to continually assess for medication adherence and identify barriers. Pharmacists and pharmacy students have been trained and exposed to numerous strategies for medication adherence, including motivational interviewing, and they can assist with or perform adherence assessments and identify barriers.
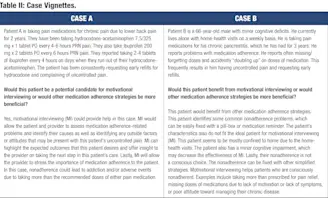
A variety of strategies are available to increase adherence. Motivational interviewing is one of many safe and effective techniques with evidence to support improved medication adherence. Patient characteristics, type of nonadherence, and needs should be considered when assessing the role of motivational interviewing to improve medication adherence.


Leave a Reply
You must be logged in to post a comment.