SUMMARY:In most cases, extubation is a planned, intentional, and controlled procedure, that occurs in the operating room, the Intensive Care Unit (ICU), and the emergency department. Unplanned extubation (UE) is any extubation that is not planned, intentional, and controlled. This complication can occur in the ICU or in the operating room setting, resulting in significant morbidity and mortality. The Society for Airway Management has partnered with the Patient Safety Movement Foundation to increase awareness and provide actionable patient safety solutions to reduce the incidence and complications related to unplanned extubation.
Introduction
In most cases, extubation is a planned, intentional, and controlled procedure that occurs in the operating room, the Intensive Care Unit (ICU), or the emergency department. However, even when the extubation is planned, intentional, and controlled, the rate of complications related to extubation in the operating room setting has been reported to be around 12%.1,2 Unplanned extubation (UE) is any extubation that is not planned, intentional, and controlled.3,4 This complication can occur in the ICU or in the operating room setting, resulting in significant morbidity and mortality.3-7 Unplanned extubation can occur when the patient dislodges or removes the endotracheal tube by pulling on it (self-extubation), or if an external force is applied to the endotracheal tube during movement of the patient or other nursing care (accidental extubation). It can also occur in any location where an intubated patient may receive care, such as the operating room, the ICU, the emergency department, procedural areas, or during patient transport. While many publications in the literature exist that address the challenges of difficult intubation, the complications and challenges of extubation have been less widely studied. This complication is not often tracked as a quality measure, so its incidence is most likely under-reported. This article discusses the scope of the problem and provides potential strategies to reduce the risk and incidence of UE.
Incidence and Risk Factors
The incidence of unplanned extubation as reported in the literature varies widely from a median of 7.3% (0.5–35.8%) in adults to as high as 18.2% (1–80.8%) in the neonatal population.5-8 The majority of studies were conducted in the ICU, and the reported incidence of UE in the operating room remains unknown. In the neonatal ICU, unplanned extubation is the fourth most commonly reported adverse event.5 A recent retrospective study found a higher incidence of unplanned extubation in COVID-19 patients (13.2%) compared to the incidence in intubated patients not infected with COVID-19 (4.3%).9
Unplanned Extubation in the Operating Room
Unplanned extubation is uncommon in the operating room since patients receive general anesthesia, as well as muscle relaxation, but it can still occur. Self-extubation can occur during emergence, and usually does not require re-intubation, but can pose a risk of vocal cord injury if the ETT cuff is still inflated. More serious is accidental extubation during the surgical procedure, which can occur during positioning, during prone surgical procedures or during head or neck procedures, which are in proximity to the airway. Several case reports exist of accidental extubation during prone spine surgery.10-11 Other procedures performed with the patient positioned 180 degrees away from the anesthesia machine restrict the anesthesia professional’s ability to visualize and monitor the endotracheal tube, which can potentially result in delayed recognition of tube dislodgement or extubation during the procedure. UE can also occur during the transfer of intubated patients (to or from the OR table, or from the OR to the ICU).
Unplanned Extubation in the ICU
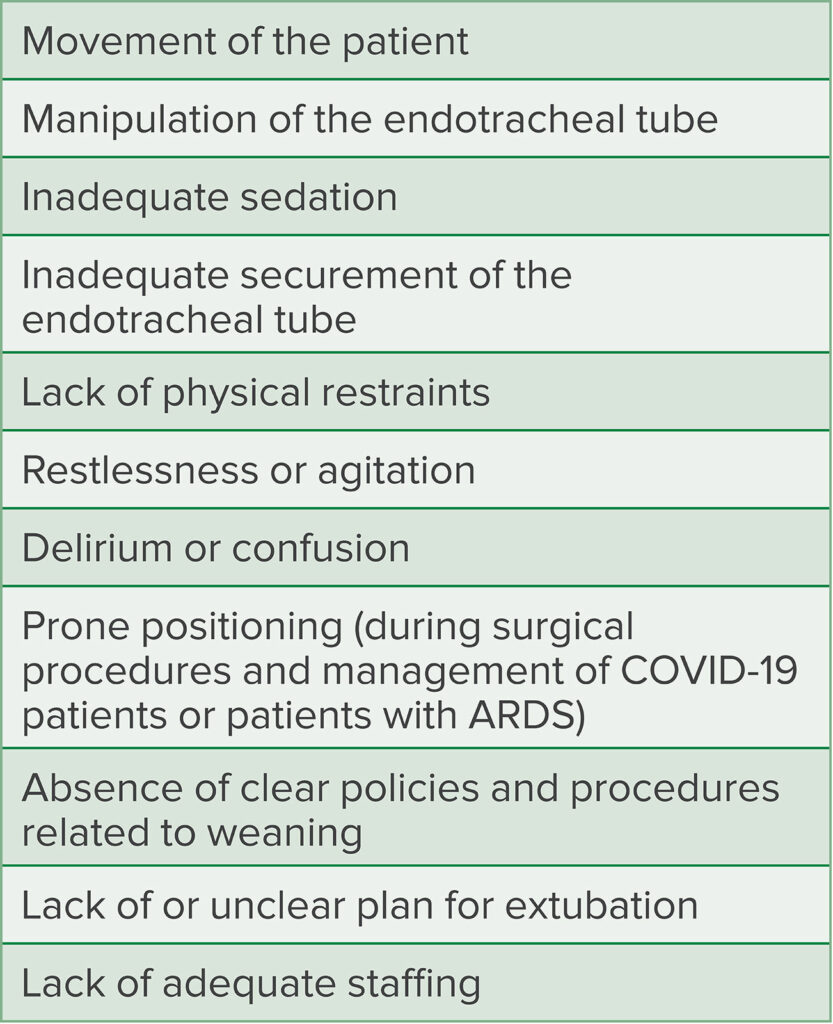
Unplanned extubation is more common in the ICU environment compared to the operating room setting, where muscle relaxation is less often employed, the patient to provider ratio is typically higher, and changes in position or tube manipulation are more frequent (Table 1). Self-extubation is the most common cause of UE in adult ICU patients, but other causes, classified as accidental extubation, include patient movement during bedside procedures, extubation during transport (between departments in the hospital or interfacility transports), and airway suctioning maneuvers.12 Intubated patients with COVID-19 often require prone placement to optimize ventilation, which is a known risk factor for UE.9
Table 1: Risk Factors for Unplanned Extubation12-14
Complications Related to Unplanned Extubation
Airway-related complications during emergence and extubation in the operating room have been reported to be as high as 30%.15 Airway-related complications are even higher outside the operating room and in uncontrolled situations.16 Unplanned extubation can result in immediate complications such as injury to the vocal cords or trachea, hypoxemia, hemodynamic instability, respiratory failure, brain damage, cardiac arrest, and death.15,17 If re-intubation is required after UE, the presence of hemodynamic instability or airway edema can make airway management more difficult. If the UE occurs during the surgical procedure, immediate access to the patient’s airway may be inhibited due to surgical drapes or positioning, making airway management challenging. This may result in delays in providing oxygenation and ventilation to patients. The incidence of re-intubation after unplanned extubation varies in the literature, but has been reported to be as high as 89%, and may carry a poor prognosis.18,19 The majority of studies looking at the need for re-intubation after unplanned extubation have been performed in the ICU setting, and reintubation is more commonly required after accidental extubation than self-extubation.19 Unplanned extubation has also been associated with a statistically significant increased risk of ventilator-associated pneumonia (increased from 13.8% to 30%), and prolonged ICU and hospital length of stay .19
Cost Burden
The complications of unplanned extubation and the impact on length of stay result in a significant cost burden. Studies that have factored in the cost of ICU care and the costs of complications due to unplanned extubation estimate that the overall yearly cost burden in the United States is approximately five billion dollars annually.20,21 A single unplanned extubation adds $41,000 to the average cost of an ICU stay (the average ICU stay costs $59,000) and increases total ICU stay costs to an estimated $100,178.21
Unplanned Extubation Prevention
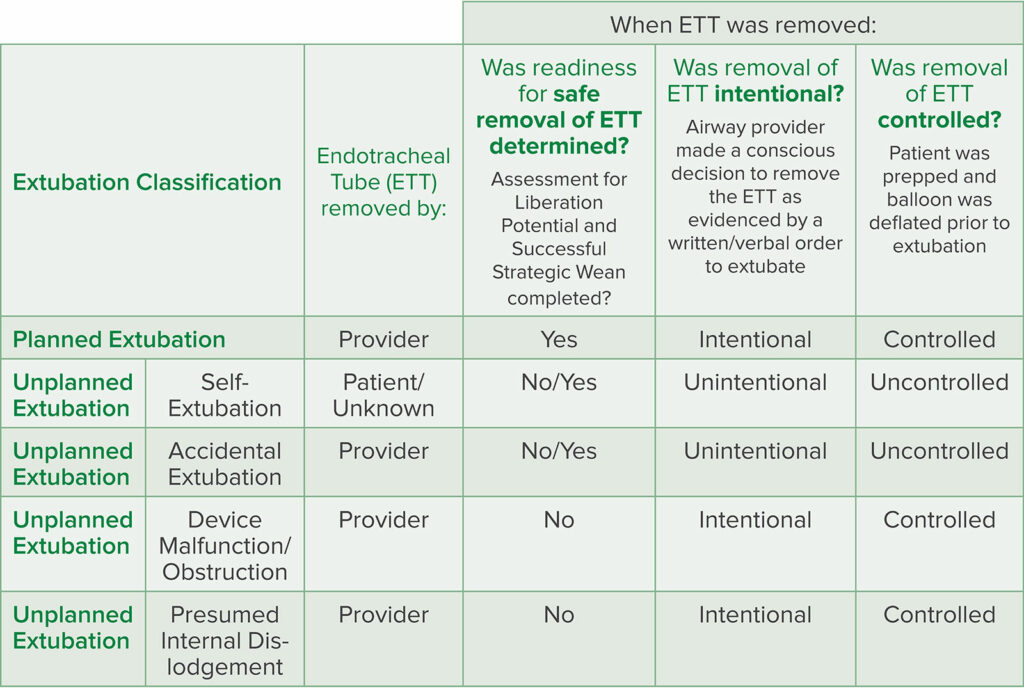
Is this complication preventable? Several strategies can be employed to reduce the risk of UE. The most important first step is recognition of the problem based upon data. Accurate tracking of every extubation and classification of every extubation as planned versus unplanned, using predefined definitions of extubation, are needed to identify if a problem exists (Table 2). Since UE is often not tracked, and most electronic medical record systems do not include data sets that track accidental or self-extubation, it is often not acknowledged as a problem. Another important step is recognition of risk factors. Education about how to identify and mitigate risk factors for UE should be provided to all clinicians that manage intubated patients. Vats et al. created an airway risk assessment scoring tool for pediatric patients to identify patients at higher risk.22 Incorporating risk assessment and mitigation strategies for UE into protocols used by providers managing these patients can increase awareness and potentially reduce complications.22,23
Table 2: Extubation Classification Tool
Source: Unplanned Extubation Actionable Patient Safety Solutions (APSS) patientsafetymovement.org
Accessed on November 15, 2021. Reprinted with permission.
In the operating room, briefings and time-outs can identify cases at higher risk for unplanned extubation, similar to discussions around cases at risk for airway fire. Many cases at risk for airway fire are also at higher risk for accidental extubation. These types of cases often require sharing of the airway and positioning of the patient far away from the anesthesia professional, and sometimes require extubation and re-intubation during a procedure. A pre-induction discussion of the optimal method to secure the endotracheal tube, how the tube may be manipulated during the procedure, and the location and availability of airway equipment in case of the need for urgent re-intubation should be performed to mitigate risk of UE.
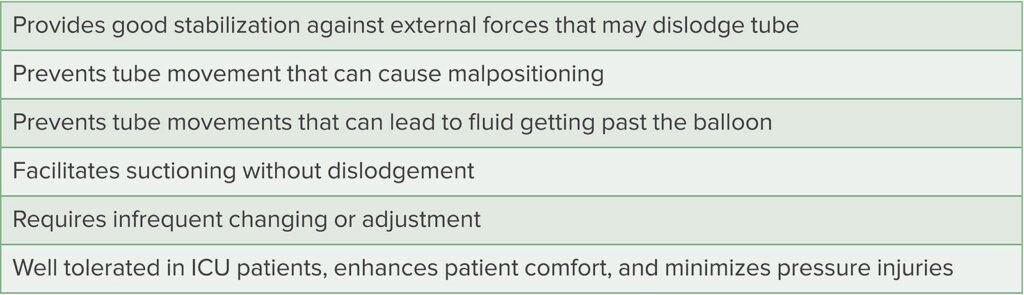
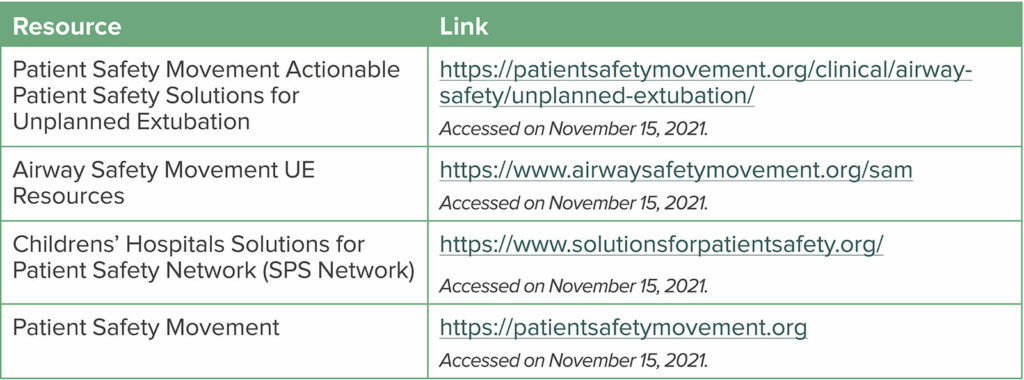
Protocols for bedside tube manipulation and patient transfers, bedside reminders with visual cues, and standardization of tube securement methods have been demonstrated to be effective in mitigating UE.23 Optimizing securement of the endotracheal tube may also reduce risk. Although no single securement method for the endotracheal tube has been proven to be superior, several attributes have been suggested in the literature (Table 3) and by the Patient Safety Movement Foundation in their Patient Safety Solutions (Table 4).24 Good communication and teamwork, especially during high-risk procedures such as suctioning, turning, or transport of a patient have been shown to be beneficial in reducing UE events.23 It is recommended that at least one provider be responsible for protecting the tube during these procedures to prevent dislodgement.23
Table 3: Suggested Characteristics of an Optimal Endotracheal Tube Securement Device
Table 4: Links and Resources related to Unplanned Extubation (UE)
Strategies to maximize oxygenation and ventilation after both planned and unplanned extubation can be employed to avoid the need for intervention both in the operating room and in the ICU. Several new methods of high-flow oxygenation via the nasal route can potentially delay or prevent the need for re-intubation by maximizing oxygen delivery.25,26 Several of these methods also provide continuous positive airway pressure (CPAP) and can be useful in patients at higher risk for airway obstruction and hypoxemia (i.e., obesity, obstructive sleep apnea). It is important to keep in mind that despite these strategies, many patients will still require re-intubation if oxygenation and/or ventilation remain inadequate after UE.
Future Directions
Unplanned extubation is an often an underrecognized and costly problem in the perioperative environment. Increasing awareness and preventive strategies are vital to address this problem. Better tracking, addition of core data sets in the electronic medical record, and quality improvement initiatives may make an impact on addressing this issue. The Patient Safety Movement Foundation (PSMF) includes UE as one of several important topics to address, as part of achieving a culture of safety.27 The PSMF, in addition to their Blueprints for Actionable Patient Safety Solutions, makes available educational, evidence-based resources and a coaching program to help hospitals develop a culture of safety, institute quality improvement programs, track UE, and decrease the incidence of unplanned extubation.27,28
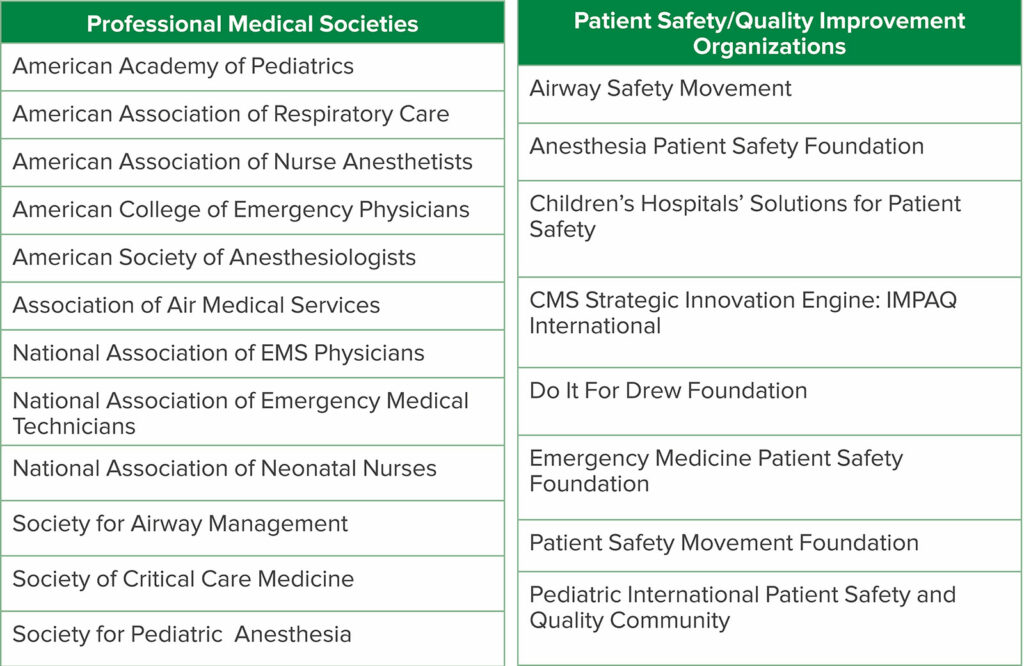
The Society for Airway Management, a global medical society devoted to improving airway safety, created a special projects committee to address UE. This committee formed a coalition with 20 medical societies and patient safety organizations to increase awareness of UE (Table 5). The coalition has published over 30 articles on UE and developed a toolkit consisting of checklists and core data sets that hospitals can use to track UE. The special projects committee and coalition have also partnered with the PSMF to create blueprints for Actionable Patient Safety Solutions (APSS) specifically addressing UE in both the adult and pediatric/neonatal populations. These resources are updated yearly and can be accessed free of charge from airwaysafetymovement.org or patientsafetymovement.org.
Table 5: Coalition for Unplanned Extubation Awareness And Prevention Members
The Coalition has also collaborated with the two newly created patient safety networks, The Children’s Hospitals’ Solutions for Patient Safety Network (SPS Network) and The Adult Hospital Solutions for Airway Safety Network. The Children’s SPS Network consists of over 135 children’s hospitals that are collaborating to reduce harm by sharing quality improvement methods and best practices to reduce UE. The newer Adult Network is modeled after the Children’s SPS Network and is adapting the practices already proven to be effective in children and neonates to the adult population.
References
- Asai T, Koga K, Vaughan RS. Respiratory complications associated with tracheal intubation and extubation. Br J Anaesth. 1998;80:767–775.
- Domino KB, Posner KL, Caplan RA, et al. Airway injury during anesthesia: a closed claims analysis. Anesthesiology. 1999;91:1703–1711.
- Ismaeil MF, El-Shahat HM, El-Gammal MS, et al. Unplanned versus planned extubation in respiratory intensive care unit, predictors of outcome. Egyptian J Chest Dis Tuberc. 2014;63:219–231.
- Bouza C, Garcia E, Diaz M, et al. Unplanned extubation in orally intubated medical patients in the intensive care unit: a prospective cohort study. Heart Lung. 2007;36:270–276.
- da Silva PS, Reis ME, Aguiar VE, et al. Unplanned extubation in the neonatal ICU: a systematic review, critical appraisal and evidence-based recommendations. Resp Care. 2013;58:1237–1245.
- da Silva PS, de Carvalho WB. Unplanned extubation in pediatric critically ill patients: a systematic review and best practice recommendations. Pediatr Crit Care Med. 2010;11:287–294.
- McNett M, Kerber K. Unplanned Extubations in the ICU: risk factors and strategies for reducing adverse events. J Clin Outcomes Manag. 2015;22:303–311.
- Kapadia FN, Bajan KB, Raje KV. Airway accidents in intubated intensive care unit patients: an epidemiological study. Crit Care Med. 2000;28:659–664.
- China AK, Loyd GE, Syzmanski TJ, et al. Frequency and analysis of unplanned extubation in coronavirus disease 2019 patients. Crit Care Explor. 2020;24:2:e0291.
- Rapheal J, Rosenthal-Ganon T, Gozal Y. Emergency airway management with a laryngeal mask airway in a patient placed in the prone position. J Clin Anesth. 2004;16:560–561.
- Hung MH, Fan SZ, Lin CP, et al. Emergency airway management with fiberoptic intubation in the prone position with a fixed flexed neck. Anesth Analg. 2008;107:1704–1706.
- Cosentino C, Fama M, Foà C, et al. Unplanned extubations in intensive care unit: evidences for risk factors. a literature review. Acta Biomed. 2017;88:55–65.
- Ai ZP, Gao XL, Zhao XL. Factors associated with unplanned extubation in the intensive care unit for adult patients: a systematic review and meta-analysis. Intensive Crit Care Nurs. 2018;47:62–68.
- Piriyapatsom A, Chittawatanarat K, Kongsayreepong S, et al. Incidence and risk factors of unplanned extubation in critically ill surgical patients: The Multi-Center Thai University-Based Surgical Intensive Care Units Study (THAI-SICU Study). J Med Assoc Thai. 2016;99:S153–S162.
- Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the 4th National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: Anaesthesia. Br J Anaesth. 2011;106:617–631.
- Robbertze R, Posner KL, Domino KB. Closed claims review of anesthesia for procedures outside the operating room.Curr Opin Anaesthesiol. 2006;19:436–442.
- Chao CM, Sung MI, Cheng KC, et al. Prognostic factors and outcomes of unplanned extubation. Sci Rep. 2017;7:8636.
- Mort TC. Unplanned tracheal extubation outside the operating room: a quality improvement audit of hemodynamic and tracheal airway complications associated with emergency tracheal reintubation. Anesth Analg. 1998;86:1171–1176.
- de Lassence A, Alberti C, Azoulay E, et al. Impact of unplanned extubation and reintubation after weaning on nosocomial pneumonia risk in the intensive care unit: a prospective multicenter study. Anesthesiology. 2002;97:148–156.
- Needham DM, Pronovost PJ. The importance of understanding the costs of critical care and mechanical ventilation. Crit Care Med. 2005;33:1434–1435.
- Dasta J, McLaughlin T, Mody S, Piech C. Daily cost of an ICU day. Crit Care Med 2005;33:1266–1271.
- Vats A, Hopkins C, Hatfield K, et al. An airway risk assessment score for unplanned extubation in intensive care pediatric patients. Pediatr Crit Care Med. 2017;18:661–666.
- Kandil SB, Emerson BL, Hooper M, et al. Reducing unplanned extubations across a children’s hospital using quality improvement methods. Pediatr Qual Saf. 2018;3: e114.
- Gardner A, Hughes D, Cook R, et al. Best practices in stabilization of oral endotracheal tubes: a systematic review. Aust Crit Care. 2005;18:160–165.
- Patel A, Nouraei SA. Transnasal Humidified Rapid-Insufflation Ventilator Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015;70:323–329.
- Jaber S, Monnin M, Girard M, et al. Apnoeic oxygenation via high-flow nasal cannula oxygen combined with non-invasive ventilation preoxygenation for intubation in hypoxaemic patients in the intensive care unit: the single-centre, blinded, randomised controlled OPTINIV trial. Intensive Care Med. 2016;42:1877–1887.
- https://patientsafetymovement.org/wp-content/uploads/2016/02/APSS-1_-Culture-of-Safety-copy.pdf
- https://patientsafetymovement.org/clinical/creating-a-foundation-for-safe-and-reliable-care/