Author: Bob Kronemyer
Anesthesiology News
Pain scores and other measured outcomes did not vary significantly between single-shot and continuous fascia iliaca blocks for geriatric patients with hip fractures.
Narcotic use, pain scores, opioid-related complications, hospital length of stay and time to ambulation were all similar between the two methods.
“We wanted to try to provide early and safe pain relief for these patients,” said co-principal investigator Carol Lin, MD, an assistant professor of orthopedic surgery at Cedars-Sinai Medical Center, in Los Angeles. “Both opioids and pain can cause delirium and other medical problems for these patients. How can we offer long-lasting pain relief without having to repeat procedures or use a lot of opioids?”
The study, which was presented at the 2019 annual meeting of the American Academy of Orthopaedic Surgeons, in Las Vegas (abstract PO978), consisted of 263 patients (mean age, 86 years) who presented with hip fractures at Cedars-Sinai between March 2017 and January 2018.
Patients were treated with either a single-shot (202 patients) or continuous (61 patients) block via a nerve catheter. The primary outcome was opioid use, pre- and postoperatively, as measured by morphine milligram equivalents (MME).
Single-Shot Block Performs Better Than Anticipated
Preoperatively, the single-shot block was 22.59 versus 27.45 MME for the continuous block. On the day of surgery, the single-shot block was 7.32 versus 6.35 MME for the continuous block. For day 1 post-op, MME was 15 and 13, respectively, and for day 2, 10.01 for both techniques.
For secondary outcomes of pain scores measured via the 0 to 10 visual analog scale, opioid-related complications (delirium, respiratory depression and urinary retention), length of stay and time to ambulation did not differ significantly between methods.
“We expected that patients treated with a nerve catheter would have less pain requirements,” Dr. Lin said. “But we actually found that a single-shot versus a continuous catheter failed to show much of a difference with patients. These two modalities are similar to a spinal versus an epidural. You would think the pain outcomes would sort of follow that course.”
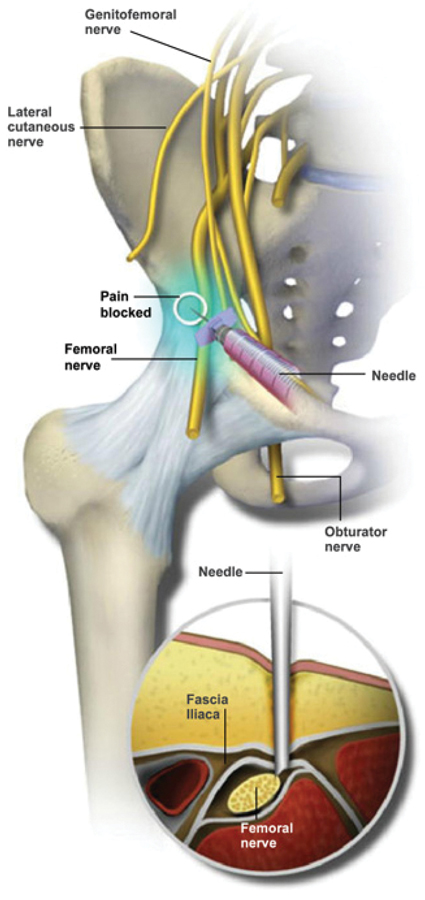
Dr. Lin said one of the reasons a fascia iliaca block is successful is because it is a volume-related block. “When we bolus the patients with a single shot, it is possible that the medication reaches further along fascial planes and provides better coverage, instead of doing a slow infusion in a single location,” she said. “Therefore, the efficacy we achieve is probably related more to volume than to dose.”
Dr. Lin is pleasantly surprised that a single shot showed equal pain efficacy to a continuous catheter. “For stability, it is going to be much easier to adopt this point-of-care procedure if it is a single-shot technique,” she said. “To do a catheter requires far more sophisticated resources.”
Another benefit of the study is that these two groups of patients can likely now be grouped together as one fascia iliaca block group for any larger research analysis.
Nonopioid Analgesia Essential
Edward Mariano, MD, a professor of anesthesiology, perioperative and pain medicine at Stanford University School of Medicine, in California, congratulated the authors for conducting the study, which shows the potential benefits of a peripheral nerve block in geriatric hip fracture patients.
“However, since this was not a randomized clinical trial, we cannot exclude selection bias in the choice of single-injection versus continuous catheter technique,” Dr. Mariano said. “Additionally, the lack of superiority is not the same as equivalence from a statistical standpoint.”
Nonetheless, “peripheral nerve block in either form represents an important component of multimodal analgesia for all surgical patients,” he said. “In geriatric hip fracture patients, use of any and all nonopioid analgesic modalities is essential.”
While the choice of a single-shot or continuous catheter block may be influenced by local factors, “the results of this study suggest that any form of regional analgesia should be employed for this patient population as part of a multimodal regimen,” Dr. Mariano said.


Leave a Reply
You must be logged in to post a comment.