Author: Michael Vlessides
Anesthesiology News
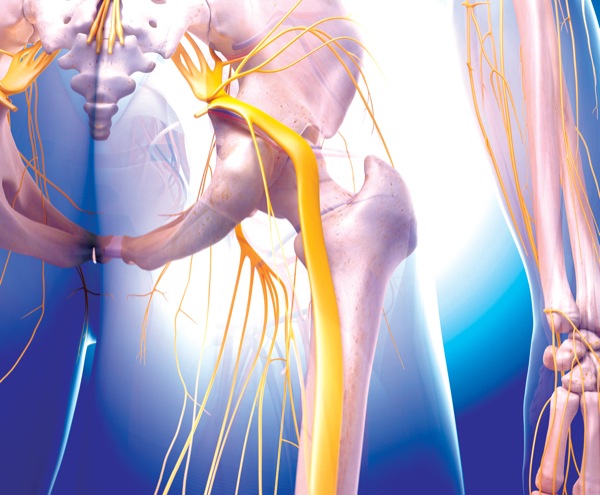
A novel continuous popliteal-sciatic nerve block using a location immediately distal to the sciatic nerve bifurcation and deep to the paraneural sheath appears to offer no postoperative analgesic advantage over the traditional technique. Catheter insertion above the sciatic bifurcation and superficial to the paraneural sheath has been used more commonly.
According to Jacklynn F. Sztain, MD, an assistant clinical professor of anesthesiology at the University of California, San Diego School of Medicine, new research is challenging the traditional approach to these blocks. “Recent data suggest that in single-injection blocks, depositing the local anesthetic relative to the paraneural sheath can influence the block’s efficacy. Moreover, subparaneural injections have been found to have faster onset and higher success rates than their supraparaneural counterparts.”
Dr. Sztain and her colleagues hypothesized that postoperative analgesia with continuous popliteal-sciatic nerve block after foot or ankle surgery would be improved if the perineural catheter tip is inserted deep to the paraneural sheath and immediately distal to the bifurcation between the tibial and common peroneal branches. The traditional approach is insertion superficial to the paraneural sheath proximal to the bifurcation.
Patients were excluded from the trial if they had any type of neuropathy in the surgical limb, a history of chronic opioid use, renal insufficiency, a body mass index greater than 40 kg/m2 or local anesthetic allergies, or were pregnant.
“For the proximal location, the catheter was inserted 6 to 7 cm proximal to the sciatic bifurcation,” Dr. Sztain explained. “For the distal approach, the Tuohy [needle] and catheter were inserted immediately distal to the sciatic nerve bifurcation, where the two branches are adjacent but distinct, between the perineurium and epineurium spaces.”
The trial’s primary end point was average pain, measured on a numerical rating scale (NRS) of 0 to 10, in the two hours before a data-collecting telephone call at noon the day after surgery. Secondary end points included maximum pain score during those same two hours, opioid consumption in the PACU and following hospital discharge, fluid leakage at the catheter insertion site, and perceived numbness in the foot and toes.
No Advantage Found
Presenting at the 2018 annual meeting of the American Society of Anesthesiologists (abstract A2276), Dr. Sztain reported no significant differences in pain scores. The average NRS score of patients with a catheter inserted at the proximal subparaneural location (n=31) was a median of 1.5 (10th, 25th-75th and 90th quartiles: 0.0, 0.0-3.5 and 7.0, respectively), compared with a median of 1.5 (quartiles: 0.0, 0.0-4.0 and 7.0) for their 32 counterparts who had the catheter inserted in the distal supraparaneural location (P=0.927).
The study also found no clinically meaningful or statistically significant differences between the treatment groups for any secondary end points (Table).
| Table. Findings for Secondary End Points | |||
| Proximal | Distal | P Value | |
|---|---|---|---|
| Catheter insertion time (minutes) | 4.5 (4.0-6.0) | 4.8 (4.0-7.6) | 0.408 |
| Postoperative lidocaine bolus, n (%) | 22 (71) | 21 (66) | 0.649 |
| Degree of foot numbness (0-10 scale) | 7.0 (4.0-8.5) | 7.0 (5.0-9.2) | 0.413 |
| Fluid leakage at catheter site, n (%) | 3 (10) | 4 (12) | 0.722 |
| Intraoperative/PACU opioid consumption (morphine equivalents) | 3.5 (1.5-4.0) | 3.1 (2.3-4.6) | 0.894 |
| PACU/postoperative day 1 opioid consumption (morphine equivalents) | 0.3 (0.0-1.0) | 0.0 (0.0-0.8) | 0.919 |
“So, our conclusion was that for subjects randomized to the two approaches who had a catheter inserted per protocol, there was no clinically relevant or statistically significant difference between the two groups with respect to any end point,” Dr. Sztain said.
“This trial found no evidence that continuous distal perineural sciatic nerve catheters provide any clinically relevant or statistically significant benefits compared to the traditional superficial proximal perineural catheter,” she added. “This is in contrast to what is found when you see single injections to the perineurium, distal to the bifurcation of the sciatic nerve.”
Session co-moderator Angela Selzer, MD, an assistant professor of anesthesiology at the University of Colorado School of Medicine, in Denver, questioned whether the study’s methodology considered the possibility of a negative finding. “When you have a negative study, oftentimes you think about whether you were adequately powered to find a significant difference. What type of difference were you looking for?”
“Our study was powered to find a difference in NRS pain scores of 2.5 between the two groups,” Dr. Sztain replied.
“I actually perform my single-shot blocks distally and my catheters proximally,” Dr. Selzer added. “So I’m happy that your findings support that part of my practice.”


Leave a Reply
You must be logged in to post a comment.