Introduction
The awake anesthetic technique used during craniotomy has been demonstrated to provide adequate sedation to keep patients awake, comfortable, and responsive to commands. This technique facilitates cortical mapping and allows for greater extent of tumor resection. A review of our institution’s total costs for awake craniotomies was compared with data from all craniotomies in the state of Florida. We found awake craniotomies performed at our institution demonstrated significantly reduced length of stay (LOS) and lower costs when compared with all craniotomies performed in Florida. The awake anesthetic technique has proven to be a key component in maintaining cost-effective, value-based care.
The Technique
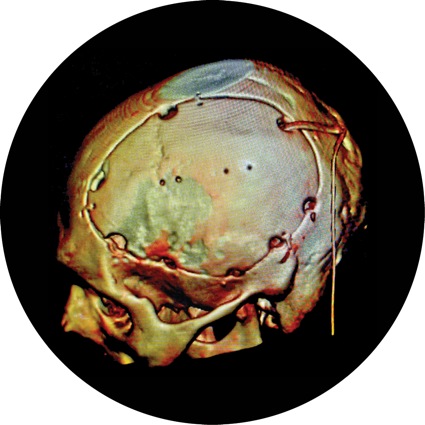
The awake anesthetic technique for craniotomy has become an increasingly popular method in which the surgeon, anesthesiologist, and patient work together during the procedure to achieve an optimal outcome for the patient. This method uses an anesthetic that provides the appropriate level of sedation to keep the patient awake, comfortable, and responsive to commands. The awake technique is preferred in order to facilitate cortical mapping,1 which is crucial when resecting tumors in the eloquent cortex.2
Previous studies have linked the awake anesthetic technique to lower neurologic complication rates, greater extent of tumor resection, and shorter hospital stays.3 It has been shown that although the awake anesthetic technique is linked to shorter hospital LOS, there is no difference in operating room time or ICU LOS.4 In our experience, over 75% of patients are discharged within 24 hours of awake craniotomy after maximum safe resection of tumors in eloquent regions of the brain.5
The risks of craniotomies performed using the awake technique include intraoperative seizures, respiratory arrest, nausea/vomiting, and patient intolerance.6 Initial anesthetic goals must include a thorough risk–benefit evaluation, proper patient education, and a discussion with the neurosurgeon and patient. Few papers have fully evaluated the cost savings associated with awake craniotomies, sparking a review at our institution, Moffitt Cancer Center, and comparing these with other craniotomies in the state of Florida.
Methods
Institutional review board approval for a retrospective review was obtained, and the requirement for written informed consent was waived. Seventy-four consecutive awake craniotomies from July 2013 to February 2015 were retrospectively reviewed for total costs. This was compared with state of Florida outcomes of 4,188 procedures performed between April 2015 and March 2016. These data were available on floridahealthfinder.gov under the procedure noted as “craniotomy.”
The awake craniotomy protocol at our institution begins with careful patient selection and preoperative assessment. Evaluation of the patient’s mental and physical status and medical history is critical. Patients with anxiety, altered mental status, obesity, severe obstructive sleep apnea, known difficult airways, or other significant neurologic and active respiratory problems should undergo a more extensive evaluation as to whether the awake craniotomy procedure is most appropriate. Upon arrival on the day of surgery, the procedure and expectations are explained to the patient.
Preoperatively, nausea prophylaxis and anxiolysis are prioritized with the administration of IV ondansetron, famotidine, and midazolam, as needed. In the operating room, a nasal cannula and standard American Society of Anesthesiologists monitors are placed. A dexmedetomidine infusion is initiated at 0.4 to 0.7 mcg/kg per hour; remifentanil (Ultiva, Mylan) infusion is started at 0.04 mcg/kg per minute. Both medications are titrated for patient comfort and hemodynamic stability. Boluses of dexmedetomidine are avoided to reduce the incidence of hypotension and bradycardia. Once adequate sedation is achieved, preparation is made for superficial scalp blocks, as described by Pinosky et al.7 Upon completion of the full scalp block, the neuromonitoring team places leads for monitoring somatosensory evoked potentials, and the scalp is prepped and draped following standard technique. Per surgeon request, 50 g of mannitol, 10 mg of dexamethasone, and 20 mg of furosemide are administered intravenously to improve surgical exposure.
A t test for linear regression was performed using institutional data on LOS, severity of illness, and risk for mortality compared with total costs. Severity of illness was defined as the extent of physiologic decompensation or organ system loss of function, and mortality risk was defined as the likelihood of death. Both values were determined by secondary diagnoses, age, and procedures performed. These assessments were graded as minor, moderate, major, or severe for the analysis as per the Health Care Financing Association’s 3M Health Information Systems All Patient Refined Diagnosis Related Groups.
All values were applied the Grubbs’ test for the extreme studentized deviate to identify and determine the significance of any outliers within the data set. One value (total cost, $132,486) was excluded from the statistical analysis after it was determined a largely significant outlier from the test for extreme studentized deviates (P<0.01).
Results
| Table. Cost Comparison of Craniotomies | ||
| Moffitt Cancer Center | State of Florida Hospitals | |
|---|---|---|
| Minimum cost | $35,255 | $78,260 |
| Maximum cost | $82,171 | $193,190 |
| Average length of stay | 2 days | 8.3 days |
| Costs for Moffitt Cancer Center are described as the lowest and highest values. Cost values for state of Florida hospitals are reported as 25th and 75th percentiles. | ||
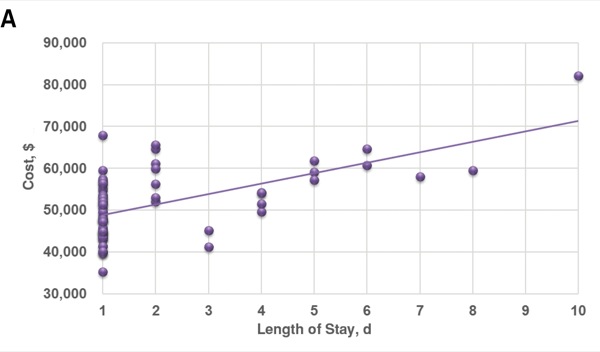
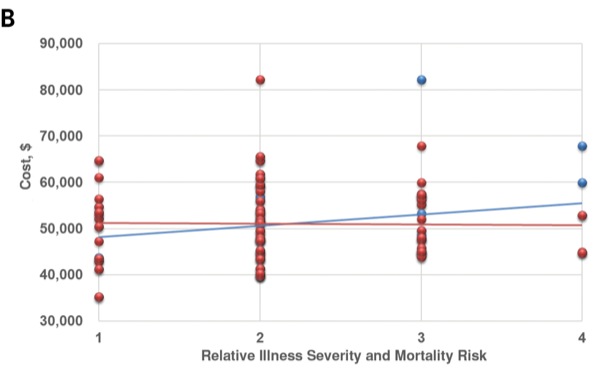
At our institution, the average total cost of craniotomies performed under sedation was $52,143. Total costs ranged from $35,255 to $82,171, with an average LOS of 2 days (Table). There was a significant line of regression with a nonzero slope for the association between LOS and total costs (P<0.01). A correlation coefficient of 0.59 was observed (Figure, Panel A). However, nonsignificant associations existed between total costs and illness severity (P=0.06) or mortality risk (P=0.88). Correlation coefficients of 0.21 and –0.02 were observed, respectively (Figure, Panel B). State of Florida outcomes found costs ranged from a 25th percentile of $78,260 to a 75th percentile of $193,190, with an average LOS of 8.3 days.
Discussion
Costs and LOS are significantly reduced when an awake anesthetic technique for craniotomy is used. Limitations of the state data include incomplete reporting to the Agency for Health Care Administration/Florida Center for Health Information and Transparency and the assumption that all reported craniotomies were performed under general anesthesia. Although the reduced costs can be attributed to decreased LOS, no significant association exists between total costs and illness severity or risk for mortality.
Cost is still an important outcome to be examined in the health care industry in order to maximize efficiency and value-based patient care. As the craniotomy procedure advances to include preoperative functional brain mapping and intraoperative magnetic resonance scanning, the awake anesthetic technique may offer a safe and low-cost solution.8
References
- De Benedictis A, Moritz-Gasser S, Duffau H. Awake mapping optimizes the extent of resection for low-grade gliomas in eloquent areas. Neurosurgery. 2010;66(6):1074-1084.
- Black PM, Ronner SF. Cortical mapping for defining the limits of tumor resection. Neurosurgery. 1987;20(6):914-919.
- Sacko O, Lauwers-Cances V, Brauge D, et al. Awake craniotomy vs surgery under general anesthesia for resection of supratentorial lesions. Neurosurgery. 2011;68(5):1192-1198.
- Peruzzi PP, Bergese SD, Viloria A, et al. A retrospective cohort-matched comparison of conscious sedation versus general anesthesia for supratentorial glioma resection. J Neurosurg. 2011;114(3):633-639.
- Groshev A, Padalia D, Patel S, et al. Clinical outcomes from maximum-safe resection of primary and metastatic brain tumors using awake craniotomy. Clin Neurol Neurosurg. 2017;157:25-30.
- Hervey-Jumper SL, Li J, Lau D, et al. Awake craniotomy to maximize glioma resection: methods and technical nuances over a 27-year period. J Neurosurg. 2015;123(2):325-339.
- Pinosky ML, Fishman RL, Reeves ST. The effect of bupivacaine skull block on the hemodynamic response to craniotomy. Anesth Analg. 1996;83(6):1256-1261.
- Burnand C, Sebastian J. Anaesthesia for awake craniotomy. Contin Educ Anaesth Crit Care Pain. 2014;14(1):6-11.


Leave a Reply
You must be logged in to post a comment.