Introduction
Time-out checklists reduce morbidity and mortality from surgical procedures.1 While these checklists are now ubiquitous in operating rooms, their adoption in other procedural areas is inconsistent, but no less important. The challenges of nonoperating room anesthesia (NORA) include ineffective team dynamics, remote location from assistance, unfamiliar procedures, and physical obstacles present in the work environment.2,3 In addition, studies have shown that patients receiving NORA tend to be older and have more comorbidities when compared to patients in the OR (operating room).4 The added complexities of a remote location with unique physical set up and staff that may be unfamiliar with working in NORA locations make the time-out checklist even more important in establishing common ground to ensure optimal patient care. The purpose of this review is to highlight important elements for designing and implementing a NORA checklist based on experience at our institution.
Many aspects of a time-out checklist are similar for both the OR and NORA locations, but there are some elements unique to, or more crucial to emphasize, in the NORA location. For example, waiting until the patient is prepped and draped before initiating the time-out is common practice in the OR. However, we recommend performing the time-out with the patient in the NORA location before induction of anesthesia, given potential idiosyncrasies of the procedures. For example, positioning for a Computerized Tomography (CT)-guided procedure may depend on an initial CT scan; it is inconvenient to convert to prone positioning after the patient is already intubated and supine on the CT carriage. Another possibility is the necessity of lung isolation for a procedure, which radiologists may forget to communicate to the anesthesia professionals ahead of time.
Checklist
Our time-out checklist focuses on four essential categories: 1. patient; 2. procedure; 3. team; and 4. emergency response.
- Patient—The patient information contained in the NORA checklist is very similar to that used in the OR. The usual patient identifying information, weight, and allergies are covered here. Additional information may include pregnancy test results, COVID-19 status, and coagulation studies. Disposition of the patient should also be discussed. In NORA locations, proceduralists are often consultants, not the primary care team, which highlights the need for discharge plans to be clarified, including the location of post-anesthesia care and whether the patient will be admitted or discharged home after the procedure.
- Procedure—Patient positioning, length of the intervention, discussion of potential complications, and anticipated post-procedural pain should be discussed, especially if the anesthesia professional is not as familiar with the procedure. Patients undergoing general anesthesia need proper positioning and padding, deep venous thrombosis prophylaxis, and temperature management. Staff in NORA locations may not be as accustomed to implementing these interventions and may need to gather appropriate equipment.
- Team—Team dynamics can be challenging, as members of the procedural team may not routinely work with anesthesia professionals. Establishing rapport with introductions may facilitate better teamwork and plays a crucial role in emergency response. The whole team should participate in the time-out to ensure everyone’s questions have been answered and there is a shared understanding of the plan of care. At our institution, the anesthesia team was unsuccessful in establishing a time-out practice at one NORA location until we involved the entire team of physicians, nurses, and technicians in the process.5
- Emergency response—One of the biggest challenges in NORA is its remote location, far from immediate availability of additional anesthesia personnel and life-saving equipment. Therefore, ensuring availability of emergency contact numbers for additional providers and anesthesia technicians is essential when help is needed. We have established a system of writing these contact numbers on a time-out whiteboard, ensuring all team members have this information and that someone other than the anesthesia team can call for help when needed. The location of the nearest code cart and malignant hyperthermia cart should be verified during the time-out.
For the time-out, we use a large whiteboard with prompts for all the key elements of the checklist (see Figure 1). We found that the visual cue of the elements of the checklist is key to a successful time-out. The visualized checklist creates a shared understanding of the plan of care, facilitates active participation, and ensures access to essential information throughout the procedure.
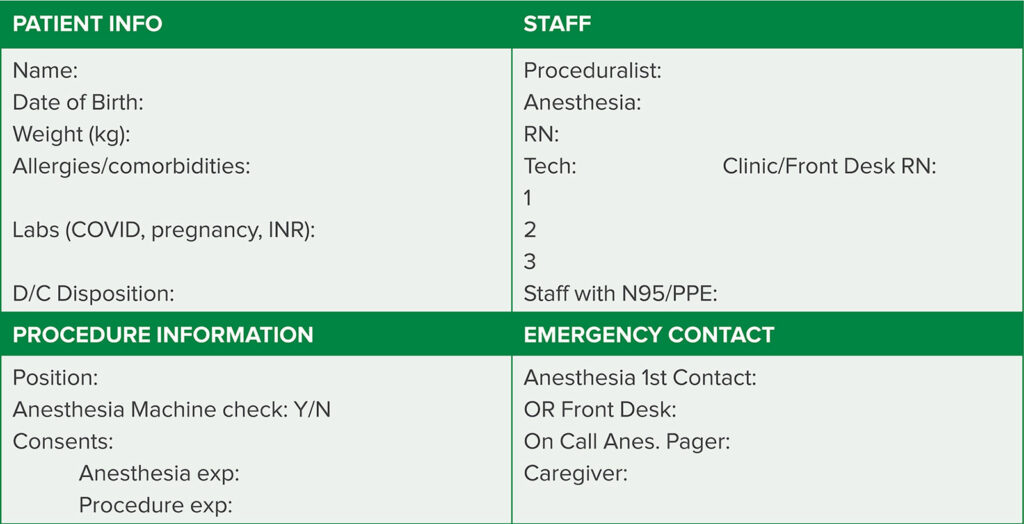
Figure 1. Example of a NORA time-out checklist, showing the four main categories: patient, procedure, team members, and emergency contact.
Conclusion
Establishing a time-out checklist requires more than simply providing a whiteboard and expecting people to use it. Like any quality improvement project, engaging the whole team is key to successful implementation. A successful time-out should include the issues proceduralists, anesthesia professionals, nurses, technicians, and patients have determined to be important to discuss prior to the procedure. Following implementation of the checklist, solicitation of feedback is crucial to long-term success. Having an anesthesia professional focused time-out alone is unlikely to be successful without engagement of other team members. Anesthesia professionals are often focused on hands-on tasks associated with placing lines and monitors, preparing for induction, and may be distracted from leading the time-out. We believe in emulating common OR practice where the proceduralist or circulating nurse leads the time-out. After implementation of the time-out, assessing compliance can establish expectations and ensure that the time out is integrated into the workflow of NORA locations.
Preventing adverse events and setting the stage for optimal response to unexpected events requires advance team preparation. Consistently performing a time-out before a patient is anesthetized for a NORA procedure establishes common ground for team members.
The NORA time-out also increases awareness of anticipated events during the procedure, and facilitates methods for accessing additional help when needed. This process will ensure that routine procedures proceed more smoothly as concerns can be discussed ahead of time, and also helps establish the appropriate actions should an adverse event occur. Given the complexities of working in NORA, such advance preparation could prevent significant morbidity and even mortality.
References
- Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–499.
- Chang B, Kaye AD, Diaz JH, Westlake B, Dutton RP, Urman RD. Interventional procedures outside of the operating room: results from the National Anesthesia Clinical Outcomes Registry. J Patient Saf. 2018;14:9–16.
- Walls JD, Weiss MS. Safety in non-operating room anesthesia (NORA). APSF Newsletter. 2019;34:3–4, 21. https://www.apsf.org/article/safety-in-non-operating-room-anesthesia-nora/. Accessed February 14, 2021.
- Nagrebetsky A, Gabriel RA, Dutton RP, Urman RD. Growth of nonoperating room anesthesia care in the United States: a contemporary trends analysis. Anesth Analg. 2017;124:1261–1267.
- Dudley R, Chang C. Time out for pediatric radiation therapy—a patient safety initiative. Poster session presented at 66th Annual Update in Anesthesiology, Park City, UT. February 2021.

