Anesthesiology News
Department of Anesthesiology and Perioperative Medicine
Department of Pulmonary Medicine
Division of Anesthesiology and Critical Care
Department of Pulmonary Medicine
Division of Internal Medicine
Department of Pulmonary Medicine
Division of Internal Medicine
Section Chief, Interventional Pulmonology
Director, Interventional Pulmonology Fellowship Program
Deputy Department Chair
Department of Pulmonary Medicine
Division of Internal Medicine
The University of Texas MD Anderson Cancer Center
Houston
Case reports describe the stepwise safe anesthetic induction of two patients with anterior mediastinal masses using total intravenous anesthesia (TIVA) followed by tailored positive pressure jet ventilation (PPJV) and administration of a muscle relaxant.
Available reports suggest that an anterior mediastinal mass causing more than 50% narrowing of the trachea and compressing the great vessels can cause further narrowing of the airway and cardiovascular collapse after the administration of muscle relaxants.1,2 Accordingly, either inhalation induction of general anesthesia or awake intubation is used to avoid muscle relaxation.3,4
The following case reports describe the stepwise safe anesthetic induction of two patients with anterior mediastinal masses using TIVA followed by tailored PPJV and administration of a muscle relaxant.
Case 1
A 68-year-old woman with recurrent large B-cell lymphoma presents following multiple rounds of chemotherapy and palliative radiation. The patient developed progressive shortness of breath over a three-month period. The patient also complained of a choking sensation, hoarseness, dysphagia, and orthopnea along with increasing neck size.
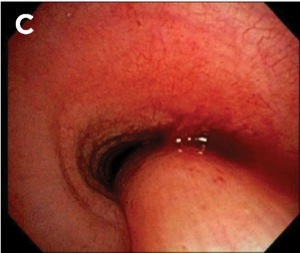
A CT scan showed a large anterior mediastinal mass measuring 9.3 cm. The mass encased the great vessels and the aortic arch, narrowing the tracheal luminal diameter to 7 mm (Figure 1A and B). The patient was scheduled for a rigid bronchoscopy for placement of a tracheal stent.
Preoperative assessment revealed hoarseness, audible stridor and palpable supraclavicular mass with engorgement of superficial neck veins. Preprocedural vital signs were heart rate, 116 beats per minute (bpm); blood pressure, 109/59 mm Hg; respiratory rate, 16 breaths per minute; and oxygen saturation, 97% via a 5-L nasal cannula.
An electrocardiogram showed sinus tachycardia. A preprocedural echocardiogram showed mild concentric left ventricular hypertrophy, a left ventricular ejection fraction of 45% to 50%, and mild global hypokinesis of the left ventricle. Consent for general anesthesia was obtained.
The patient was taken to the bronchoscopy suite and placed in a sitting position. Preoxygenation with non-rebreather face mask was started using standard American Society of Anesthesiologists monitoring. Additionally, bispectral index (BIS) and noninvasive arterial blood pressure monitoring were used. Propofol infusion of 250 mcg/kg per minute and 50 mcg of fentanyl were given. As the BIS reading dropped to the 60s, PPJV was initiated, with tidal volume in the range of 500 mL, a peak airway pressure of 20 cm H2O and an inspiratory–expiratory (I:E) ratio of 1:4 to avoid air trapping.
As the vital signs and oxygen saturation remained stable, the patient was gradually lowered to a supine position, at which the stability of the vital signs and ventilation were reassessed and deemed stable, and 120 mg of succinylcholine was given intravenously. Ventilation and hemodynamics were unchanged after muscle paralysis, an 11.2-mm rigid bronchoscope was inserted without difficulty, and PPJV was commenced.
Airway examination showed that the positive pressure generated by jet ventilation was associated with an increase in the diameter of the airway and adequate chest rise. However, during the expiratory phase, the airway diameter decreased to the narrowed baseline. As a result, we elected to increase the expiratory time to allow for adequate exhalation. Neuromuscular relaxation was maintained during the procedure using 5 mg of cisatracurium.
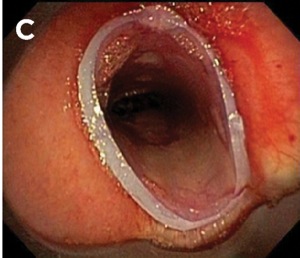
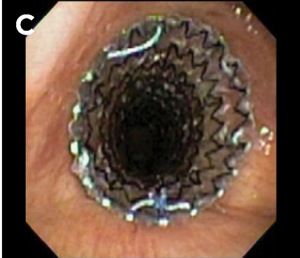
Bronchoscopic airway inspection revealed 70% to 80% obstruction of the trachea and main carina, 10% obstruction of the proximal right main stem bronchus and 60% obstruction of the left main stem (Figure 1C). A CRE balloon dilatation catheter (Boston Scientific) was used in the trachea. The patient was then extubated and reintubated using a 13.2-mm rigid bronchoscope through which a silicone Y stent was deployed (Figure 2A-C). The rigid bronchoscope was then removed and a laryngeal mask (LM) airway was placed. Muscle relaxation was reversed and the patient was extubated. The patient’s dyspnea and stridor resolved immediately after the procedure.
Case 2
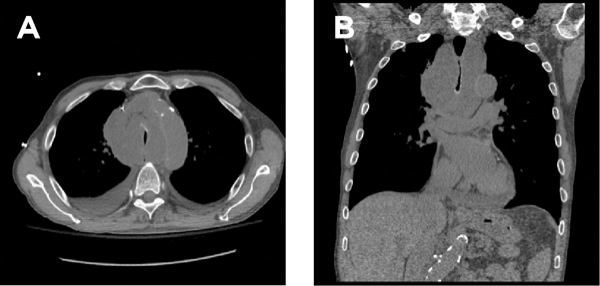
A 74-year-old man with advanced, poorly differentiated squamous cell carcinoma of the esophagus presented with acute worsening of shortness of breath shortly after undergoing an upper endoscopy. The patient complained of retrosternal chest discomfort and was noted to have wheezing and stridor. A CT scan of the chest revealed a large mediastinal mass, suggestive of a mediastinal abscess. The tracheal lumen was narrowed by approximately 80%. There were bilateral pleural effusions and a mild to moderate pericardial effusion (Figure 3A and B).
Preoperative assessment showed stridor, audible wheezing and engorged neck veins. Preprocedural vital signs were heart rate, 150 bpm; respiratory rate, 30 breaths per minute; blood pressure, 108/68 mm Hg; and oxygen saturation, 94% via a non-rebreather face mask. An electrocardiogram showed atrial fibrillation with a rate of 149 bpm. Preprocedural echocardiography was normal with an ejection fraction of 55% to 60% and a small pericardial effusion. Consent for general anesthesia was obtained.
Anesthesia
The patient was positioned, monitored, and preoxygenated in a similar manner to case 1. Anesthesia was induced with a propofol infusion at the rate of 200 mcg/kg per minute. Bag-mask ventilation was difficult due to the inability to create an adequate mask seal. As a result, an LM airway was inserted. PPJV through the LM airway was adequate, with tidal volumes of 500 to 800 cc at a peak airway pressure of 18 cm H2O and an I:E ratio of 1:4.
The patient was gradually lowered to a recumbent position, and adequate ventilation and hemodynamics were confirmed. Airway examination showed 80% obstruction of the trachea (Figure 3C) with an increase in airway diameter with PPJV and subsequent return to the narrowed baseline during the expiratory phase. The patient’s hemodynamics and ventilation remained stable before 6 mg of cisatracurium was administered. The LM airway was removed, the patient was intubated without difficulty using a 12-mm diameter rigid bronchoscope, and PPJV was initiated.
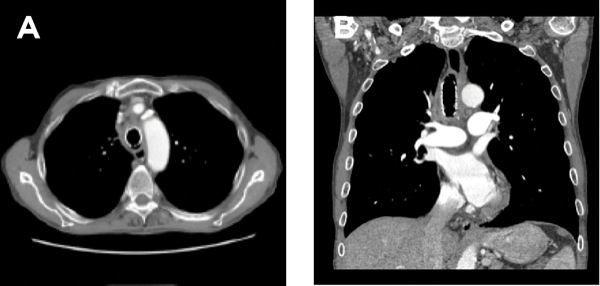
The trachea was dilated using the barrel of the rigid bronchoscope and a self-expanding hybrid metal stent was deployed into the lower trachea (Aero Tracheobronchial Stent System, 18 × 60 mm; Merit Medical) (Figure 4A-C). The rigid bronchoscope was then removed and an LM airway was placed. The muscle relaxation was subsequently reversed and the patient was extubated. The patient reported marked improvement in his dyspnea following the procedure.
Discussion
These cases illustrate that safe use of TIVA, including the judicious use of muscle relaxants, in patients with mediastinal masses compressing the tracheobronchial tree is possible. Key elements are:
- Adequate preoperative understanding of the obstructive physiology in question.
- Careful planning and appropriate safety precautions are mandatory, including the availability of rigid bronchoscopy and advanced airway management if needed.
- Ensuring the patient is in the sitting position and adequately preoxygenated prior to anesthesia induction adds a margin of safety. As the patient is gradually sedated, stepwise reduction in the angle of inclination while reassessing the adequacy of PPJV permits better control of a fluid clinical situation.
- If bag-mask ventilation proves to be difficult at any point, insertion of an LM airway should be attempted and the adequacy of PPJV assessed
- Increasing the expiratory time to avoid air trapping distal to the obstruction is essential.Unrecognized air trapping with consequent hyperinflation and increase in intrathoracic pressure could lead to cardiovascular collapse secondary to impaired venous return.
- Once ventilation adequacy and stable vital signs are established with tailored PPJV parameters, a muscle relaxant can be administered safely and PPJV can be maintained at the same ventilator settings.
- With adequate neuromuscular blockade in place, the insertion of a rigid bronchoscope becomes easier and provides an added safety measure, as it is able to stent the airway open beyond the obstruction, eliminating any air trapping.
Difficulty with bag-mask ventilation in patients with an anterior mediastinal mass is generally attributed to the narrowing of the airway; however, in our experience, particularly in patients with extrinsic airway compression, this is not the case. Under direct bronchoscopic vision, the airway diameter is actually noted to enlarge when PPJV is administered. The airway diameter is even larger when positive pressure is given in a paralyzed patient, as muscle relaxation enhances airway and lung expansion. This suggests that at least some of the difficulties reported in bag-mask ventilation of these patients may be due to air trapping and consequent hyperinflation.
It is also important to note that our back-up plan in both of these cases was to insert the rigid bronchoscope under local anesthesia if difficulty in ventilation or hemodynamic instability were encountered during induction.5,6 Additionally, pediatric patients are known to have more collapsible airways than adults, and the aforementioned technique was not examined in the pediatric population.7,8 The anesthesia technique described in these case reports was used in cases where airway stenting was planned and should not be used in other procedures, such as mass biopsy or central line placements, where a rigid bronchoscope and airway stent are not available.9,10
References
- Gardner JC, Royster RL. Airway collapse with an anterior mediastinal mass despite spontaneous ventilation in an adult. Anesth Analg. 2011;113(2):239-242.
- Bechard P, Létourneau L, Lacasse Y, et al Perioperative cardiorespiratory complications in adults with mediastinal mass: incidence and risk factors. Anesthesiology. 2004;100(4):826-834.
- Northrip DR, Bohman BK, Tsueda K. Total airway occlusion and superior vena cava syndrome in a child with an anterior mediastinal tumor. Anesth Analg. 1986;65(10):1079-1082.
- Goh MH, Liu XY, Goh YS. Anterior mediastinal masses: an anaesthetic challenge. Anaesthesia. 1999;54(7):670-674.
- Neuman GG, Weingarten AE, Abramowitz RM, et al. The anesthetic management of the patient with an anterior mediastinal mass. Anesthesiology. 1984;60(2):144-147.
- Galway U, Doyle DJ, Gildea T. Anesthesia for endoscopic palliative management of a patient with a large anterior mediastinal mass. J Clin Anesth. 2009;21(2):150-151.
- Mackie AM, Watson CB. Anaesthesia and mediastinal masses. A case report and review of the literature. Anaesthesia. 1984;39(9):899-903.
- Bittar D. Respiratory obstruction associated with induction of general anesthesia in a patient with mediastinal Hodgkin’s disease. Anesth Analg. 1975;54(3):399-403.
- Sibert KS, Biondi JW, Hirsch NP. Spontaneous respiration during thoracotomy in a patient with a mediastinal mass. Anesth Analg. 1987;66(9):904-907.
- Rath L, Gullahorn G, Connolly N, et al. Anterior mediastinal mass biopsy and resection: anesthetic techniques and perioperative concerns. Semin Cardiothorac Vasc Anesth. 2012;16(4):235-242.






Leave a Reply
You must be logged in to post a comment.