Author: Chase Doyle
Anesthesiology News
Balancing the goals of analgesia with early ambulation after total knee arthroplasty has led to increasingly selective regional analgesia that can sometimes fail to provide optimal pain control. However, recent analysis suggests that adding the iPACK (Infiltration between the Popliteal Artery and Capsule of the Knee) block may offer patients improved pain control with earlier ambulation.
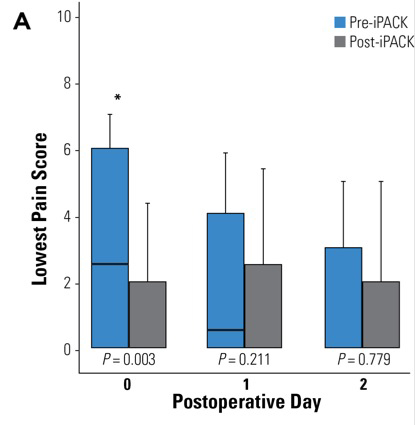
A retrospective analysis of pain outcomes in patients undergoing total knee arthroplasty before and after implementation of iPACK at a single institution showed patients’ lowest reported pain on the day of surgery was lower among those receiving adductor canal plus iPACK blocks versus an adductor canal block alone. Although the results showed relatively limited benefits in terms of pain scores outside this measure, researchers noted that these early benefits in pain relief could translate into improvements in ambulation with deployment of additional resources.
Dr. Mariano, who is a member of the Anesthesiology News editorial advisory board, reported that there has been a gradual focus on the regional analgesic technique over the years, moving away from epidural analgesia toward peripheral nerve blocks that isolate the operative leg and, more recently, even further selectivity. However, with greater sparing of the nerve, said Dr. Mariano, comes an inability to provide the same level of pain control.
For the iPACK block, a high-frequency ultrasound transducer was used to visualize the popliteal artery and posterior surface of the distal femoral shaft after adductor canal catheter insertion. Using an in-plane approach, a 20-gauge Tuohy needle was inserted from medial to lateral to position the needle tip between the popliteal artery and femur, at which point 20 mL of 0.2% ropivacaine were injected.
For this study, Dr. Mariano and his colleagues retrospectively reviewed data for consecutive patients undergoing total knee arthroplasty by a single surgeon four months before and after iPACK implementation. All patients received adductor canal catheters and perioperative multimodal analgesia. The primary outcome was pain on postoperative day 0 (POD 0). Secondary outcomes included daily pain scores, opioid consumption, ambulation distance, length of stay and 30-day adverse events.
Improved Analgesia on Day of Surgery
As Dr. Mariano reported at the 2019 annual meeting of the American Society of Regional Anesthesia and Pain Medicine, the final cohort included 80 patients (n=32 before and n=48 after iPACK implementation).
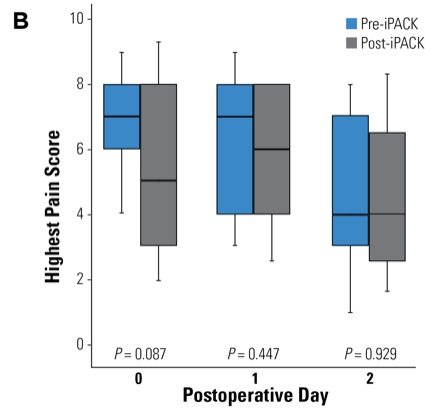
With respect to the primary outcome, patient-reported pain scores on POD 0, the lowest pain score was lower for patients receiving iPACK plus adductor canal blocks versus an adductor canal block alone (Figure). However, the highest patient-reported pain scores on POD 0, as well as other lowest and highest pain scores through POD 2, were not significantly different between the two groups, Dr. Mariano reported.
Although total opioid consumption on POD 0 was lower in patients receiving iPACK plus adductor canal blocks compared with an adductor canal block alone (34 morphine milligram equivalents [MME] vs. 47 MME), the difference was not statistically significant (P=0.166). As Dr. Mariano explained, however, given the robust multimodal analgesic regimen already in place, it is becoming increasingly difficult to demonstrate reductions in inpatient opioid use.
“Opioid consumption for our joint replacement patients is at an all-time low, which makes it harder to find not just statistically significant but clinically meaningful differences in opioid use with just one tweak of our multimodal regimen,” he said.
Despite the benefit in pain relief on POD 0, the authors also observed no improvements in ambulation. According to Dr. Mariano, however, this result is not a failure of the iPACK technique but rather a reflection of the need to improve enhanced recovery protocols at his institution.
“We’ve taken the data from this study to our administration to hire additional physical therapy personnel to help mobilize our patients on the day of surgery,” Dr. Mariano said. “We now have evidence to show that pain relief can be accomplished with our current techniques, but in order to actually maximize our patients’ physical function, we have to test them.”
Convinced That iPACK Block Adds Value
David H. Kim, MD, an anesthesiologist at the Hospital for Special Surgery, in New York City, told Anesthesiology News that his hospital has included the iPACK block as a standard of care for total knee arthroplasty and unicompartmental knee arthroplasty pathways based on evidence of improved analgesia.
“We are convinced that the iPACK block has added value to our already robust multimodal total knee arthroplasty pathway,” Dr. Kim said. “What we have found in our prospective randomized controlled trial is that the iPACK block has significantly lowered pain on ambulation—not just at rest—and lowered opioid consumption up to 24 hours.
“Facilitating mobility by augmenting analgesia via motor-sparing blocks has remained a significant clinical goal among our surgeons and anesthesiologists, especially when early ambulation has been linked to shorter length of stay,” Dr. Kim continued. “However, we do feel that it is always good to replicate our findings in different settings to make sure iPACK adds value.”