BACKGROUND
Food bolus impaction and foreign object ingestion are aberrant clinical conditions that often require urgent intervention including endoscopy with either a push or retrieval technique.1 Patients presenting with foreign body ingestion or impaction may subsequently develop catastrophic sequelae such as gastrointestinal perforation, bleeding, or ulceration.2 In children, the most common objects ingested are coins, toys, magnets, and batteries, while in adults, bone or meat bolus impaction is the most common presenting pathology.3 Patient populations presenting with foreign object ingestion frequently include children, psychiatric patients, and prisoners, whereas food bolus impaction more commonly occurs in elderly patients with baseline esophageal pathology.4 Food impactions tend to be more common in males, and the most common associated pathologies are esophagitis, esophageal strictures and hiatal hernias, with more than half of boluses located in the lowest third of the esophagus.5 In contrast, foreign bodies are often lodged in the upper two thirds of the esophagus.6,7 Whereas foreign bodies in the upper portion of the esophagus pose additional risks including the inability to clear secretions and possible damage to the airway, potential sequelae of lower esophageal obstruction include esophageal erosion, mucosal damage, foreign body sensation, odynophagia, and sialorrhea.8 The level of risk to the patient ranges from minimal to life threatening depending on the ingested object or food, location, patient’s underlying pathology, and time to treatment.8
Endoscopic retrieval or manipulation of food boluses or foreign objects in patients that suffer from acute obstruction has been shown to have high success rates, lower incidence of minor complications, and a reduction in the need for surgery or hospitalization.9-12 The rate of complications increases with longer duration of obstruction and size/type of foreign body.13,14 For example, a sharp pointed food impaction has a higher risk of causing esophageal perforation and would benefit from early endoscopic intervention.15,16 Patients often present with dysphagia, odynophagia, vomiting and/or feelings of choking and gagging. Progression of an impaction or ingestion to an obstruction can lead to airway compromise, the inability to tolerate secretions, and even death.16
Various tools are used in conjunction with endoscopy to retrieve food or foreign bodies including baskets, retrieval forceps, polypectomy, snares and nets. It is important to note that foreign body impaction in the esophagus may be treated with flexible or rigid endoscopy, and the former technique often requires no anesthesia.17
ANESTHESIA FOR ENDOSCOPY
Sedation standards and practices for gastrointestinal endoscopy vary greatly between institutions, and in different legal jurisdictions. Sedation may be provided by the anesthesiology team or nonanesthesia personnel, including nurses and gastroenterologists.18 Routinely used medications include titratable intravenous sedative-hypnotic agents, benzodiazepines, and opioids.
The 2018 guidelines released by the American Society for Gastrointestinal Endoscopy (ASGE) outline standards of care for patients undergoing procedures under the supervision of interventional gastroenterologists.19 Sedation may be conducted by nonanesthesia professionals ranging from topical anesthetic with minimal or no intravenous medication to moderate sedation with propofol and other intravenous medications (in locations where nonanesthesia professional administered propofol [NAAP] is sanctioned).20 Nonetheless, the ASGE guidelines reports that anesthesia professional-administered sedation for endoscopy yields improved patient satisfaction, decreased distractions for the endoscopist, and increased procedure volume in the endoscopy unit because of shorter sedation and recovery times. Therefore, it is unsurprising that anesthesia services are frequently requested for endoscopic procedures, especially for endoscopic retrieval of a food bolus or foreign object.
CHOICE OF ANESTHETIC FOR FOOD BOLUS IMPACTION/FOREIGN OBJECT INGESTION
The optimal anesthetic technique for gastrointestinal procedures has long been debated with inconclusive results regarding superiority of one modality over another.21 When it comes to endoscopic removal of a foreign body or food bolus, the risk of aspiration during endoscopic manipulation is a critical concern for anesthesia professionals and should significantly influence the choice of anesthetic technique utilized. Nonetheless, these procedures are frequently performed using sedation instead of General Anesthesia (GA) with an endotracheal tube to secure the airway. There are risks and benefits to both GA and Monitored Anesthesia Care (MAC), though past literature is inconclusive regarding the superior approach. In one retrospective analysis, no difference in adverse events was found between conscious sedation using nonanesthesia personnel versus MAC and GA provided by anesthesia personnel.21 In this analysis, the most commonly occurring complications were surgical, including mucosal laceration and bleeding, while aspiration occurred much less frequently. Interestingly, though not surprising, 5.6% of their patient cohort could not tolerate conscious sedation, and required conversion to anesthesia professional-guided MAC or GA. In another study, there was no difference in therapeutic results for patients undergoing endoscopic management of foreign bodies between GA and topical pharyngeal anesthesia.22
It is critically important for anesthesia professionals to make a preoperative assessment regarding the presence or absence of a full stomach when considering intubation in all cases—a determination that may be complicated or obscured when managing a patient with food bolus impaction or foreign object ingestion. Generally, aspiration is more likely to occur when there is sufficient volume in the stomach for regurgitation, the lower esophageal sphincter is unable to protect the patient from retrograde movement of gastric contents, and upper airway reflexes are absent or blunted.23 During endoscopic retrieval of a food bolus or foreign object under anesthesia, many or all of these conditions are likely present, categorically increasing the potential risk for aspiration. General anesthesia with an endotracheal tube is likely the safest option for perioperative care of patients suffering from both food bolus impaction and foreign body ingestion, and great care should be taken to consider deviation from this choice of anesthetic. After a thorough examination of the patient, assessment of the gastrointestinal status and discussion with the gastroenterologist/proceduralist, however, consideration may be given to other anesthetic options, as discussed below (though the option to convert to a secure airway with an endotracheal tube must always be available).
CHOOSING A SAFE ANESTHESIA PLAN
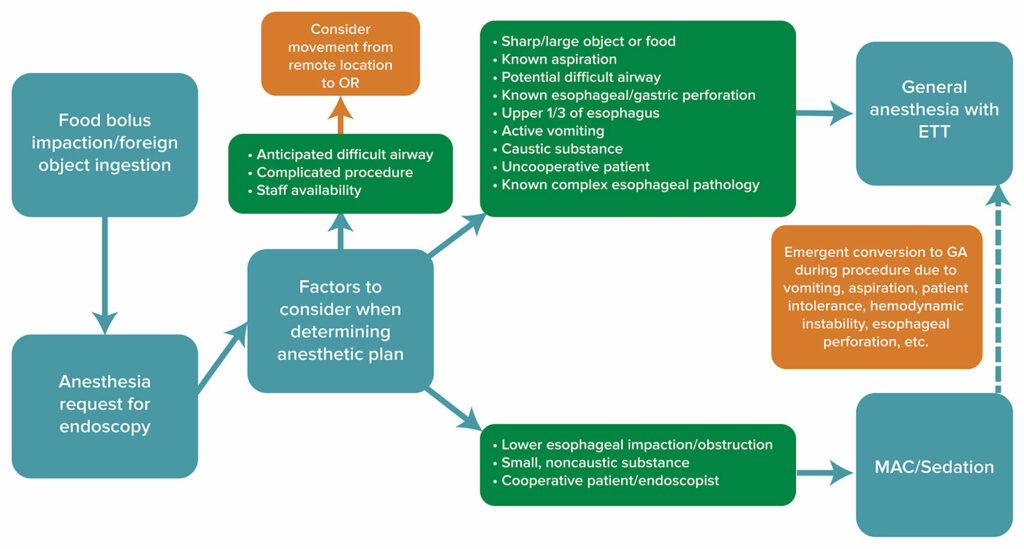
It is not clear if anesthesia professionals should routinely intubate for endoscopic removal of foreign bodies or food impaction. Certain situations may offer clear direction, but many circumstances are unique and require individualized assessment (Figure 1). If a patient has an obstruction or foreign body in the proximal esophagus, a secured airway may improve patient safety. Other situations that may prompt intubation include factors impacting the technical difficulty of retrieval and longer procedure duration such as ingestion of a caustic material, or exceedingly large or sharp foreign bodies; pediatric or combative patients; history of abnormal esophageal or gastric anatomy; or active or recent nausea and vomiting.24 Anticipated complicated procedures and morbidly obese patients with a difficult airway may require care in the operating room in order to have access to advanced anesthesia and surgical equipment along with additional personnel to help if need arises.25
Figure 1: Algorithm for decision-making regarding the anesthetic care of a patient presenting for endoscopy with either food bolus impaction or foreign object ingestion. Consideration should be given to factors such as airway exam, procedure type, staffing, and logistics to determine anesthetic technique and proper setting for procedure. MAC: monitored anesthesia care, GA: general anesthesia, ETT: endotracheal tube
In contrast, patients with suspected, but not confirmed, ingestion may be candidates for sedation. Patients who have radiographic confirmation of an object or food bolus that is in the distal esophagus and those with limited or no comorbidities, may demonstrate a trait profile that increases the likelihood of receiving sedation for the procedure.26 Further considerations that may prompt use of sedation include absence of recent vomiting, small sized object/food bolus, dull object, good patient compliance or willingness to agree with a sedation plan of minimal to moderate sedation, and provider/patient preference.9
Considerations related to surgical technique may also impact anesthetic choice. For example, cap-assisted endoscopy (which uses a cap fitted to the end of the scope to depress mucosal folds and improve visualization) for treatment of food bolus impaction or foreign body ingestion has been shown to have increased rate of treatment success and shorter procedure time, which may increase willingness of the anesthesia professional to utilize a sedation anesthetic technique.27,28 Sedation may also be preferred in nonurgent endoscopies, such as those recommended for medium sized blunt objects, which may be delayed up to 72 hours from the time of initial ingestion.24 Further, the use of such devices as an overtube, a device through which an endoscope is inserted, may help to reduce the risk of aspiration and mucosal injury, and may also influence decision-making by the anesthesia professional.29,30 The overtube serves to protect gastrointestinal mucosa from trauma and decreases the risk of aspiration by providing an occlusive conduit from the esophagus to outside the oral cavity.29,31
An important consideration prior to anesthetic care for endoscopy for food bolus impaction and foreign object ingestion is logistics of the treatment facility. Often, these procedures are performed in the emergency room, gastrointestinal procedure suite, hospital bed, or other remote location outside of the operating room. This limitation introduces such complicating factors as space constraints, difficulty accessing the patient’s head, poor lighting, limited monitoring, lack of advanced airway equipment, lack of experienced ancillary staff, and inadequate communication with personnel involved in patient care.32 Past literature has shown that emergency airway management outside of the operating room can be challenging and increases the risk of adverse events.32 Patients with anatomic variants, poor functional reserve and high risk for aspiration who present for emergency endoscopy likely should be moved to the operating room and should undergo GA with an endotracheal tube to limit risk of such adverse events.32 Successful anesthesia for endoscopic procedures in remote locations requires adequate monitoring equipment, devices for delivering anesthetic agents, and the ability to oxygenate, as well as a thorough understanding of the surgical procedure and its associated invasiveness.33
SPECIAL SAFETY CONSIDERATIONS
Communication
Effective communication is essential for the safe perioperative care of patients undergoing endoscopy for retrieval of a food bolus or foreign object. This includes communication with the proceduralist, patient, family members, nursing staff, technologists, and administrative personnel. It is necessary to ensure proper communication to facilitate timely care, confirm available resources, and coordinate care between preoperative, intraoperative, and postoperative staff, as well as the patient’s primary care service in the medical facility. When the decision has been made to proceed with MAC in a remote location, the anesthesia professional must ensure that the equipment and personnel are in place to convert to general anesthesia whenever required by the patient’s medical condition. In addition, given the potential for encountering a difficult airway (especially in a remote location), equipment such as video laryngoscopes, fiberoptic bronchoscopes, and intubating LMAs should be available to assist with the intubation.
Postoperative Care
The anesthesia professional must also pay special attention to the postoperative disposition of the patient afflicted with a foreign object or food bolus impaction. Due to the possible complications of both conditions affecting the gastrointestinal tract, these patients are at increased risk of such events as esophageal or gastric perforation, gastrointestinal bleeding, and aspiration. These potentially catastrophic sequelae necessitate close monitoring by qualified personnel for signs such as hypoxemia, wheezing, and hemodynamic instability. Ancillary services should also be available for patients such as thoracic surgery for treatment of esophageal perforation causing pneumomediastinum or esophageal rupture. In addition, critical care services should be available for patients who suffer systemic compromise requiring elevated and invasive support.
CONCLUSION
There is no uniform approach to anesthetic care for endoscopic procedures to treat food bolus impaction or foreign object ingestion. One must consider numerous factors prior to initiating care of these patients, and effective communication with the patient, endoscopist, and ancillary staff is extremely important. Proper planning is necessary when the procedure is conducted in a remote location along with backup plans in place for some of the potential complications such as failed endoscopist-administered sedation, aspiration or airway obstruction, or procedural complications such as perforated esophagus requiring surgical intervention. Nonetheless, these procedures may be safely performed if the anesthesia team utilizes a systematic approach to evaluate and treat these patients, such as the framework proposed by the authors.
REFERENCES
- Schupack DA, Lenz CJ, Geno DM, et al. The evolution of treatment and complications of esophageal food impaction. United European Gastroenterol J. 2019;7:548–556. PMID: 31065372
- Selivanov V, Sheldon GF, Cello JP, Crass RA. Management of foreign body ingestion. Ann Surg. 1984;199:187–191. PMID: 6696536
- Sugawa C, Ono H, Taleb M, Lucas CE. Endoscopic management of foreign bodies in the upper gastrointestinal tract: a review. World J Gastrointest Endosc. 2014;6:475–481. PMID: 25324918
- Magalhães-Costa P, Carvalho L, Rodrigues JP, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: an evidence-based review article. GE Port J Gastroenterol. 2016;23:142–152. PMID: 28868450
- Katsinelos P, Kountouras J, Paroutoglou G, et al. Endoscopic techniques and management of foreign body ingestion and food bolus impaction in the upper gastrointestinal tract: a retrospective analysis of 139 cases. J Clin Gastroenterol. 2006;40):784–789. PMID: 17016132
- Hong KH, Kim YJ, Kim JH, et al. Risk factors for complications associated with upper gastrointestinal foreign bodies. World J Gastroenterol. 2015;21:8125–8131. PMID: 26185385
- Gurala D, Polavarapu A, Philipose J, et al. Esophageal food impaction: a retrospective chart review. Gastroenterology Res. 2021;14:173–178. PMID: 34267832
- Fung BM, Sweetser S, Wong Kee Song LM, Tabibian JH. Foreign object ingestion and esophageal food impaction: an update and review on endoscopic management. World J Gastrointest Endosc. 2019;11:174–192. PMID: 30918584
- Geraci G, Sciume C, Di Carlo G, et al. Retrospective analysis of management of ingested foreign bodies and food impactions in emergency endoscopic setting in adults. BMC Emerg Med. 2016;16:42. PMID: 27809769
- Zhang X, Jiang Y, Fu T, et al. Esophageal foreign bodies in adults with different durations of time from ingestion to effective treatment. J Int Med Res. 2017;45:1386–1393. PMID: 28606025
- Mosca S, Manes G, Martino R, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: report on a series of 414 adult patients. Endoscopy. 2001;33:692–696. PMID: 11490386
- Park JH, Park CH, Park JH, et al. [Review of 209 cases of foreign bodies in the upper gastrointestinal tract and clinical factors for successful endoscopic removal]. Korean J Gastroenterol. 2004;43:226–233. PMID: 15100486
- Sung SH, Jeon SW, Son HS, et al. Factors predictive of risk for complications in patients with oesophageal foreign bodies. Dig Liver Dis. 2011;43:632–635. PMID: 21466978
- Liu Q, Liu F, Xie H, et al. Emergency removal of ingested foreign bodies in 586 adults at a single hospital in China according to the European Society of Gastrointestinal Endoscopy (ESGE) recommendations: a 10-year retrospective study. Med Sci Monit. 2022;28:e936463. PMID: 35879885
- Li G, Wu D, Zhou L, et al. Delayed endoscopic management of esophageal sharp-pointed food impaction: an analysis of 829 cases in China. Dig Dis Sci. 2022;67:3166–3176. PMID: 34342753
- Long B, Koyfman A, Gottlieb M. Esophageal foreign bodies and obstruction in the emergency department setting: an evidence-based review. J Emerg Med. 2019;56:499–511. PMID: 30910368
- Gmeiner D, von Rahden BH, Meco C, et al. Flexible versus rigid endoscopy for treatment of foreign body impaction in the esophagus. Surg Endosc. 2007;21:2026–2029. PMID: 17393244
- Amornyotin S. Sedation and monitoring for gastrointestinal endoscopy. World J Gastrointest Endosc. 2013;5:47–55. PMID: 23424050
- Early DS, Lightdale JR, Vargo JJ, 2nd, et al. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018;87:327–337. PMID: 29306520
- Vargo JJ, Cohen LB, Rex DK, Kwo PY. Position statement: nonanesthesiologist administration of propofol for GI endoscopy. Gastroenterology. 2009;137:2161–2167. PMID: 19961989
- Cha MH, Sandooja R, Khalid S, et al. Complication rates in emergent endoscopy for foreign bodies under different sedation modalities: a large single-center retrospective review. World J Gastrointest Endosc. 2021;13:45–55. PMID: 33623639
- Geng C, Li X, Luo R, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: a retrospective study of 1294 cases. Scand J Gastroenterol. 2017;52:1286–1291. PMID: 28691540
- Engelhardt T, Webster NR. Pulmonary aspiration of gastric contents in anaesthesia. Br J Anaesth. 1999;83:453–460. PMID: 10655918
- Birk M, Bauerfeind P, Deprez PH, et al. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:489–496. PMID: 26862844
- Lin OS, Weigel W. Nonoperating room anesthesia for gastrointestinal endoscopic procedures. Curr Opin Anaesthesiol. 2018;31:486–491. PMID: 29781859
- Pfau PR. Removal and management of esophageal foreign bodies. Techniques in Gastrointestinal Endoscopy. 2014;16:32–39. doi:https://doi.org/10.1016/j.tgie.2013.10.004
- Mohan BP, Bapaye J, Hamaad Rahman S, et al. Cap-assisted endoscopic treatment of esophageal food bolus impaction and/or foreign body ingestion: a systematic review and meta-analysis. Ann Gastroenterol. 2022;35:584–591. PMID: 36406971
- Abdelhafez M, Phillip V, Hapfelmeier A, et al. Cap assisted upper endoscopy for examination of the major duodenal papilla: a randomized, blinded, controlled crossover study (CAPPA Study). Am J Gastroenterol. 2017;112:725–733. PMID: 28291239
- Kim SH. Usefulness of an overtube device in gastrointestinal endoscopy. Clin Endosc. 2019;52:203–204. PMID: 31154698
- Ofosu A, Ramai D, Reddy M. Overtube-assisted foreign body removal: a review of endoscopic management and case illustration. Cureus. 2017;9:e1730. PMID: 29201579
- Tierney WM, Adler DG, Conway JD, et al. Overtube use in gastrointestinal endoscopy. Gastrointest Endosc. 2009;70:828–834. PMID: 19703691
- Jarzebowski M, Estime S, Russotto V, Karamchandani K. Challenges and outcomes in airway management outside the operating room. Curr Opin Anaesthesiol. 2022;35:109–114. PMID: 35102045
- Pardo E, Camus M, Verdonk F. Anesthesia for digestive tract endoscopy. Curr Opin Anaesthesiol. 2022;35:528–535. PMID: 35787532