Anesthesia professionals have consistently been leaders in patient safety and have long recognized the importance of hand hygiene in the anesthesia workspace.1 Hand contamination is associated with pathogen transmission across multiple anesthesia workspace reservoirs, and genome analysis of bacteria cultured from provider hands and infection causing pathogens have confirmed that providers transmit pathogens that result in patient infections.2,3,4 Staphylococcus aureus (S. aureus) transmission among anesthesia workspace reservoirs is associated with an increased risk of surgical site infection (SSI).5 In fact, SSI risk increases over fivefold when the pathogens are sensitive to the prophylactic antibiotic employed and ninefold when the pathogens are resistant to the prophylactic antibiotic employed.6 In order to reduce this risk, a multifaceted approach is indicated to prevent SSIs.7 When improved hand hygiene is incorporated as part of a multifaceted program, substantial reductions in S. aureus transmission and SSIs can be achieved.8,9 These findings should provide the impetus for widespread improvements in hand hygiene compliance for all intraoperative personnel, with anesthesia professionals taking the lead.
The anesthesia workspace is a complex environment that includes the patient, the surgical bed/table, the anesthesia machine, the intravenous (IV) pole(s) with attached infusion devices, a cart with clean supplies, and medications stored within the cart or a separate medication station. Anesthesia professionals interact with the patient and multiple components of the anesthesia workspace during routine anesthesia practice.10,11 Given the complexity of this environment, hand decontamination is necessary to interrupt transmission events and reduce infection propagation. The World Health Organization (WHO) defines events, after which hand hygiene should be performed as the, “Five Moments of Hand Hygiene.”12 These moments that call for hand hygiene arethe following: before touching a patient, before a clean or sterile procedure, after touching a patient, after a task with a body-fluid exposure risk, and after touching the patient’s surroundings (Figure 1).12 Compliance with WHO and similar recommendations would require the anesthesia professional to perform hand hygiene as often as 54 times per hour13 up to 150 times per hour.11,13 However, studies reveal that anesthesia professionals perform hand hygiene less than once per hour.14 Clearly, there is substantial opportunity for some improvement. It might seem that fighting against the transmission of pathogens is impossible, given how ubiquitous bacteria are in our environment. However, research suggests that reducing the levels of S. aureus on provider hands to less than 100 colony-forming units (CFU) is an achievable goal that can help to protect our patients.9,15
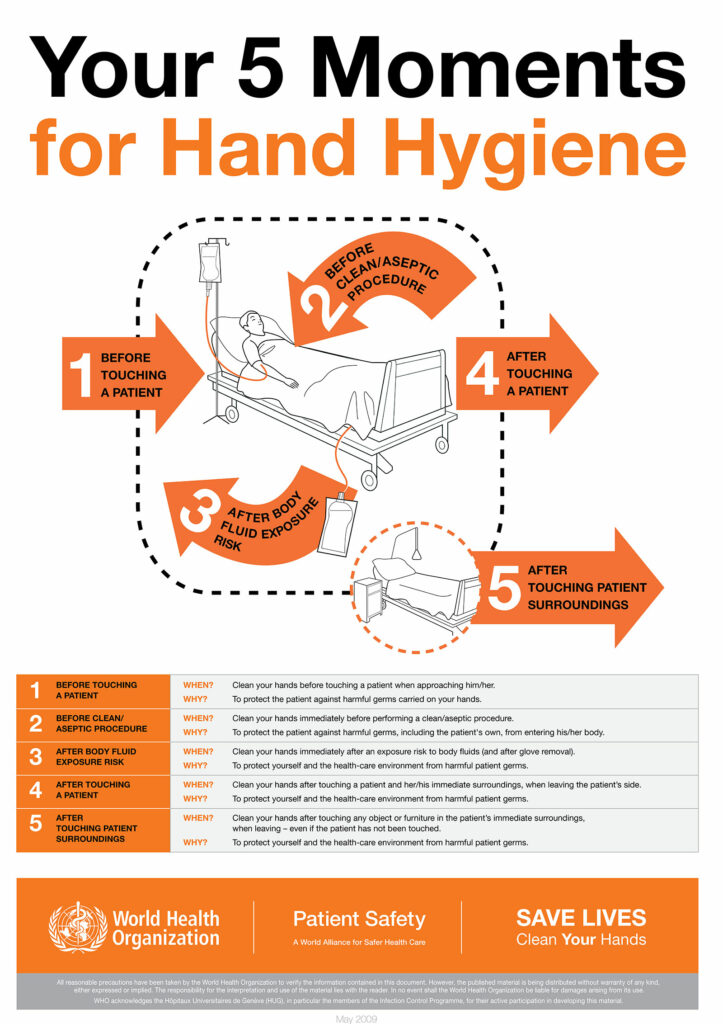
Figure 1: Your 5 Moments for Hand Hygiene. Geneva, Switzerland. World Health Organization. 2009. License: CC BY-NC-SA 3.0 IGO.
The APSF Patient Safety Priorities Advocacy Group: Infectious Disease recommends that anesthesia professionals perform hand hygiene at least approximately eight times per hour during anesthesia care.16 Washing one’s hands or using hand sanitizer at a frequency of eight times per hour optimally reduced environmental and stopcock contamination and subsequent infection development.14 However, the proper methodology to prompt hand hygiene compliance at this frequency is not clear.16 Important future research include products (e.g., alcohol-based or soap and water), dispenser locations, cleansing technique, and potential risks.
While hands can be effectively decontaminated using alcohol-based solutions, visibly contaminated hands or potential contact with spore-forming organisms should be decontaminated with soap and water.14,17 Since scrub sinks must be outside the operating room, alcohol is the primary hand hygiene option for anesthesia professionals, and because it is associated with less skin irritation than soap and water, it may reduce the risk of irritated skin and higher bacterial counts on the irritated skin.18,19
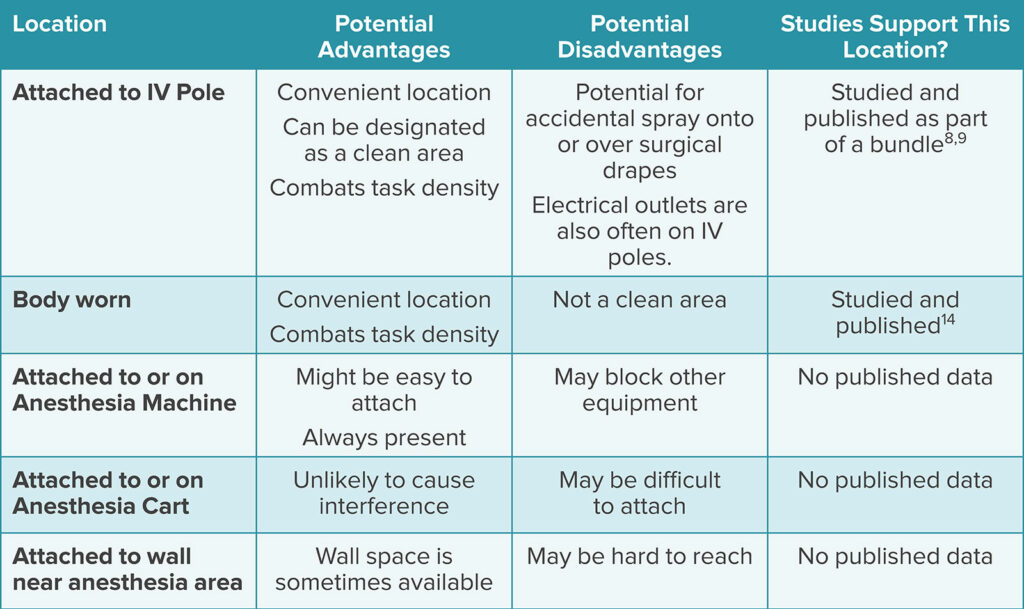
Dispenser locations should be determined by task density, which is the number of tasks that need to be done in a period of time. Health care infection prevention organizations recommend dispenser placement in locations that are easily accessible within the patient care arena.20 Using dispensers placed outside the anesthesia work area (e.g., on the wall or near the entrance to the operating room) may disrupt patient care. The importance of task density is well-delineated. In one study, anesthesia professional use of a personalized, body-worn alcohol dispenser increased hand hygiene compliance 37-fold, and, in turn, reduced the incidence of environmental and stopcock contamination and health care associated infections.14 Other investigators evaluated dispenser placement on the intravenous pole to the left of the provider as part of a multifaceted program.8,9 Dispenser placement in this location reduced the incidence of bacterial transmission and subsequent SSI development.8,9
Because provider hand contamination is associated with environmental contamination, improving the frequency and quality of environmental cleaning may also help to augment hand hygiene improvement efforts. In one study, separating the anesthesia workspace into “clean” and “dirty” areas was associated with a reduction in the proportion of sites reaching ≥ 100 CFUs.14,21 It is intuitive that alcohol dispensers should be placed in areas designated as clean. For example, the dispenser may be secured to the anesthesia machine or supply cart with a mounting rack, or on the intravenous pole. If secured to the intravenous pole, then caution should be taken to protect the patient, surgical field, and underlying electrical plugs from splashes and drips (Table 1).
Table 1: Potential Considerations for Hand Sanitizer Locations in the Anesthesia Workspace.
While anesthesia professionals must have ready access to a hand sanitizer, there are potential hazards to consider. All alcohol-based sanitizers contain 60–80% ethyl or isopropyl alcohol and water. This is because a sufficient water component is necessary to hydrolyze microorganism membranes and slow evaporation of the product.22,23 Because alcohol products are flammable, fire codes regulate the total volume of sanitizers allowed within a procedure room and the minimum separation distance between alcohol dispensers. Dispensers must be separated by a minimum distance of four feet, and their combined volume in one room must not exceed 1.2 liters.24 The Centers for Disease Control and Prevention also espouses these fire safety recommendations.25 The volume for personalized, body-worn alcohol dispensers and one-handed alcohol pumps on an IV pole is less than 3 ounces.8,9,14 While there have not been reports of fires related to hand sanitizers, it is risk worth considering.
In summary, improved hand hygiene by anesthesia professionals is an essential element of a multifaceted approach to reducing bacterial transmission and infection development. Eight hand hygiene events per hour during routine anesthesia care should be encouraged. Alcohol-based sanitizers in the anesthesia workspace should be placed in clean and easily accessible locations that are clearly visualized by the clinician.
REFERENCES
- Warner MA, Warner ME. The evolution of the anesthesia patient safety movement in America: lessons learned and considerations to promote further improvement in patient safety. Anesthesiology. 2021;135:963–974. PMID: 34666350
- Dexter F, Loftus RW. Estimation of the contribution to intraoperative pathogen transmission from bacterial contamination of patient nose, patient groin and axilla, anesthesia practitioners’ hands, anesthesia machine, and intravenous lumen. J Clin Anesth. 2024;92:111303. Epub 2023 Oct 22. PMID: 37875062.
- Loftus RW, Brindeiro CT, Loftus CP, et al. Characterizing the molecular epidemiology of anaesthesia work area transmission of Staphylococcus aureus sequence type 5. J Hosp Infect. 2024;143:186–194. Epub 2023 Jul 13. PMID: 37451409.
- Loftus RW, Brown JR, Koff MD, et al. Multiple reservoirs contribute to intraoperative bacterial transmission. Anesth Analg. 2012;114:1236–1248. Epub 2012 Mar 30. PMID: 22467892.
- Hopf, Harriet W. MD. Bacterial reservoirs in the operating room. Anesthesia & Analgesia. 2015;120:p 700–702. PMID: 25790198
- Loftus RW, Dexter F, Brown JR. Transmission of Staphylococcus aureus in the anaesthesia work area has greater risk of association with development of surgical site infection when resistant to the prophylactic antibiotic administered for surgery. J Hosp Infect. 2023;134:121–128. doi: 10.1016/j.jhin.2023.01.007. Epub 2023 Jan 21. PMID: 36693592.
- Dexter F, Brown JR, Wall RT, Loftus RW. The efficacy of multifaceted versus single anesthesia work area infection control measures and the importance of surgical site infection follow-up duration. J Clin Anesth. 2023;85:111043. Epub 2022 Dec 23. PMID: 36566648.
- Loftus RW, Dexter F, Goodheart MJ, et al. The effect of improving basic preventive measures in the perioperative arena on Staphylococcus aureus transmission and surgical site infections: a randomized clinical trial. JAMA Netw Open. 2020;3: e201934. PMID: 32219407
- Wall RT, Datta S, Dexter F, et al. Effectiveness and feasibility of an evidence-based intraoperative infection control program targeting improved basic measures: a post-implementation prospective case-cohort study. J Clin Anesth. 2022; 77:110632. Epub 2021 Dec 17. PMID: 34929497.
- Sharma A, Fernandez PG, Rowlands JP, et al. Perioperative infection transmission: the role of the anesthesia provider in infection control and healthcare-associated infections. Curr Anesthesiol Rep. 2020;10:233–241. Epub 2020 Jul 17. PMID: 32837343
- Rowlands J, Yeager MP, Beach M, et al. Video observation to map hand contact and bacterial transmission in operating rooms. Am J Infect Control. 2014;42:698–701. PMID: 24969122
- WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care. Geneva: World Health Organization; 2009. 21, The WHO Multimodal Hand Hygiene Improvement Strategy. Available from: https://www.who.int/publications/i/item/9789241597906. Accessed July 5, 2024
- Biddle C, Shah J. Quantification of anesthesia providers’ hand hygiene in a busy metropolitan operating room: what would Semmelweis think? Am J Infect Control. 2012;40:756–759. Epub 2012 Feb 9. PMID: 22325482.
- Koff MD, Loftus RW, Burchman CC, et al. Reduction in intraoperative bacterial contamination of peripheral intravenous tubing through the use of a novel device. Anesthesiology. 2009;110:978–985. PMID: 19352154.
- Dexter F, Walker KM, Brindeiro CT, et al. A threshold of 100 or more colony-forming units on the anesthesia machine predicts bacterial pathogen detection: a retrospective laboratory-based analysis. Can J Anaesth. 2024;71:600–610. English. Epub 2024 Feb 27. PMID: 38413516.
- Charnin JE, Hollidge M, Bartz R, et al. A best practice for anesthesia work area infection control measures: what are you waiting for? APSF Newsletter. 2022;37:103-106. https://www.apsf.org/article/a-best-practice-for-anesthesia-
work-area-infection-control-measures-what-are-you-waiting-for/ Accessed August 9, 2024. - WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care. Appendix 2. Guide to appropriate hand hygiene in connection with Clostridium difficile spread. https://www.ncbi.nlm.nih.gov/books/NBK144042/. Accessed May 29, 2024.
- Pedersen LK, Held E, Johansen JD, Agner T. Short-term effects of alcohol-based disinfectant and detergent on skin irritation. Contact Dermatitis. 2005;52:82–87. PMID: 15725285
- Larson EL, Hughes CA, Pyrek JD, et al. Changes in bacterial flora associated with skin damage on hands of health care personnel. Am J Infect Control. 1998;26:513–521. PMID: 9795681
- Glowicz JB, Landon E, Sickbert-Bennett EE, et al SHEA/IDSA/APIC practice recommendation: strategies to prevent healthcare-associated infections through hand hygiene: 2022 update. Infect Control Hosp Epidemiol. 2023;44:355–376. PMID: 36751708
- Clark C, Taenzer A, Charette K, Whitty M. Decreasing contamination of the anesthesia environment. Am J Infect Control. 2014 Nov;42(11):1223-5. Epub 2014 Oct 30. PMID: 25444268.
- Ali Y, Dolan MJ, Fendler EJ, Larson EL. Alcohols. In: Block SS, ed. Disinfection, sterilization, and preservation. Philadelphia: Lippincott Williams & Wilkins, 2001:229–254.
- Rutala WA, Weber DJ, and the Healthcare Infection Control Practices Advisory Committee. Guideline for disinfection and sterilization in healthcare facilities, 2008. https://stacks.cdc.gov/view/cdc/47378 Accessed August 9, 2024.
- National Fire Protection Association (NFPA). NFPA 101 Life Safety Code. 2018 edition. Quincy, MA: National Fire Protection Association; 2018. https://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-
and-standards/detail?code=101 Accessed August 9, 2024. - Centers for Disease Control and Prevention (CDC). Clinical safety: hand hygiene for healthcare workers – fire safety and Alcohol-Based Hand Sanitizer (ABHS). https://www.cdc.gov/clean-hands/hcp/clinical-safety/?CDC_AAref_Val=https://www.cdc.gov/handhygiene/firesafety/index.htm Accessed July 5, 2024.


Leave a Reply
You must be logged in to post a comment.