Assistant Professor of Anesthesiology and Biomedical Informatics
Vanderbilt University Medical Center
Nashville, Tennessee
One of the defining characteristics of our current era is the rapid advancement of technology, in which the miniaturization of electronic components has been married to increasing hardware interconnectivity to produce novel devices with revolutionary potential.
While smartphones and the interwebs have forever changed our world, the spread of tools such as video laryngoscopes has dramatically altered our clinical practice.1 This review explores emerging technological developments in anesthesiology, with a particular focus on the intersection of clinical informatics and the perioperative environment. The focus is on content from the 2017 annual meeting of the Society for Technology in Anesthesia (STA), which is available online at www.stahq.org.
Perioperative Big Data
In our interconnected world, in both the lay press and scientific literature, there has been increasing interest in Big Data. Big Data can be defined as data with high volume and high velocity and having a high degree of variety.2 Although it is debatable whether the information streams that we are currently generating in the perioperative arena qualify,3 it is certainly true that we produce large quantities of data related to surgical and anesthesia care on a daily basis. It is also clear that these data could be analyzed to produce insights that may improve patient care and, ultimately, perioperative outcomes. However, analyzing these data incorrectly could lead to nonreproducible research, erroneous conclusions, wasted resources, and potential patient harm. Although appropriate research methodology is necessary to avoid these pitfalls,4 understanding appropriate statistical approaches to these data is also crucial.
At the STA meeting, Timothy Houle, PhD, who serves as statistical editor of Anesthesiology, defined having Big Data as being able to “get coffee while waiting for [your analysis] to run,” and noted that many of the analyses in this area are performed from databases that are not designed explicitly to address a given hypothesis. This requires detailed, informed statistical modeling to isolate the effect of interest from confounders, reducing the sources of bias, and attempt to determine causality. Classic statistical approaches are ill-suited to these problems. This is because very large sample sizes, even very small differences between groups, can reach statistical significance (P<0.05) while those same differences are clinically inconsequential (ie, blood oxygen saturation level of 97% vs 98%). Best practices for perioperative Big Data analyses are obtaining expert input early, determining what a clinically significant effect size would be before performing an analysis and prospective registration of the statistical analysis plan.
Although these ideas may seem intangible compared with technologies that are typically associated with anesthesia, such as devices that directly attach to patients, they have a significant effect on perioperative care and drugs used daily by anesthesiologists. For instance, as Brian Bateman, MD, PhD, discussed, a large database study published in 2013 identified an association between the induction of labor and subsequent development of autism spectrum disorder,5 which was motivated by the relationship between oxytocin’s dual role in labor induction and social/cognitive function. This study was covered extensively in the lay press and generated significant concern from some patients. However, it was performed with a traditional epidemiological design and subject to spurious findings from residual confounding. A more detailed study design was performed, which included pregnancy conditions that are associated with the need to induce labor.6 The effect disappeared with the more appropriate study design for a perioperative Big Data analysis.
In addition to its applications in obstetric anesthesia, perioperative Big Data has a role to play in pain management. Although a large sample size can confound analyses if not properly managed, it can offer the ability to study rare events. For instance, postoperative opioid overdoses are relatively rare, with an incidence rate of just 0.1%, but has been increasing over time, with a trajectory parallel to the current opioid epidemic.7 By understanding risk factors for these adverse events, such as substance abuse history and patient demographics, high-risk patients can be identified and postoperative monitoring strategies deployed for this patient population. This approach of aligning insights from perioperative Big Data to monitoring devices more traditionally in the purview of anesthesiology has the potential to reduce rare but potentially fatal postoperative complications.
Quality Measurement
With the introduction of the American Recovery and Reinvestment Act of 2009 and the subsequent passage of the Medicare Access and CHIP Reauthorization Act of 2015, Big Data has begun to turn quality measurement programs into big financial effects for anesthesia practices. The fundamental driving force behind these pieces of legislation has been to improve the patient experience of care and the health of populations, all while reducing cost, which is known as the triple aim.8 This requires focused efforts on specific aspects of care, which in turn requires systems that are able to measure how that care is performed as well as changes in that care over time. Although all quality improvement is fundamentally local, technological developments have made it feasible for practices across the nation to define quality measures in the same manner and share data at a national level to facilitate benchmarking and regulatory reporting.9 This has necessitated the development of anesthesia quality measures and standards development for the practice of anesthesiology.
As a specialty, as the Anesthesia Quality Institute Practice Quality Improvement Committee Chair Emily Richardson, MD, n oted, anesthesiology has 3 technology tiers: granular clinical data from anesthesia information management systems (AIMS), gross clinical data from registries, and administrative data from claims and billing systems. These 3 tiers allow analyses of patient outcomes and risk factors, such as in the few short years that our anesthesia-specific registries have made it feasible to understand crucial perioperative outcomes, such as cardiac arrest.10While improvement of many of the core features of AIMS has been the focus of anesthesiologists for a number of years, the broadened scope of anesthesiologists as perioperative physicians has necessitated expansion of expertise to integration of anesthesia-specific systems into hospital-wide systems that support extraction of additional patient details. These details will allow for the development of risk-adjusted outcomes measures, which will be critical for understanding local areas for quality improvement and thus drive improvements in perioperative outcomes.
One of the central challenges to quality measurement is agreement of definitions, as Avery Tung, MD, discussed. When the same complication can be measured in different ways, the resultant incidence and risk factors can vary significantly. For instance, postoperative acute kidney injury in one patient population has been found to range between 7% and 37%, depending on whether the outcome was assessed by the National Surgical Quality Improvement Program or RIFLE (Risk, Injury, Failure, Loss of kidney function, and End stage kidney disease) criteria.11 This variability can be further complicated by the approach to documentation, of which interpretation of the sometimes blurry lines between clinical conditions can determine the categorization of an outcome. Further, analysis of the same patients using the same definition can lead to different categorization when performed by untrained clinicians.12 Having oversight by a formal committee structure with dedicated local data managers and trained clinicians can improve these definitions and the measurement process. Despite these challenges, attention to process can lead to improved outcomes, even if the improvements are incremental.
Noninvasive Respiratory Monitoring
The march of technology that has enabled the development of scalable quality measurement systems also has brought increasingly sophisticated patient monitoring approaches to the market. There has been a growing body of evidence supporting the technology behind the ExSpiron (Respiratory Motion) noninvasive minute ventilation monitor, which uses a radiolucent, printed-circuit electrode padset to measure differences in thoracic impedance. This permits the measurement of respiratory volume, which provides reliable measurement of tidal volume, respiratory rate, and minute ventilation.13 This approach has been demonstrated to detect respiratory compromise well before pulse oximetry devices alert,14 and may be helpful in identifying clinical deterioration in lower acuity settings, such as the postoperative floor. Additionally, this technology has shown potential for identifying patients post-extubation who are at risk for subsequent decompensation,15 such as in the PACU, and as such might be triaged for higher acuity postoperative care. This stratification approach may pair well with and be enhanced by incorporating patient-specific risk factors, identified in population-based studies through the Big Data approaches discussed above.
Simulation Technology
Of the new technologies presented, one of the boldest was a description of a novel approach to learning anatomy that has been developed at Case Western Reserve University in conjunction with Microsoft.16 The system utilizes the HoloLens, which is an augmented reality system that allows the wearer to interact with digital content, such as 3-D anatomic models. Actual patient MRI data were used to construct the current content. These models can be manipulated and explored, with layers of tissue added and removed to facilitate an interactive approach to learning anatomy. Additionally, the platform allows for learning at a distance, as instructors can join remotely. This type of interactive anatomic content also can be used for patient education. For instance, Stanford Children’s Health now includes animated, graphic models in their descriptions of surgical treatments offered,17 which leverage these same core technologies for improving content engagement and understanding.
Serious Gaming
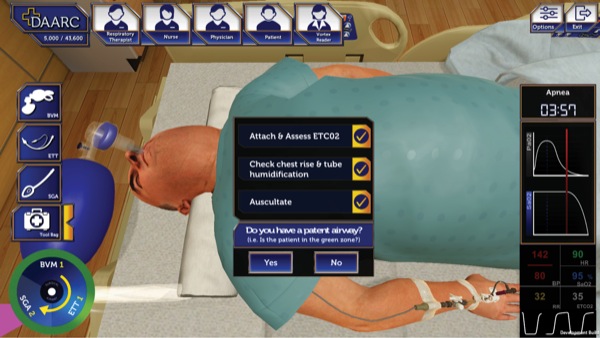
With simulation now well established in the armamentarium of clinical training, it is exciting to see several areas where technological advances have the potential to further revolutionize this approach to instruction. Serious gaming is related to simulation but with some key differences, as it is intended to both entertain as well as educate and change behavior. Unlike traditional simulation, this approach is much more easily scaled; once game development has been completed, users can interact with the material at a time and place of their convenience, and performance can be automatically scored without the need for instructor observation.18
This approach has been applied through the American Society of Anesthesiologists, Difficult Airway Algorithm and Rescue Cricothyrotomy (DAARC) game, developed through the Department of Veterans Affairs (Figures 1-3).19 The result is an application that permits a user to walk through multiple clinical scenarios, including attempted placement of supraglottic airway devices, endotracheal tubes, and surgical airways. This approach allows for practicing airway management outside the operating room, including failed and difficult airway scenarios. Further refinement of the application and validation of its use as an educational tool will be essential for determining its future role in our specialty.
Advances in Education
Although the advent of technology, such as serious gaming, is exciting, these approaches are not by themselves sufficient for training; thus, identifying the best strategies for combining online learning and traditional methods is necessary. Recent work has demonstrated that use of a blended format that combines online material and face-to-face interactions works better than either method alone.20 Viji Kurup, MD, shared his experience as an instructor at Yale Anesthesia, which utilizes the flipped classroom model.21 Online content is thoughtfully combined with in-person exercises to reinforce learning, as well as give learners an opportunity to practice skills, including teamwork, in a hands-on setting. These concepts can then be further reinforced through the use of spaced repetition, whereby content is strategically reintroduced following its initial introduction to maximize long-term retention of material.22 This approach, when integrated with online learning technology, can create systems that maximize our potential as both learners and teachers.
Conclusion
In recent years, the practice of anesthesiology has witnessed a lot of disruptive change for the better, enabled by technological advances. These changes have affected every facet of patient care: devices that are attached to patients, information systems that receive data from patients, collating data and sharing the data with national registries, and novel applications that promise to make learning more fun and efficient. The trajectories of these efforts are all aligned with technology to improve perioperative outcomes. We cannot wait to see what new surprises next year’s STA meeting will bring.
Acknowledgments: I would like to thank prior STA Annual Meeting Program Chairs Jorge Galvez, MD, and Allan Simpao, MD, as well as STA President Brian Rothman, MD, for their collective advice and support. The next STA meeting will take place January 10-13, 2018, in Miami, Florida.
References
- Wanderer JP, Ehrenfeld JM, Sandberg WS, et al. The changing scope of difficult airway management. Can J Anaesth. 2013;60(10):1022-1024.
- Gandomi A, Haider M. Beyond the hype: big data concepts, methods, and analytics. Int J Inf Manage. 2015;35(2):137-144.
- Levin MA, Wanderer JP, Ehrenfeld JM. Data, big data, and metadata in anesthesiology. Anesth Analg. 2015;121(6):1661-1667.
- Eisenach JC, Kheterpal S, Houle TT. Reporting of observational research in anesthesiology: the importance of the analysis plan. Anesthesiology. 2016;124(5):998-1000.
- Gregory SG, Anthopolos R, Osgood CE, et al. Association of autism with induced or augmented childbirth in North Carolina Birth Record (1990-1998) and Education Research (1997-2007) databases. JAMA Pediatr. 2013;167(10):959-966.
- Oberg AS, D’Onofrio BM, Rickert ME, et al. Association of labor induction with offspring risk of autism spectrum disorders. JAMA Pediatr. 2016;170(9):e160965.
- Cauley CE, Anderson G, Haynes AB, et al. Predictors of in-hospital postoperative opioid overdose after major elective operations: a nationally representative cohort study. Ann Surg. 2017;265(4):702-708.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769.
- Liau A, Havidich JE, Onega T, et al. The National Anesthesia Clinical Outcomes Registry. Anesth Analg. 2015;121(6):1604-1610.
- Nunnally ME, O’Connor MF, Kordylewski H, et al. The incidence and risk factors for perioperative cardiac arrest observed in the national anesthesia clinical outcomes registry. Anesth Analg. 2015;120(2):364-370.
- Bihorac A, Brennan M, Ozrazgat-Baslanti T, et al. National surgical quality improvement program underestimates the risk associated with mild and moderate postoperative acute kidney injury. Crit Care Med. 2013;41(11):2570-2583.
- Brown ML, Lenoch JR, Schaff HV. Variability in data: the Society of Thoracic Surgeons National Adult Cardiac Surgery Database. J Thorac Cardiovasc Surg. 2010;140(2):267-273.
- Voscopoulos CJ, MacNabb CM, Brayanov J, et al. The evaluation of a non-invasive respiratory volume monitor in surgical patients undergoing elective surgery with general anesthesia. J Clin Monit Comput. 2015;29(2):223-230.
- Galvagno SM Jr, Duke PG, Eversole DS, et al. Evaluation of respiratory volume monitoring (RVM) to detect respiratory compromise in advance of pulse oximetry and help minimize false desaturation alarms. J Trauma Acute Care Surg.2016;81(5 suppl 2 Proceedings of the 2015 Military Health System Research Symposium):S162-S170.
- Ianchulev S, Ladd D, MacNabb CM, et al. Use of a respiratory volume monitor to assess respiratory competence in cardiac surgery patients after extubation. J Clin Med Res. 2017;9(1):17-22.
- CWRU takes the stage at Microsoft’s Build conference to show how HoloLens can transform learning. http://case.edu/ hololens/ . Case Western Reserve University website. Accessed August 7, 2017.
- Hydrocephalus. www.stanfordchildrens.org/ en/ service/ neurosurgery/ hydrocephalus-treatment. Stanford Children’s Health website. Accessed August 7, 2017.
- Knight JF, Carley S, Tregunna B, et al. Serious gaming technology in major incident triage training: a pragmatic controlled trial. Resuscitation. 2010;81(9):1175-1179.
- Feinleib J, Mark L, French A, et al. Difficult Airway Algorithm and Rescue Cricothyrotomy (DAARC) Serious Game, to standardize the VA team approach to non-OR airways. www.researchgate.net. 2017. 10.13140/RG.2.2.12800.64005.
- Prunuske AJ, Batzli J, Howell E, et al. Using online lectures to make time for active learning. Genetics. 2012;192(1):67-72.
- Kurup V, Hersey D. The changing landscape of anesthesia education: is flipped classroom the answer? Curr Opin Anaesthesiol. 2013;26(6):726-731.
- Karpicke JD, Blunt JR. Retrieval practice produces more learning than elaborative studying with concept mapping. Science. 2011;331(6018):772-775.




Leave a Reply
You must be logged in to post a comment.