“The ankle block could be one of the most underrated nerve block techniques in regional anesthesia practice,” said Admir Hadzic, MD, PhD, the director of NYSORA, the New York School of Regional Anesthesia. “Ankle block may be perceived as too cumbersome by some, because of the five different nerves that need to be blocked to anesthetize the entire foot below the ankle. However, it is possible to accomplish full anesthesia for specific procedures of the foot without needing to block all five nerves, instead blocking only two or three nerves that innervate the anatomical area where the surgery takes place.
“As an example, in our practice at NYSORA CREER (Center for Research, Education, and Enhanced Recovery) in Belgium, we anesthetize all patients scheduled for bunionectomy or hallux valgus osteotomy using a partial ankle block. For this procedure, the combination of easily blocked tibial, deep peroneal and superficial peroneal nerves is sufficient. Under ultrasound guidance, this block takes only a few minutes and provides complete anesthesia for the procedure. In this edition of “The Clinical Practice of the NYSORA,” which will be a quarterly series in Anesthesiology News, we describe the ankle block in detail and provide a practical guide for clinicians on how to make the most of it.”
Since the first description of the technique by Braun in 1914,1 and the introduction of ultrasound into regional anesthesia practice, a substantial evolution has occurred by speeding block onset and improving its success rate.2 Among the advantages of an ankle block is the preservation of ankle mobility, which facilitates unassisted ambulation, allowing faster recovery after surgery. Ultrasound guidance allows for precise identification of each nerve and superficial branches together with a consistent blockade while using lower volumes of local anesthetic.
Description of the Technique
The ankle block involves anesthetizing two deep nerves (tibial and deep peroneal) and three superficial cutaneous nerves (superficial peroneal, sural and saphenous). However, any combination of these nerves can be blocked to accomplish anesthesia or analgesia for the specific areas of surgical interest.
Because block of the larger nerves requires more time for block onset, we at NYSORA block the deep nerves first and then the superficial cutaneous ones. Block of the saphenous nerve is usually not necessary for surgeries on the forefoot and toes. In most patients, the saphenous nerve does not reach distally to innervate the toes.
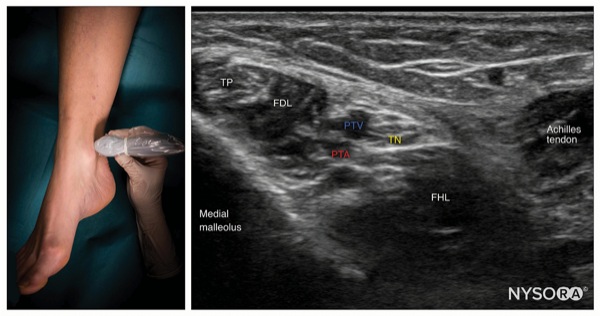
To Block the Tibial Nerve
Place the transducer in a transverse orientation between the medial malleolus and Achilles tendon (Figure 1).
Identify the tibial nerve as an oval hyperechoic structure next to the posterior tibial artery and veins, deep to the flexor retinaculum.
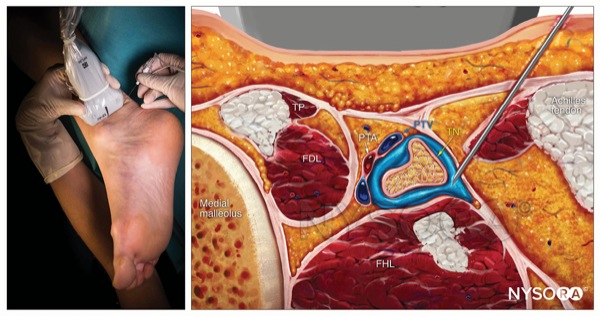
Insert the needle using an in-plane or out-of-plane approach toward the fascia enveloping the nerve (Figure 2).
Inject 1 to 2 mL of local anesthetic to confirm proper needle position by observing the spread into the fascial plane containing the nerve and surrounding the nerve.
Complete the block with a volume of 5 to 7 mL.
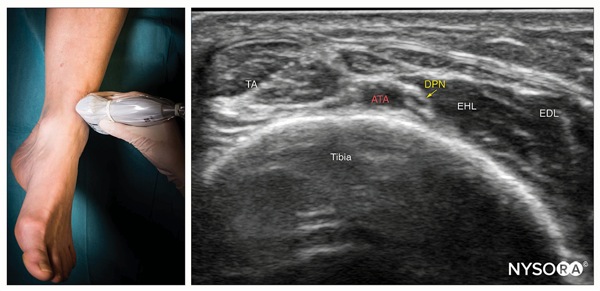
To Block the Deep Peroneal Nerve
Place the transducer in a transverse orientation over the anterior aspect of the ankle (Figure 3).
Identify the nerve as two small hypoechoic nodules with a hyperechoic rim lateral or superficial to the anterior tibial artery over the surface of the tibia.
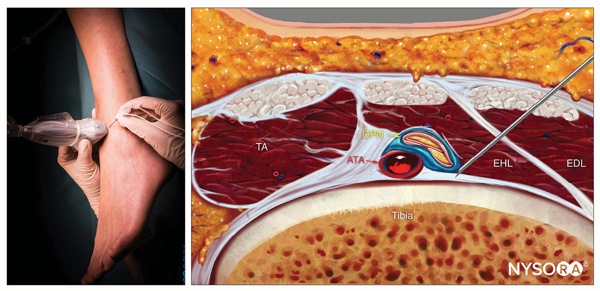
Insert the needle using an in-plane or out-of-plane approach (Figure 4).
Inject 1 to 2 mL of local anesthetic to confirm proper needle position by observing the spread within the fascial plane, displacing the nerve away from the needle.
Complete the block with a volume of 3 to 5 mL next to the nerve.
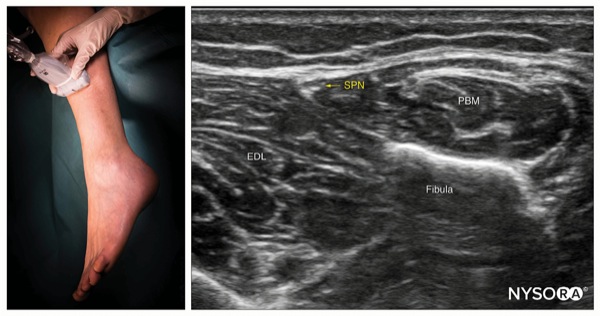
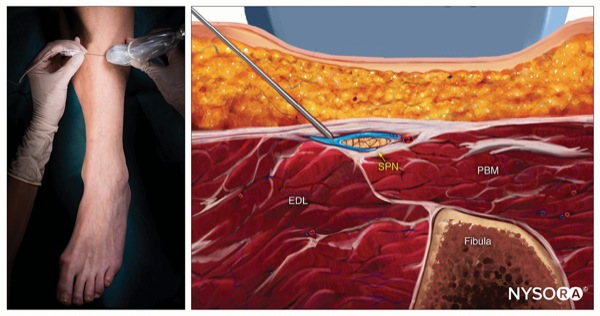
To Block the Superficial Peroneal Nerve
Place the transducer in a transverse orientation over the lateral aspect of the distal leg, 5 to 10 cm proximal to the lateral malleolus, over the fibula (Figure 5).
Identify the superficial peroneal nerve as a hypoechoic flat structure at the intersection between the crural fascia and intermuscular septum separating the lateral and anterior muscular compartments.
Insert the needle using an in-plane or out-of-plane approach into the fascial plane containing the nerve (Figure 6).
Inject 1 to 2 mL of local anesthetic to confirm proper needle positioning by observing the spread surrounding the nerve within the fascial plane.
Complete the block with a volume of 3 to 5 mL.
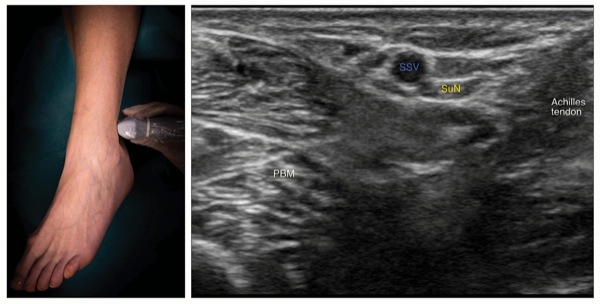
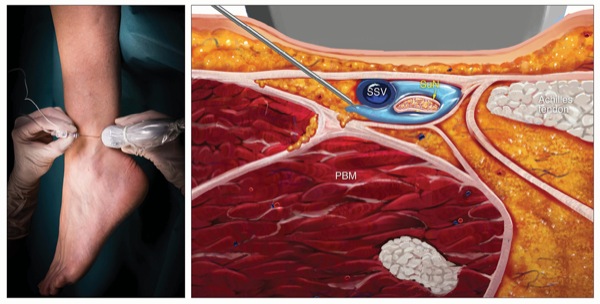
To Block the Sural Nerve
Place the transducer in a transverse orientation between the lateral malleolus and the Achilles tendon (Figure 7).
Identify the small saphenous vein superficial to the deep fascia and the sural nerve, which is a small hyperechoic structure next to it. The nerve may not always be seen.
Insert the needle using an in-plane or out-of-plane approach underneath the deep fascia (Figure 8).
Inject 1 to 2 mL of local anesthetic to confirm proper needle positioning by observing the spread around the small saphenous vein.
Complete the block with a volume of 3 to 5 mL.
To Block the Saphenous Nerve
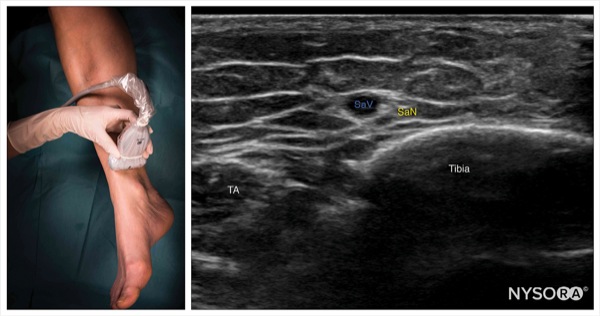
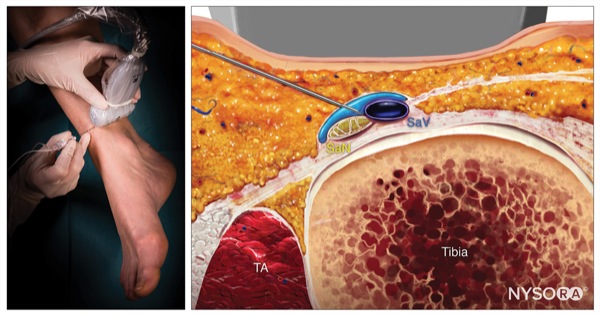
Place the transducer in a transverse orientation just proximal to the medial malleolus (Figure 9).
Identify the saphenous nerve as a small hyperechoic structure next to the great saphenous vein. The great saphenous vein is the main ultrasound landmark for this block because the nerve may not always be seen.
Insert the needle using an in-plane or out-of-plane approach toward the fascial plane surrounding the great saphenous vein (Figure 10).
Inject 1 to 2 mL of local anesthetic to confirm proper needle position by observing the spread surrounding the saphenous vein and nerve.
Complete the block with a volume of 3 to 5 mL.
In summary, we have described a standardized approach to the ankle block, which we use at NYSORA in our fast-paced ambulatory foot surgery unit with great results and patient satisfaction (Figure 11). When long-acting analgesia is required, the local anesthetic of choice is bupivacaine or levobupivacaine. However, in patients who have an edematous foot or infection, higher concentrations of local anesthetics (e.g., ropivacaine 1%) may be required for adequate block. Ropivacaine 1% or a mixture of ropivacaine 1% and lidocaine 2% is typically what we would use for distal foot, amputations or foot debridement surgeries.
Dr. Hadzic reported that he has consulted and/or performed sponsored research for Philipps, Pacira, B. Braun Medical and Heron Therapeutics. He owns and manages NYSORA.com (education), MedXpress.Pro (educational tools), and VisionExpo (medical design). He is also a member of the Anesthesiology News editorial advisory board. The remaining authors reported no relevant financial disclosures.
References
- Braun H. Operations on the extremities. In: Braun H, ed. Local Anesthesia, Its Scientific Basis and Practical Use. 3rd ed. Philadelphia, PA: Lea & Febiger; 1914:377Y380.
- Alain D, Philippe M, ClÉment C, et al. Ultrasound-guided ankle block. History revisited. Best Pract Res Clin Anaesthesiol. 2019;33(1):79-93.
Selected Reading
- Hadzic’s Textbook of Regional Anesthesia and Acute Pain Management. 2nd ed. New York NY: McGraw-Hill Education, 2017.
- López AM, Sala-Blanch X, Magaldi M, et al. Ultrasound-guided ankle block for forefoot surgery: the contribution of the saphenous nerve. Reg Anesth Pain Med. 2012;37(5):554-557.
- New York School of Regional Anesthesia. NYSORA web app. https://app.nysora.com/
- Soneji N, Peng PWH. Ultrasound-guided interventional procedures in pain medicine: a review of anatomy, sonoanatomy, and procedures. Part VI: Ankle joint. Reg Anesth Pain Med. 2016;41(1):99-116.
- Hadzic’s Textbook of Regional Anesthesia and Acute Pain Management. 2nd ed. New York NY: McGraw-Hill Education, 2017.
- López AM, Sala-Blanch X, Magaldi M, et al. Ultrasound-guided ankle block for forefoot surgery: the contribution of the saphenous nerve. Reg Anesth Pain Med. 2012;37(5):554-557.
- New York School of Regional Anesthesia. NYSORA web app. https://app.nysora.com/
- Soneji N, Peng PWH. Ultrasound-guided interventional procedures in pain medicine: a review of anatomy, sonoanatomy, and procedures. Part VI: Ankle joint. Reg Anesth Pain Med. 2016;41(1):99-116.



Leave a Reply
You must be logged in to post a comment.