Author: Michael Vlessides
Anesthesiology News
Researchers may have uncovered a simple way to avoid potential unintended awareness during high-risk cardiac surgery.
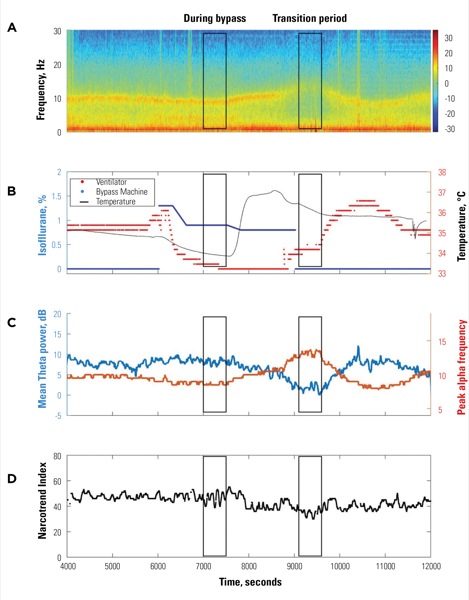
Their study found that EEG signatures similar to those seen during emergence—decreasing theta power with increasing alpha frequency—occur regularly during cardiac surgery. Paying close attention to these signals in the form of a spectrogram, the researchers found, may be a simple way to decrease the incidence of unintended awareness in this patient population.
“We know that during cardiac surgery the incidence of awareness is 10 times higher than it is during normal surgery,” said study co-investigator Heiko Kaiser, MD, an assistant professor in cardiac anesthesia at the institution.
Of note, the frontal EEG signature of a patient returning to consciousness during emergence at the end of surgery typically shows a concurrent loss of theta power and an increase in alpha frequency. Although this pattern can be easily observed in a spectrogram, it is currently unknown whether algorithms of depth-of-anesthesia monitors accurately reflect these spectral changes.
“In looking at the brain wave activity of patients undergoing cardiac surgery, we noticed there were EEG signatures similar to those of people who were intentionally waking up after surgery in the emergence period,” said Darren Hight, PhD, a postdoctoral researcher at the institution. “So we wanted to find out how often these patterns are occurring in our data set.”
The investigators sought to quantify changes in theta power and alpha frequency in a case study, determine whether the Narcotrend Index reflects the spectral changes observed, and estimate the occurrence of such EEG phenomena during cardiac surgery.
To do so, they recorded frontal bipolar EEG using a Narcotrend monitor (Narcotrend-Gruppe) in 1,072 patients undergoing cardiac surgery. In the first 300 patients, the researchers used a computational tool to create a spectrogram from spectra taken from two-second moving windows of EEG. The mean theta power (4-7 Hz) and peak alpha frequency (7-17 Hz) were also measured.
The ‘Signature’ of Awareness Is Noted
Presenting at the 2019 annual meeting of the International Anesthesia Research Society (abstract D113), the investigators noted that during the transition from cardiopulmonary bypass to ventilation in one exemplary case, mean theta power decreased from 7.8 to 1.9 dB while peak alpha frequency increased from 9.0 to 13.1 Hz. During this time, however, the mean Narcotrend Index value decreased from 46 to 35.
“We observed a basic signature where the alpha activity was increasing in frequency and the theta power was decreasing, which is the signature of someone waking up,” Dr. Hight explained. “And this was occurring at a particularly difficult time during surgery for the anesthetists, when you’re going from the bypass machine to the ventilator.”
In an interim analysis of the first 300 patients in the institution’s database, 284 patients had usable EEGs where the spectrogram was visually assessed. Of these, it was found that 52 patients (18%) showed a concurrent decrease in theta power and an increase in alpha frequency. Of note, the depth-of-anesthesia monitor only reflected these spectral changes in 15 of the 52 patients (29%).
“The overwhelming majority of these instances occur when the patient is separated from cardiopulmonary bypass,” Dr. Kaiser explained. “It’s not happening when you’re going on to bypass, and it’s not happening afterwards. It’s almost always right there.”
It was also found that alpha oscillation was temporarily absent over this transition period in 26 of the 52 patients (50%), suggesting thalamocortical depolarization.
“We don’t know if they actually were waking up or not, but the signal is certainly similar,” Dr. Hight said, “and it’s probably worth avoiding.”
Avoiding these concurrent changes in theta power and alpha frequency is the anesthesiologist’s challenge, one that the researchers said is not helped by current depth-of-anesthesia monitors. “The first thing to do is get away from an index number like the bispectral index or Narcotrend, and pay attention to the density spectral area of the EEG, where you can see the spectral changes much better,” Dr. Kaiser explained. “It gives you more information.”
As Dr. Hight explained, learning how to interpret the dense spectral array of the EEG is something any clinician can do, with enough practice. “It’s a simple pattern recognition,” he told Anesthesiology News. “It’s easy to see” (Figure).
“We think that if you look at a spectrogram properly, you can tell how deeply sedated the patient is, without looking at the specific index and number,” he added. “And you can also theoretically prevent awareness.”
The study’s results proved intriguing for Matthias Kreuzer, PhD, a researcher at the Technical University of Munich. “They show an occurring change in the spectral composition of the EEG power spectrum that may be an indicator for potential arousal during cardiac surgery, namely, a decrease in EEG theta-band power in combination with an increase in EEG alpha-band peak frequency.
“EEG-based monitoring systems may not correctly track these changes towards arousal, because these devices mainly focus on the higher and lower frequencies and the changes between high-frequency, low-amplitude activity during wakefulness and low-frequency, high-amplitude activity during anesthetic-induced unconsciousness,” Dr. Kreuzer continued. “The presented work highlights the importance of visually inspecting the density spectral arrays that can be displayed by most monitors and not exclusively relying on the ‘depth-of-anesthesia’ index.
“Anesthesiologists could use the described and easily identifiable change in the spectral composition to timely and correctly react to a changing level of general anesthesia,” he added. “Future research will have to show if potential arousal reactions only follow this theta and alpha pattern or, as it is in the case of anesthesia emergence, these arousals can have different trajectories.”


Leave a Reply
You must be logged in to post a comment.