Anesthesiology News
Department of Anesthesiology
NYU Langone Health
New York, New York
Department of Anesthesiology
NewYork-Presbyterian Hospital/Weill Cornell Medical Center
New York, New York
Department of General Anesthesiology
Cleveland Clinic Abu Dhabi
Abu Dhabi, United Arab Emirates
Professor of Anesthesiology
Cleveland Clinic Lerner College of Medicine of Case Western Reserve University
Cleveland, Ohio
The incidence of difficult intubation ranges from 1% to 8%,2,4 and the incidence of failed intubation is approximately 0.05% to 0.35%.4 While less than 1 in 5,000 routine cases fall into the “cannot ventilate, cannot intubate” category, roughly 25% to 46% of anesthesia-related deaths are associated with difficult airways.5,6 Furthermore, the incidence of difficult mask ventilation and intubation increases in patients with comorbid conditions that predispose them to having difficult airways, such as rheumatoid arthritis, obesity, pregnancy, and facial malformations (Table 1).7These findings highlight the importance of considering regional anesthetic techniques as alternatives to general anesthesia, when possible.
| Table 1. Patient Risk Factors for Difficult Airways | ||
| Predictors of Difficult Ventilation | Predictors of Difficult Intubation | Examples of Patient Factors for Possible Difficult Airway |
|---|---|---|
| Edentulous | History of difficult intubation | Acromegaly |
| History of snoring | Inability to “prognath” (protrude the lower jaw) | Ankylosing spondylitis |
| Macroglossia | Limited neck range of motion | Intraoral or retropharyngeal abscess |
| Micrognathia | Mallampati class III or IV | Pierre Robin syndrome |
| Obesity | Mouth opening <4 cm | Rheumatoid arthritis |
| Obstructive sleep apnea | Obesity | Tracheal goiter or tumor |
| Presence of beard | Thyromental distance <6 cm | Treacher Collins syndrome |
| Based on references 2, 7, and 51-53. | ||
Criteria for Selecting Regional Anesthesia
Patients who are deemed to be at high risk for difficult mask ventilation or intubation may be eligible for regional anesthesia, avoiding the need to instrument their airways. Care should be taken in selecting eligible patients, taking into consideration both the type of surgery and patient factors (Table 2).
| Table 2. Favorable and Unfavorable Surgical Situations With Respect To Regional Anesthesia |
| Surgeries Appropriate for Regional Anesthesia Alone |
|---|
| Bunionectomy |
| Minor orthopedic procedures, such as shoulder arthroscopy or elbow open reduction with internal fixation |
| Transurethral resection of prostate |
| Uncomplicated cesarean delivery |
| Surgeries That May Require Preoperative Airway Management/General Anesthesia |
| Surgeries with major blood loss, such as major trauma |
| Long surgeries, such as finger replant |
| Surgeries in which airway access may be compromised, such as Achilles tendon surgery in prone position |
| Surgeries in which regional block may not cover entire surgical area, such as interscalene block for high humeral fracture |
| Based on reference 8. |
Regional anesthesia may be considered for short procedures without major expected blood loss. These surgeries include orthopedic arthroscopies, many urologic procedures, and even some peripheral vascular cases, such as the creation of an arteriovenous fistula. Peripheral nerve blocks and neuraxial anesthesia should also be considered when the risk of general anesthesia outweighs that of regional anesthesia, such as in cesarean deliveries. General anesthesia may be more appropriate for cases with major fluid shifts or high expected blood loss, or when regional techniques will not provide adequate analgesia.
Patient positioning and airway access should also be considered, as should long cases when patient comfort in the operating room may preclude the use of regional anesthesia as the primary anesthetic. In these cases, supplementing nerve blocks or neuraxial anesthesia with sedation or additional analgesics should be done carefully in patients with a difficult and unsecured airway.8
Patient selection is also crucial in deciding whether regional anesthesia should be chosen instead of general anesthesia. Absolute contraindications to peripheral nerve blockade include patient refusal, infection at the injection site, and true allergy to local anesthetics. Relative contraindications to peripheral nerve blockade include injury to the injection site, a bleeding disorder, or preexisting neuropathy. For spinal or epidural anesthesia, absolute contraindications include coagulopathy, severe and untreated hypovolemia, and increased intracranial pressure. Relative contraindications to neuraxial anesthesia include an uncooperative patient, sepsis, preexisting neuropathies or demyelinating diseases, and severe cardiac valve pathologies, such as aortic stenosis or mitral stenosis. Spinal deformities or prior back surgery may also preclude a patient from receiving neuraxial anesthesia.9-12
Good candidates for regional anesthesia should be able to remain calm and motionless enough to tolerate both nerve or neuraxial blockade and surgical procedures while awake. Patients with a history of claustrophobia may be unable to stay in an enclosed position during the surgery, and may require additional anesthesia.
In making the decision to proceed with regional anesthesia for a patient with a recognized difficult airway, the anesthesia environment should be optimized. The anesthesiologist should have expertise in regional anesthesia techniques and difficult airway management, as well as be immediately available in case of emergency. Equipment for difficult airway management and support should be readily accessible (Table 3). Both the surgical and anesthesia teams must be in full communication and fully cooperate to ensure patient safety.
Ideally, there should be easy and direct access to the head should there be any need for an unplanned endotracheal intubation or advanced airway management. Before proceeding, the patient with a difficult airway should be made aware of the possible conversion to general anesthesia and the potential placement of a surgical airway.8
| Table 3. Potentially Valuable Airway Tools, If Regional Anesthesia Needs Conversion to General Anesthesia |
| Airtraq (Teleflex) |
| Airway introducer/airway bougie |
| Cricothyroidotomy/tracheostomy kit |
| Direct laryngoscopes |
| Fiber-optic scope |
| Laryngeal mask or other type of supraglottic airway |
| Retrograde intubation kit |
| Video laryngoscope |
| Based on references 54 and 55. |
Possible Complications Of Regional Anesthesia
For a patient with a recognized difficult airway, the option of using regional anesthesia as the primary anesthetic technique may initially provide reassurance to the patient and all members of the medical team, as regional anesthesia helps to avoid the possibility of awake intubation, and also bypasses the dilemma encountered when deciding when and where to extubate the patient. However, one should recognize the potential limitations of this approach.
Placement of the peripheral nerve block or neuraxial block may be difficult or impossible. Patients who are at risk for having difficult airways can also have other anatomic anomalies precluding placement during regional procedures. An example of this is the patient with ankylosing spondylitis, which results in chronic inflammation of axial and peripheral joints. In the spine, the inflammatory process leads to fibrosis and ossification of the intervertebral disks, usually starting with sacroiliac joints and moving cephalad; spinal involvement can make placement of spinals or epidurals challenging.13,14
In a retrospective study by Schelew et al involving 82 patients with ankylosing spondylitis, epidural placement was entirely unsuccessful, and placement of spinals was not possible for 23.8% of patients scheduled for neuraxial anesthesia.13 Patients with ankylosing spondylitis have limited cervical flexion and temporomandibular joint disease, both of which make airway management immensely difficult. In the study, 2 of 35 patients undergoing conventional intubation after standard induction were unable to be intubated.13
Patients with rheumatoid arthritis, an autoimmune disorder with polyarthropathy affecting peripheral small joints with possible involvement of the axial skeleton, present similar challenges. Regional anesthesia often is preferred for this group of patients; however, peripheral nerve blocks and neuraxial blocks may be hard to place because of contractures or deformities limiting optimal positioning.15 The provider should also be cautious of high spinals in patients with rheumatoid arthritis. Leino et al found a mean spread of sensory block with bupivacaine to be 1.5 segments higher in patients with the disease compared with patients without rheumatoid arthritis.16
Obese parturients also present challenging airways due to friable mucosa, the presence of a full stomach, and excessive adipose tissue.17 Neuraxial anesthesia is also difficult in these patients due to difficulties with identification of landmarks.18 Nielsen et al showed that block failure rates increase with greater body mass index (BMI); in a study of 6,920 patients, block failure rate was 9.5%, 10.7%, and 12.7% for BMI levels <25, 25-29, and ≥30 kg/m2, respectively.19 The anesthesiologist should be prepared for the possibility of managing a difficult airway and proceeding with general anesthesia in the event of unsuccessful regional anesthesia procedures.
The anesthesiologist should also be aware of the possibility of inadequate analgesia, as blocks may be incomplete. Anatomic variations, such as the presence of epidural midline structures, can result in patchy epidurals despite successful placement of the catheter.20 A single peripheral nerve block may not cover the complete surgical area, necessitating a second block or supplemental analgesia, such as in the case of additional intercostobrachial nerve coverage needed for some upper arm surgeries.21
In orthopedic surgery, patients can also experience tourniquet pain, which is difficult to treat despite success of regional anesthesia procedures.22,23 For patients with difficult airways, tourniquet pain may be managed by deflating the tourniquet more regularly in an effort to avoid sedating the patient.22 Choosing an appropriate local anesthesia solution to use is very important to ensure adequate analgesia, especially with single-shot nerve blocks or spinals. If the surgery lasts longer than the duration of nerve blockade, then the anesthesiologist may need to provide general anesthesia and manage a difficult airway.
Emergency situations can arise and lead to an unplanned endotracheal intubation. Complications from regional anesthesia can include unexpected true allergy to local anesthetics, inadvertent intravenous injection of local anesthesia, or local anesthesia systemic toxicity (LAST). These patients may react with altered mental status, seizures, arrhythmias, and even cardiac arrest.24One of the mainstays of management for LAST includes airway management, which may be challenging for patients with recognized difficult airways.
High or total spinals, leading to apnea and cardiovascular collapse, can also necessitate unplanned and emergent intubation. Another situation requiring possible conversion to general anesthesia and instrumentation of the airway include unanticipated hemodynamic instability caused by blood loss, hypothermia, or myocardial ischemia or infarct. Smokers and patients with reactive airway disease are at increased risk for laryngospasm and bronchospasm; for a patient who may be difficult to intubate or mask ventilate, this can be potentially disastrous and even fatal.25
Regional Versus General Anesthesia
Currently, there is no conclusive evidence in the literature to support the use of either regional over general anesthesia or vice versa in managing most patients with difficult airways.26 While studies to date have specifically looked at airway complications that compare these two types of anesthesia techniques, there are many studies that assess other outcomes, including morbidity and mortality, patient satisfaction, and health care cost-effectiveness.27,28
In the appropriate patient, use of regional over general anesthesia offers benefits in addition to avoidance of a potentially difficult airway. For obstetric patients undergoing cesarean delivery, the trend has leaned away from general anesthesia toward neuraxial.29 Improved outcomes include less blood loss,30,31 decreased postoperative pain,32 and higher patient satisfaction scores.32,33The American Society of Anesthesiologists’ Task Force recommends using spinal or epidural anesthesia over general anesthesia for most cesarean deliveries.34
In a retrospective study comparing interscalene blocks with general anesthesia for patients undergoing shoulder arthroplasty, there was less total intraoperative time, decreased length of PACU stay, and fewer unplanned admissions related to pain, sedation, or nausea and vomiting in patients who received an interscalene block.35 For patients undergoing total hip arthroplasty, studies comparing regional with general anesthesia showed decreases in surgical site infection rates,36 hospital length of stay,36 operative time,37 and cardiovascular adverse events.36,37Interestingly, in a retrospective study of 20,936 patients undergoing total hip arthroplasty,37 there was a statistically significantly increased risk for postoperative unplanned intubation with the use of general anesthesia compared with regional anesthesia.
For some patients, it may be prudent to control the airway electively before surgery in addition to performing peripheral nerve blocks or neuraxial anesthesia. Some surgeries require the use of both regional and general anesthesia. Thoracic epidurals are often used in major abdominal and thoracic surgeries in conjunction with general anesthesia, which reduces thromboembolic events, improves respiratory function, and better controls postoperative pain.38-41 Digit replantation surgeries benefit from the reduction of vasospasm,42 increased perfusion,43 and vasodilation44resulting from peripheral nerve blocks; however, general anesthesia is often needed as well due to the length of these operations.45,46
The anesthesiologist might also consider securing the airway in a patient who has received a block or neuraxial anesthesia in instances when the airway is difficult to access during the surgery, or if the patient is at high risk for deteriorating during the surgery. The decision to proceed with regional anesthesia with or without a secure airway should be made with careful consideration of the patient and surgical and environmental factors.
Regional Anesthesia for the Airway
Regional anesthesia can be useful for blocking innervation of the airway to secure the airway in an awake patient. This is particularly useful for patients with recognized difficult airways, in which standard induction of anesthesia may put the patient at risk for a “cannot ventilate, cannot intubate” situation.
Understanding the anatomy of the airway is crucial to determining which structures to block. The upper airway is divided into the nasal cavity, oropharynx, pharynx, and larynx. The nasal cavity is innervated by branches of the trigeminal nerve, specifically the anterior ethmoidal nerve and the greater and lesser palatine nerves. Oropharyngeal sensation comes from branches of the vagus, trigeminal, and glossopharyngeal nerves. Branches of the vagus nerve innervate the epiglottis and more distal airway structures. For oral intubation, it is important to block innervation to the posterior portion of the tongue, hypopharynx, larynx, and proximal trachea.8,47 Nasal intubation requires additional blocks to the nasopharynx.47
When performing awake intubation, it is important to block nerves contributing to the gag reflex, glottic closure reflex, and cough reflex.48 The gag reflex is controlled by the glossopharyngeal nerve as the afferent branch and the vagus nerve as the efferent branch. The glottic closure reflex comes from stimulation of the superior laryngeal nerve, triggering the efferent recurrent laryngeal nerve. The cough reflex is mediated by branches of the vagus nerve.
It is prudent to adequately prepare the patient for an awake intubation. The patient should be psychologically aware and cooperative. Anxiolytic and analgesic medications are often given; however, use caution to avoid oversedating the patient, as this can lead to airway obstruction and apnea.49 Antisialogogues, such as glycopyrrolate, can be given to decrease secretions, allowing for better fiber-optic visualization of the airway and increased absorption of topical anesthesia into the oropharynx.47,49 Supplemental oxygen should also be given prior to attempts at awake intubation.
Anesthetizing the airway can be done topically or with targeted nerve blockade. Topical anesthesia can be given by applying concentrated lidocaine jelly or ointment to the tongue and spraying lidocaine while advancing toward the vocal cords.48 Three nerve blocks used for anesthetizing the airway are the glossopharyngeal block, superior laryngeal block, and the translaryngeal block.50 For nasal intubations, local anesthesia can be applied to block the palantine and anterior ethmoid nerves.48,50 Once the airway is appropriately anesthetized, intubation can be accomplished with either laryngoscopy or a fiber-optic scope.
Conclusion
Using regional anesthesia as the primary anesthetic helps avoid a difficult airway, but the anesthesiologist should recognize that the difficult airway is still present. It is prudent to carefully devise an anesthetic plan for these patients before entering the operating room.
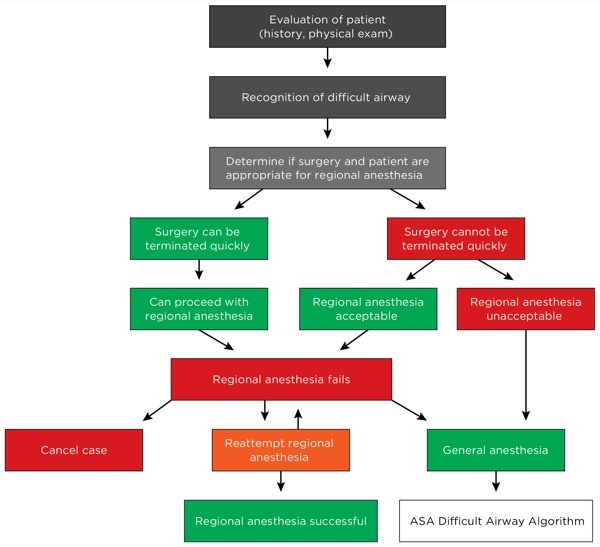
The algorithm presented here (Figure) is valuable for managing regional anesthesia and its role in patients with recognized difficult airways. According to this algorithm, which is adapted from Fleisher et al,26 once the difficult airway is recognized, the next step is to determine if the surgery can be performed under regional anesthesia and establish how quickly surgery can be stopped should any difficulties arise. Regional anesthesia is advisable if the surgery can be terminated quickly or if there is no perceived difficulty in accessing the airway in the middle of the case.
For cases in which regional anesthesia fails, options include retrying the block or converting to general anesthesia using an awake intubation method. The anesthesiologist should be aware of the American Society of Anesthesiologists’ difficult airway algorithm in cases when regional anesthesia may be contraindicated or in emergency situations.
Overall, the anesthesiologist should recognize that although regional anesthesia allows for avoiding the handling of a difficult airway, the possibility of a difficult airway is still present; the anesthesiologist should always be prepared to obtain airway access in case of a needed conversion to general anesthesia.
References
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251-270.
- Shah PN, Sundaram V. Incidence and predictors of difficult mask ventilation and intubation. J Anaesthesiol Clin Pharmacol. 2012;28(4):451-455.
- Kheterpal S, Martin L, Shanks AM, et al. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology. 2009;110(4):891-897.
- Seo SH, Lee JG, Yu SB, et al. Predictors of difficult intubation defined by the intubation difficulty scale (IDS): predictive value of 7 airway assessment factors. Korean J Anesthesiol. 2012;63(6):491-497.
- Cook TM, MacDougall-Davis SR. Complications and failure of airway management. Br J Anaesth. 2012;109(Suppl 1):i68-i85.
- Peterson GN, Domino KB, Caplan RA, et al. Management of the difficult airway: a closed claims analysis. Anesthesiology. 2005;103(1):33-39.
- Gupta S, Sharma KR, Jain D. Airway assessment: predictors of difficult airway. Indian J Anaesth. 2005;49(4):257-262.
- Hagberg CA. Benumof and Hagberg’s Airway Management E-Book. Elsevier Health Sciences; 2012.
- Butterworth JF, Mackey DC, Wasnick JD. Spinal, epidural, & caudal blocks. In: Morgan & Mikhail’s Clinical Anesthesiology. 5th ed. New York, NY: McGraw-Hill Education; 2013.
- Warren DT, Neal JM, Bernards CM. Neuraxial anesthesia. In: Longnecker DE, Brown DL, Newman MF, et al, eds. Anesthesiology. New York, NY: McGraw-Hill Education; 2012.
- Horlocker TT, Wedel DJ, Rowlingson JC, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine evidence-based guidelines (third edition). Reg Anesth Pain Med. 210;35(1):64-101.
- Bernards CM, McDonald SB, Salinas FV. A Practical Approach to Regional Anesthesia. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009.
- Schelew BL, Vaghadia H. Ankylosing spondylitis and neuraxial anaesthesia—A 10 year review. Can J Anaesth. 1996;43(1):65-68.
- Singh M, Chaudhary S, Arya AK, et al. Difficult airway with difficult regional anaesthesia for lower limb orthopaedic surgeries in patients with ankylosing spondylitis. What should we opt for? Sri Lankan J Anaesthesiol. 2012;20(1):39-42.
- Samanta R, Shoukrey K, Griffiths R. Rheumatoid arthritis and anaesthesia. Anaesthesia. 2011;66(12):1146-1159.
- Leino KA, Kuusniemi KS, Pälve HK, et al. Spread of spinal block in patients with rheumatoid arthritis. Acta Anaesthesiol Scand. 2010;54(1):65-69.
- Rao DP, Rao VA. Morbidly obese parturient: challenges for the anaesthesiologist, including managing the difficult airway in obstetrics. What is new? Indian J Anaesth. 2010;54(6):508-521.
- Bansal T, Kumar P, Hooda S. Regional anaesthesia—still a comfortable choice in morbidly obese parturient. Rev Colomb Anestesiol. 2013;41(4):302-305.
- Nielsen KC, Guller U, Steele SM, et al. Influence of obesity on surgical regional anesthesia in the ambulatory setting: an analysis of 9,038 blocks. Anesthesiology. 2005;102(1):181-187.
- Portnoy D, Vadhera RB. Mechanisms and management of an incomplete epidural block for cesarean section. Anesthesiol Clin North America. 2003;21(1):39-57.
- Hadzic A. Cutaneous nerve blocks of the upper extremity. In: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia. New York, NY: McGraw-Hill Education; 2012.
- Kumar K, Railton C, Tawfic Q. Tourniquet application during anesthesia: “What we need to know?” J Anaesthesiol Clin Pharmacol. 2016;32(4):424-430.
- Saied A, Ayatollahi Mousavi A, Arabnejad F, et al. Tourniquet in surgery of the limbs: a review of history, types and complications. Iran Red Crescent Med J. 2015;17(2):e9588.
- Christie LE, Picard J, Weinberg GL. Local anaesthetic systemic toxicity. Contin Educ Anaesth Crit Care Pain. 2015;15:136-142.
- Gavel G, Walker RW. Laryngospasm in anaesthesia. Contin Educ Anaesth Crit Care Pain. 2014;14(2):47-51.
- Fleisher LA. Evidence-Based Practice of Anesthesiology. Philadelphia, PA: Elsevier Saunders; 2013.
- Kettner SC, Willschke H, Marhofer P. Does regional anaesthesia really improve outcome? Br J Anaesth. 2011;107(Suppl 1):i90-i95.
- Iohom G, Shorten G. Outcome studies comparing regional and general anesthesia. In: Finucane B, ed. Complications of Regional Anesthesia. New York, NY: Springer; 2007:39-52.
- Bucklin BA, Hawkins JL, Anderson JR, et al. Obstetric anesthesia workforce survey: twenty-year update. Anesthesiology. 2005;103(3):645-653.
- Dyer RA, Els I, Farbas J, et al. Prospective, randomized trial comparing general with spinal anesthesia for cesarean delivery in preeclamptic patients with a nonreassuring fetal heart trace. Anesthesiology. 2003;99(3):561-569.
- Afolabi BB, Lesi FE. Regional versus general anaesthesia for caesarean section. Cochrane Database Syst Rev.2012;10:CD004350.
- Mekonnen S, Eschete A, Desta K, et al. Maternal satisfaction and postoperative pain severity in mothers who undergo caesarean section under general and spinal anesthesia in Gandhi Memorial Hospital, Addis Ababa. Int J Anesth Res.2014;4(7):294-299.
- Fassoulaki A, Staikou C, Melemeni A, et al. Anaesthesia preference, neuraxial vs general, and outcome after caesarean section. J Obstet Gynaecol. 2010;30(8):818-821.
- American Society of Anesthesiologists Committee on Standards and Practice Parameters. Practice guidelines for obstetric anesthesia: an updated report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Anesthesiology. 2007;106(4):843-863.
- D’Alessio JG, Rosenblum M, Shea KP, et al. A retrospective comparison of interscalene block and general anesthesia for ambulatory surgery shoulder arthroscopy. Reg Anesth. 1995;20(1):62-68.
- Helwani MA, Avidan MS, Ben Abdallah A, et al. Effects of regional versus general anesthesia on outcomes after total hip arthroplasty: a retrospective propensity-matched cohort study. J Bone Joint Surg Am. 2015;97(3):186-193.
- Basques BA, Toy JO, Bohl DD, et al. General compared with spinal anesthesia for total hip arthroplasty. J Bone Joint Surg Am. 2015;97(6):455-461.
- Block BM, Liu SS, Rowlingson AJ, et al. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003;290(18):2455-2463.
- Nimmo SM, Harrington LS. What is the role of epidural analgesia in abdominal surgery? Contin Educ Anaesth Crit Care Pain. 2014;14(5):224-229.
- Freise H, Van Aken HK. Risks and benefits of thoracic epidural anaesthesia. Br J Anaesth. 2011;107(6):859-868.
- Manion SC, Brennan TJ. Thoracic epidural analgesia and acute pain management. Anesthesiology. 2011;115(1):181-188.
- Taras JS, Behrman MJ. Continuous peripheral nerve block in replantation and revascularization. J Reconstr Microsurg. 1998;14(1):17-21.
- Su HH, Lui PW, Yu Cl, et al. The effects of continuous axillary brachial plexus block with ropivacaine infusion on skin temperature and survival of crushed fingers after microsurgical replantation. Chang Gung Med J. 2005;28(8):567-574.
- Li J, Karmakar MK, Li X, et al. Regional hemodynamic changes after an axillary brachial plexus block: a pulsed-wave doppler ultrasound study. Reg Anesth Pain Med. 2012;37(1):111-118.
- Gadsden J. Regional Anesthesia in Trauma: A Case-Based Approach. New York, NY: Cambridge University Press; 2012.
- Bird TM, Strunin L. Anaesthetic considerations for microsurgical repair of limbs. Can Anaesth Soc J. 1984;31(1):51-60.
- Klock PA. The role of awake intubation. In: Glick DB, Cooper RM, Ovassapian A, eds. The Difficult Airway. New York, NY: Springer; 2013:33-46.
- Pani N, Kumar Rath S. Regional & topical anaesthesia of upper airways. Indian J Anaesth. 2009;53(6):641-648.
- Leslie D, Stacey M. Awake intubation. Contin Educ Anaesth Crit Care Pain. 2015;15(2):64-67.
- Pintaric TS. Upper airway blocks for awake difficult airway management. Acta Clin Croat. 2016;55(Suppl 1):85-89.
- Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92(5):1229-1236.
- Crawley SM, Dalton AJ. Predicting the difficult airway. Contin Educ Anaesth Crit Care Pain. 2015;15(5):253-257.
- Vasudevan A, Badhe AS. Predictors of difficult intubation—a simple approach. Internet J Anesthesiol. 2008;20(2).
- Kendale S. Difficult Intubation and various tools. In: Atchabahian A, Gupta R, eds. The Anesthesia Guide. New York, NY: McGraw-Hill Education; 2013:206-213.
- Asai T, Latto IP, Muthuswamy D, et al. Equipment list for difficult airway management. Anaesthesia. 2004;59(9):922.