Author: Michael Vlessides
Anesthesiology News
In patients with trismus, flexible fiber-optic intubation can be accomplished through the retromolar space, according to a new study. The researchers also noted an association between increasing body mass index (BMI) and decreasing size of the retromolar space.
“Patients with head and neck cancers often present with trismus—they can’t open their mouths,” said Angela T. Truong, MD, one of the researchers and a professor of anesthesiology and perioperative medicine at the University of Texas MD Anderson Cancer Center, in Houston. “Obviously, this is a problem when it comes to intubation.
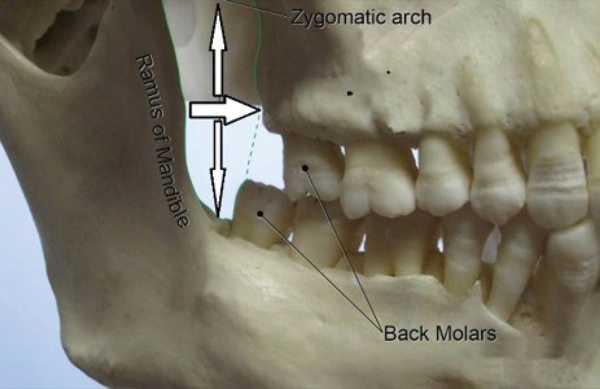
“We know that the retromolar space exists and often use it, such as to suction when a patient emerges from anesthesia with their teeth clenched,” she said. “Nevertheless, a lot of anesthesiologists don’t think of it. So, our goal in this study was to measure the space and see if we could use it to intubate patients using a flexible fiber-optic scope” (Figure 1). Although dental pantomograms (panoramic radiographs) have previously been used to measure the retromolar space, these measurements did not account for soft tissue overlying the space, leading the authors to use putty molds to determine if the space can readily accommodate tracheal tubes.
Trismus is defined as a restricted mouth opening that measures less than 35 mm interincisal distance, and severe trismus is an interincisal distance less than 10 mm. “Normal mouth opening should be about 50 mm,” Dr. Truong said. Nasal intubation and tracheostomy have traditionally been performed in patients with trismus, but both options are invasive and associated with potential complications.
The researchers enrolled 80 healthy volunteers from four ethnic groups into the trial: 20 white, 20 black, 20 Hispanic and 20 Asian (with 10 men and 10 women in each group). Participants were excluded from the study if they were edentulous, had previous surgery causing anatomic distortion of the mandible, could not completely clench their teeth, or had an impaired gag reflex.
Silicone putty molds of the left and right retromolar spaces were made at maximum intercuspation for each participant, then scanned with CT and spaces measured directly from the scans (Figure 2). Demographic and clinical data were recorded, including age, sex, ethnicity, height, weight, BMI and the number of molars present on each side.
“There was only one study investigator who inserted the molds into participants’ mouths. This same person made the measurements directly from the scans,” Dr. Truong noted.
Retromolar Versus Nasal Intubation
At the 2018 annual meeting of the Canadian Anesthesiologists’ Society, Dr. Truong reported the widths and heights of the retromolar spaces in men, women and the group as a whole (abstract 431504) (Table).
| Table. Clinical Characteristics of Patients With Trismus | ||||
| Women, n=40 | Men, n=40 | P Valuea | Total, N=80 | |
|---|---|---|---|---|
| Age, years | ||||
| Mean ± SD | 40.13±11.42 | 43.75±11.61 | 0.172 | 41.94±11.59 |
| Median (range) | 37.5 (23-65) | 44.5 (24-74) | 39.5 (23-74) | |
| BMI, kg/m2 | ||||
| Mean ± SD | 26.15±5.75 | 27.79±3.91 | 0.023 | 26.97±4.96 |
| Median (range) | 24.83 (20.36-43.85) | 26.83 (19.5-35.73) | 25.84 (19.5-43.85) | |
| Right Side | ||||
| Width of Right RS, mm | ||||
| Mean ± SD | 8.69±2.17 | 9.42±3.74 | 0.751 | 9.05±3.06 |
| Median (range) | 8.82 (4-14.49) | 8.7 (4.42-18.4) | 8.82 (4-18.4) | |
| Height of Right RS, mm | ||||
| Mean ± SD | 5.66±2.06 | 5.8±2.04 | 0.788 | 5.73±2.04 |
| Median (range) | 5.71 (1.79-9.51) | 5.61 (2.43-9.67) | 5.61 (1.79-9.67) | |
| Left Side | ||||
| Width of Left RS, mm | ||||
| Mean ± SD | 8.69±2.37 | 9.21±4.04 | 0.470 | 8.95±3.3 |
| Median (range) | 8.43 (3.22-14.33) | 7.75 (4.4-23.2) | 8.02 (3.22-23.2) | |
| Height of Left RS, mm | ||||
| Mean ± SD | 6.09±1.86 | 6.21±1.69 | 0.874 | 6.15±1.77 |
| Median (range) | 6.17 (2-9.6) | 6.21 (2.91-9.6) | 6.16 (2-9.6) | |
|
a By Wilcoxon rank-sum test.
BMI, body mass index; RS, retromolar space |
||||
Linear regression analysis was used to assess the association between BMI and retromolar space dimensions, with adjustment for age, sex and ethnicity. There was a statistically significant decrease in the height (P=0.011) and width (P=0.012) of the space for every unit increase in BMI. Given this relationship, the researchers noted that retromolar intubation may not be feasible in obese patients.
The researchers noted that the study was limited by a relatively small number of participants and the potential inability of the silicone putty to maximally displace soft tissue. Although the outer diameter of a 6.0-mm endotracheal tube is 8.4 mm, the mean space height fell below this value, suggesting that compressible soft tissues may account for successful retromolar intubation in these individuals. “I’ve been intubating patients with trismus using the retromolar space, and I have been successful in placing a 6.0-mm tube in these individuals,” Dr. Truong said.
“Could you use nasal-tracheal intubation in these patients?” asked Sumitra G. Bakshi, MB BS, MD, an attending anesthesiologist at Tata Memorial Hospital in Mumbai, India.
“Some people have complete occlusion,” Dr. Truong replied. “In these cases, many clinicians will do a nasal intubation. The problem with nasal intubation is that there are often contraindications, such as nasal stenosis, history of basilar skull fractures, coagulopathy or proposed surgery involving the nasal passages. Flexible fiber-optic retromolar intubation becomes a valuable technique in these special cases, in which nasal intubation is simply not a viable option.”
Although session moderator Mahesh Nagappa, MD, prefers nasal intubation when oral intubation is contraindicated, he saw the value of retromolar intubation in certain circumstances. “Usually we opt for nasal intubation in patients who can’t open the mouth at all,” said Dr. Nagappa, an assistant professor of anesthesia and perioperative medicine at Western University’s Schulich School of Medicine & Dentistry, in London, Ontario. “But if there is any difficulty or contraindications in using the nasal orifice, I can see how retromolar intubation can be one of the possibilities. But in my clinical practice over the past 15 years, I have never seen unsuccessful nasal intubation when the oral route is contraindicated,” he said.



Leave a Reply
You must be logged in to post a comment.