Communication failures in the clinical setting lead to poor outcomes in patient care.1,2 In particular, patients with low English proficiency (LEP) have been shown to experience less patient-centered care, utilize health care less frequently, and face increased risk of adverse events in the health care setting.3,4 High-risk situations that have been reported to be associated with poorer outcomes for LEP patients include medication reconciliation, discharge from the hospital, obtaining informed consent, emergency department care, and perioperative surgical care, all of which intersect with the work of anesthesia professionals.5,6 In the perioperative care environment, anesthesia professionals are encouraged to use in-person, telephone, or video interpreters to improve patient-physician communication and ensure the best quality patient care possible.7
Although providing care for patients with LEP has become easier with widespread availability of interpreter services, there remain points along the perioperative spectrum that are not easily conducive to their use.8-13 When looking through the lens of a patient’s perioperative journey, there are several settings in which language interpreter use is difficult or lacking. One such point is upon check-in and during the rooming process in the preoperative clinic. Although interpreters are often made available during the clinician encounter once the patient has been roomed, interpreters are rarely used in the process leading up to this point.11 Another point is within the intraoperative setting, where in-person interpreters often cannot readily enter the operating room, and telehealth interpreters often are not able to be effectively utilized during induction and emergence of anesthesia.13 While these points make up a relatively small portion of the perioperative spectrum, miscommunication and lack of effective communication along all parts of their perioperative journey can compromise the patient’s sense of safety. In response to these identified gaps, we enacted a quality improvement initiative focused on structural changes in the preoperative and intraoperative settings to enhance communication between the anesthesia care team and the LEP patient.
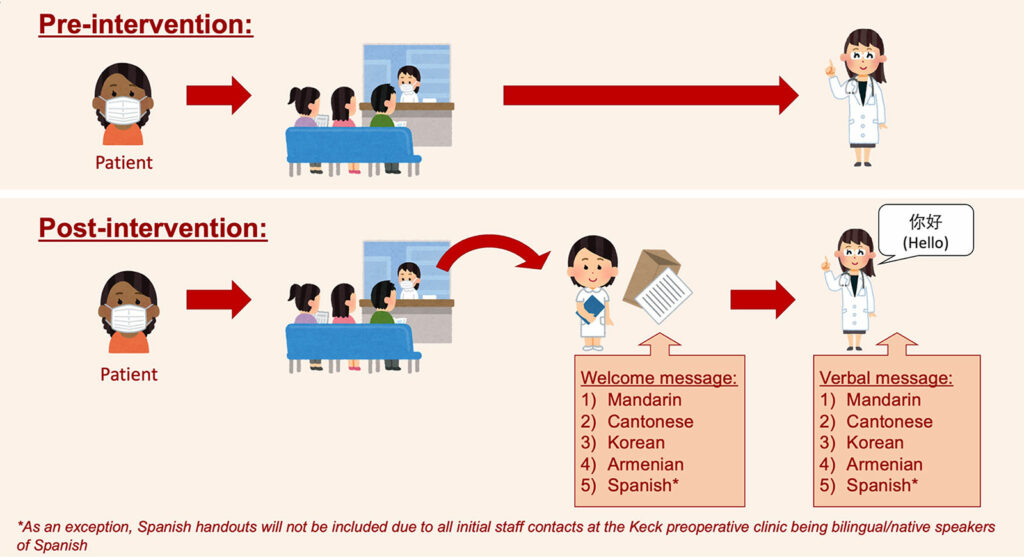
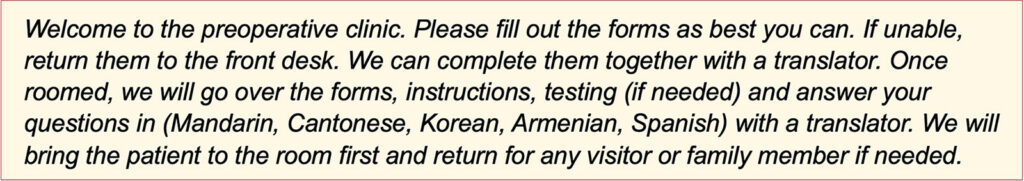
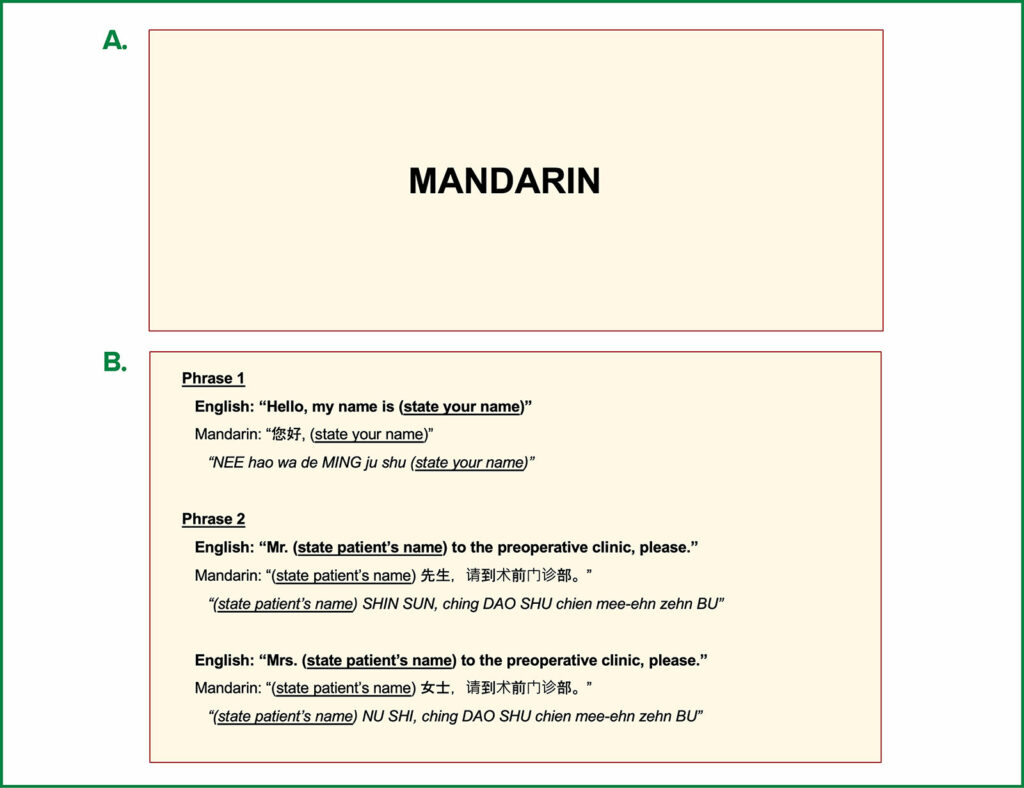
We first aimed to facilitate effective communication in our preoperative clinic, where the patient is first introduced to the anesthesia care team in our health system, by building patient rapport with a welcome message and an individualized greeting. In the immediate check-in process, a translated, laminated welcome message and visit description were provided to patients with LEP (Figure 1). The aim of this message was not only to outline the workflow and purpose of the visit, but also to reassure the patient that their health history, preoperative instructions, and questions would be discussed in their preferred language. Translations of the messages in the top ten most encountered foreign languages in our patient population were created by medical professionals who were native speakers (Figure 2). In addition, laminated cards identifying the patient’s language were placed in each LEP patient’s chart to visually indicate to health care staff the patient’s primary spoken language (Figure 3). On the back of these cards, phonetic pronunciations of how to say “Hi, my name is (staff name)” and “Mr./Mrs. (patient name) to the preoperative clinic, please” were printed in each of the ten languages accordingly, with the goal of having the staff greet, introduce themselves and call for patients in their native language. After rooming the patient, the chart would be available to the rest of the preoperative clinic team to also greet the patient in their native language.
Figure 1: Schematic demonstrating the structural changes we made to the preoperative clinic experience for those with language barriers. Used with permission from the authors.
Figure 2: Welcome message (English template) that was translated into the top ten languages encountered at Keck Hospital. Used with permission from the authors.
Figure 3: Front (a) and back (b) views of cards placed in each LEP patient’s chart. Used with permission from the authors.
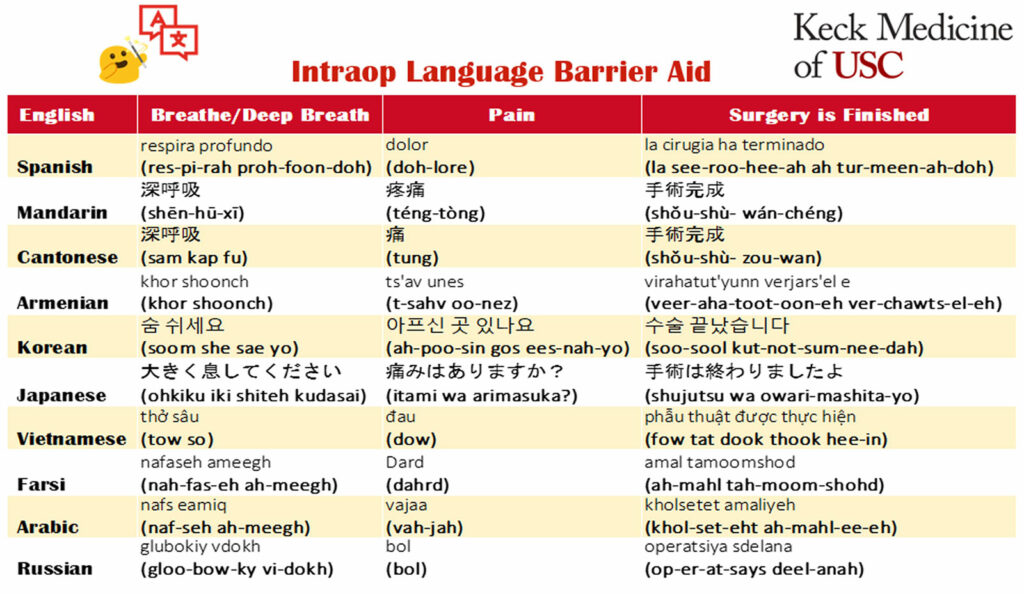
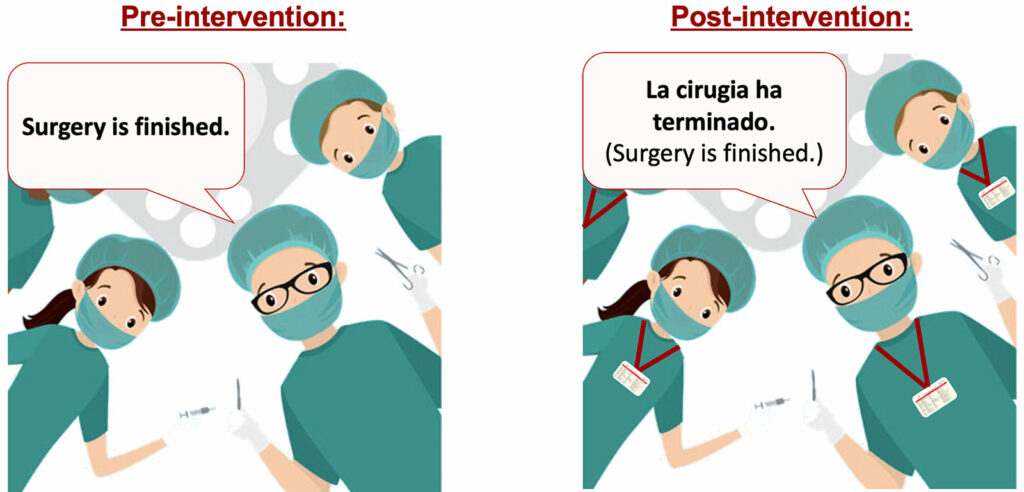
Similarly, on the day of surgery, we focused on reducing preoperative anxiety and improving physician-patient rapport by explaining to the patient that, while the in-person or video interpreter will not be accompanying us into the operating room, we will have a few key phrases in their preferred language for when they are going under and waking up from anesthesia. A badge card linguistic tool was crafted, which listed phonetic pronunciations of how to say “breathe”, “surgery is finished,” and “pain?” in the top ten foreign languages encountered at our institution (Figure 4). These translations were created by medical professionals who were also native speakers of these langauges, and distributed to all anesthesia care team members. Feedback on their use was encouraged. With this additional resource readily available, the anesthesia care team was now able to encourage deep breathing on induction and emergence, and in recovery to facilitate preoxygenation and improve postoperative ventilation. The care team was also able to improve reorientation on emergence by communicating that the surgery was now finished. Finally, they were able to better assess patient pain prior to transfer to the postanesthesia care unit in an effort to minimize untreated or undertreated postoperative pain. Thus, we improved communication with patients with LEP during critical parts of patient care with a few key words or phrases in the patient’s preferred language (Figure 5).
Figure 4: Badge card provided to all anesthesia staff at the Keck Hospital of USC. Used with permission from the authors.
Figure 5: Illustration of the effect of implementing the badge card linguistic tool intraoperatively. Used with permission from the authors.
In order to assess our quality improvement initiative, patients and clinical staff were asked to fill out a five-point Likert scale questionnaire to assess their experience. Survey results were compiled and assessed for patient satisfaction and overall feedback. Overwhelmingly, patients and staff responded that the changes positively impacted their experience. Fifty-three patients completed the survey, with 89% responding with a 5/5 response (strongly agree that our implemented greeting and message was a positive experience and made them feel welcomed). An additional 4% responded with a 4/5, and the remaining 7% responded with a neutral 3/5. There were no responses which indicated a negative impact on their experience. Fifty-six staff members consisting of representation from the preoperative clinic team and anesthesia care team completed the survey, with 88% responding with a 5/5 (strongly agree that the language tools were helpful and made a positive impact on patient interactions) and the remaining 12% responding with a 4/5.
Our initiative produced a few different notable outcomes. First, it demonstrated that it is feasible to introduce structural changes to address language barriers in the perioperative settings at low cost. The total cost incurred to generate the laminated welcome messages, chart cards, and badges was less than $250, which was funded by our department, and no outside funding or outside personnel were needed for this study. Secondly, this initiative was able to be implemented relatively quickly. It only took a few months to receive approval from the Institutional Review Board, prepare the translations, laminate, print, and distribute materials. Finally, we were able to facilitate improved communication on emergence in patients with LEP—a situation in which the degree of English proficiency is likely to be even lower than their preoperative state.
Overall, our quality improvement initiative demonstrates that these structural changes to the preoperative and intraoperative settings unsurprisingly improved the experiences of patients with LEP. Patients provided positive feedback in response to the changes, and health care staff involved appreciated the user-friendly nature of the language tools, noting that they helped patient greeting and rooming to feel more welcoming and less awkward. Based on the results of our current study, linguistic tools present a simple and practical approach to improving patient-provider communication within the operating room, as well as in the preoperative clinic. Furthermore, our interventions helped add a more personal element to the patient’s experience with the anesthesia team within our preoperative clinic and on the day of surgery. Patient-centric improvements to our care help build rapport and trust with our patients and improve the overall perioperative experience for both the patient and anesthesia care team.
Barriers to implementation included finding medical professionals to conduct the translations, as well as orienting health care staff to the new badges, cards, and welcome messages. However, after translations were completed and staff were oriented to the new process changes and available resources, the rest of the process went smoothly. The orientation process included brief in-person training to go over the new workflow and practice using the greeting cards and badges, all of which took around 30 minutes. We recognize that, while our institutional resources included in-house health care staff who speak the top ten languages encountered, this may not be the case everywhere. Therefore, alternative resources that may be considered include paid medical translation services. For the minority of patients (4.7%) who did not speak one of the top ten languages, an interpreter was available for the clinic visit. These languages will be included in future steps of this initiative.
Given the ease of implementation with minimal resources, our initiative demonstrates that similar improvements in the experience for LEP patients is feasible for most perioperative settings. The most common languages will differ at each institution based on patient demographics, but can be easily customized according to the needs of each institution. Overall, by improving communication between the health care staff and patients during the high-risk points during the preoperative assessment as well as during intraoperative care, we were able to achieve improved rapport with and quality of care for the LEP patient. Future steps in our initiative are aimed at increasing the number of languages represented, increasing the variety of phrases used intraoperatively, and finding ways to broaden the accessibility of these translations, such as through digital technology, especially given the recent increase in its use in the health care field.14,15 While mobile application translations services may go on to replace the hard-copy language aids in addressing the language barrier gap, we remain aware of digital literacy as a potential issue.14
In conclusion, our structural changes positively impacted the patient experience for those with language barriers. We demonstrated that these changes improved patient-centered care, whether facilitating communication upon emergence or feeling welcomed and appropriately greeted at our preoperative clinic. Ultimately, we aim to improve the perioperative care of LEP surgical patients one step at a time by identifying the barriers they face and tailoring their care to bridge those gaps.
REFERENCES
- Liu P, Lyndon A, Holl JL, et al. Barriers and facilitators to interdisciplinary communication during consultations: a qualitative study. BMJ Open. 2021;11:e046111. PMID: 34475150
- Dixit AA, Elser H, Chen CL, et al. Language-related disparities in pain management in the post-anesthesia care unit for children undergoing laparoscopic appendectomy. Children. 2020;7. PMID: 33020409
- Pérez-Stable EJ, El-Toukhy S. Communicating with diverse patients: how patient and clinician factors affect disparities. Patient Educ Couns. 2018;101:2186–2194. PMID: 30146407
- van Rosse F, de Bruijne M, Suurmond J, et al. Language barriers and patient safety risks in hospital care. A mixed methods study. Lang Commun Issues Health Care. 2016;54:45–53. PMID: 25840899
- Betancourt JR, Renfrew MR, Green AR, et al. Improving patient safety systems for patients with limited English proficency: a guide for hospitals. Published online September 2012. https://www.ahrq.gov/sites/default/files/publications/files/lepguide.pdf. Accessed February 19, 2024.
- Charwat H, Lane-Fall M. Anesthesia care for patients with limited English proficiency. APSF Newsletter. 2023;38:11–12. https://www.apsf.org/article/anesthesia-care-for-patients-with-limited-english-proficiency/ Accessed August 13, 2024
- Burkle CM, Anderson KA, Xiong Y, et al. Assessment of the efficiency of language interpreter services in a busy surgical and procedural practice. BMC Health Serv Res. 2017;17:456. PMID: 28676091
- Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42:727–754. PMID: 17362215
- Khoong EC, Fernandez A. Addressing gaps in interpreter use: time for implementation science informed multi-level interventions. J Gen Intern Med. 2021;36:3532–3536. PMID: 33948799
- Kapoor R, Owusu-Agyemang P, Feng L, Cata JP. The impact of the need for language assistance services on the use of regional anesthesia, postoperative pain scores and opioid administration in surgical oncology patients. J Pers Med. 2023;13. PMID: 36983663
- Azua E, Fortier LM, Carroll M, et al. Spanish-speaking patients have limited access scheduling outpatient orthopaedic appointments compared with English-speaking patients across the united states. Arthrosc Sports Med Rehabil. 2023;5:e465–e471. PMID: 37101862
- Jimenez N, Jackson DL, Zhou C, et al. Postoperative pain management in children, parental English proficiency, and access to interpretation. Hosp Pediatr. 2014;4:23–30. PMID: 24435597
- Shapeton A, O’Donoghue M, VanderWielen B, Barnett SR. Anesthesia lost in translation: perspective and comprehension. J Educ Perioper Med JEPM. 2017;19:E505. PMID: 28377945
- Mittermaier M, Venkatesh KP, Kvedar JC. Digital health technology in clinical trials. NPJ Digit Med. 2023;6:88. PMID: 33212293
- Kamdar N, Jalilian L. Telemedicine: A digital interface for perioperative anesthetic care. Anesth Analg. 2020;130(2):272-275. PMID: 31934901