Clinical Vignette
DW is an anesthesia professional at a community hospital who takes call from home and just finished her last case at midnight. She was nodding off to sleep at 2:00 am when she was alerted by the OR front desk that she was needed to provide anesthesia for an elderly patient with a small bowel obstruction. Exhausted and less than enthusiastic about returning to the hospital, she met the patient in the holding area and went through the usual preoperative routine. The patient was frightened and apologized profusely to the operating room team that they all had to be called in to provide care in the middle of the night. DW reassured the patient that this was her job and that she spent many years training to do exactly this—to care for people that are ill and in pain, irrespective of the hour. The surgery proceeded without incident and in the recovery room, the patient was relieved and profoundly appreciative to the team for making it through surgery. DW recounted that when she left the hospital later that morning, she was exhausted yet invigorated and recharged from helping this frightened and distressed patient who benefited from her expertise. Despite her physical exhaustion, she was not upset or angry but felt connected to her colleagues and reaffirmed in her role as an anesthesia professional able to care for this patient during a time of great need.
The Current State
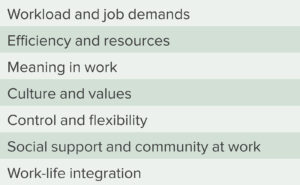
In October 2018, the APSF Newsletter described the trend of increasing burnout among anesthesia professionals.1 Burnout is a syndrome resulting from chronic and unmanaged workplace stress, characterized by decreasing work effort, cynicism, and low physical and emotional energy levels.2,3 Drivers of burnout can be divided into seven categories (see Table 1).3,4 While studies to characterize and combat burnout are occurring, the phenomenon continues to escalate. In 2014, burnout rates of 50% were reported among anesthesia professionals and continue to be cited as a perioperative patient safety priority in 2021.5,6 A survey conducted among members of the American Society of Anesthesiologists in March 2020 during the initial phases of the pandemic assessed burnout and demonstrated 59% were at high risk of burnout and nearly 14% met criteria for burnout syndrome.7 The AANA has identified a paucity of research on burnout among anesthesia professionals while underscoring the threat of contributing factors such as increasing emotional exhaustion.8
Barriers to Experiencing Connectedness
 The COVID-19 pandemic which is associated with an increase in the prevalence of burnout among health care workers, has exacerbated many of the factors which contribute to burnout.1,9 In a survey targeting the experiences of health care workers involved in the COVID-19 pandemic, 76% of respondents reported exhaustion and burnout and over one-third noted a lack of adequate emotional support.10 Common concerns included an increase in emotional exhaustion (82%), difficulty with sleep (70%), physical exhaustion (68%), and work-related dread (63%).10 A recent Washington Post article on the experiences of an anesthesiologist involved in airway management during COVID-19 compared the stress to working beside a nuclear reactor.11
The COVID-19 pandemic which is associated with an increase in the prevalence of burnout among health care workers, has exacerbated many of the factors which contribute to burnout.1,9 In a survey targeting the experiences of health care workers involved in the COVID-19 pandemic, 76% of respondents reported exhaustion and burnout and over one-third noted a lack of adequate emotional support.10 Common concerns included an increase in emotional exhaustion (82%), difficulty with sleep (70%), physical exhaustion (68%), and work-related dread (63%).10 A recent Washington Post article on the experiences of an anesthesiologist involved in airway management during COVID-19 compared the stress to working beside a nuclear reactor.11
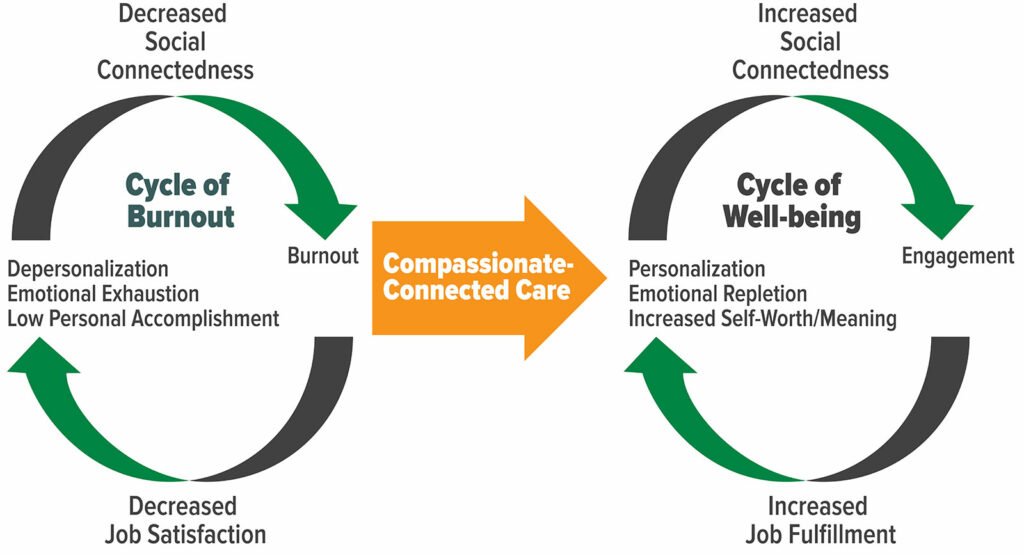
A perceived lack of support in the workplace has been identified as one of the most important factors contributing to burnout.7 In a pre-COVID environment, attempts to mitigate burnout at the institutional level included implementing tools such as flexible scheduling to enhance provider satisfaction, education for providers on the causes and symptoms of burnout, promotion of enhanced work-life integration, and providing resources to promote resilience and self-care.1,3 However, during the height of the pandemic, many health promotional activities such as exercising in a gym, connecting in-person with friends and family, or traveling were significantly curtailed leading individual health care providers to cope on their own. COVID-19 has only amplified the limitations of existing approaches. As we slowly emerge from the pandemic, what are more effective strategies to mitigate burnout and promote clinician well-being? (See Figure 1.)
Many frontline workers have intuitively discovered during this pandemic that compassionate-connected care can be an effective antidote to neutralize each of the three hallmarks of burnout: emotional exhaustion, lack of personal accomplishment, and depersonalization (Figure 1).12 The crux of the argument for compassionate care to mitigate burnout and enhance the anesthesia professional’s connection to their profession lies in the idea that while empathy is simply the recognition and understanding of someone’s pain and suffering, compassion is the “emotional response to another’s pain or suffering, involving an authentic desire to help.”13,14 In other words, compassion involves not just feeling someone else’s pain but taking the action to alleviate or eliminate it. By the very definition of the specialty of anesthesiology, anesthesia professionals are the experts at eliminating physiologic pain and suffering and derive satisfaction from seeing the direct impact of those actions in the service of others. These acts of compassionate care can be rejuvenating.
In addition to combatting burnout, the other benefits of compassionate care include improved patient safety, higher patient satisfaction, and even decreased cost of care.15-18 Expanding compassion in clinical practice can increase social connectedness that extends beyond our patients and includes our colleagues and coworkers. It is important to note that the factors that have contributed to burnout, are in fact the very same barriers that prevent clinicians from connecting to their patients. These barriers include spending nonnegotiable time on clerical and billing functions in the electronic health record (EHR), production pressure that leads to hurrying and not connecting with patients, and taking short cuts due to staffing shortages. Given these powerful benefits of compassionate care, we, in partnership with our institutions should work to eliminate the barriers and create systemic conditions that increase the ability of clinicians to connect with their patients and with each other.
Systemic Changes Foster Organizational Compassion
 To further mitigate burnout, health care institutions should foster a workplace culture of compassion to extend beyond patients and also include colleagues and coworkers. Strong interpersonal relationships are an important contributor to one’s physical and emotional well-being.19,20 In fact, strong human relationships may be a better predictor of one’s health than traditional markers such as lipid levels.15 Feeling connected both at home and at work can protect against burnout.7 Additionally, institutions play an important role in breaking the cycle of burnout and can be crucial in emphasizing a culture of compassion for colleagues and in helping one another cope with the stressors that exist in anesthesia practice.
To further mitigate burnout, health care institutions should foster a workplace culture of compassion to extend beyond patients and also include colleagues and coworkers. Strong interpersonal relationships are an important contributor to one’s physical and emotional well-being.19,20 In fact, strong human relationships may be a better predictor of one’s health than traditional markers such as lipid levels.15 Feeling connected both at home and at work can protect against burnout.7 Additionally, institutions play an important role in breaking the cycle of burnout and can be crucial in emphasizing a culture of compassion for colleagues and in helping one another cope with the stressors that exist in anesthesia practice.
Various system-level interventions have been proposed to address the cycle of burnout, including assessing mental health needs, providing consistent childcare opportunities for frontline workers, allowing work hour flexibility, providing adequate personal protective equipment and COVID-19 testing, and offering reassurance that clinicians will not be relocated to other fields or suffer financial cuts.21 Furthermore, to enhance compassion at the organizational level, institutions must continue to adjust expectations of increased productivity, excessive documentation, and administrative burden which are drivers of burnout. These external factors have been identified to increase pressure on health system leaders, managers and practice leaders.22
Numerous programs have been described that focus on enhancing the patient-caregiver relationship, which also remind clinicians why they entered the profession (Table 2). For example, the Schwartz Center Rounds enable health care providers to develop increased insight into social and emotional aspects of patient care, increasing the level of compassion towards patients, and decreasing feelings of stress and isolation.16 Some institutions have spearheaded programs that feature organizational compassion cultivation training that can improve self-reported mindfulness, self-compassion and compassion toward others.17 Though originating in a pre-pandemic environment, programs such as these may be extremely useful now to mitigate the effects of burnout in anesthesia professionals and other frontline health care workers and could be widely promoted by health care institutions in a spirit of promoting organizational compassion.
Table 2: Compassionate Care Resources for Health Care Providers.
| Center for Mindful Self-Compassion https://centerformsc.org/train-msc/ |
| Cleveland Clinic- Communicate with H.E.A.R.T. https://my.clevelandclinic.org/departments/patient-experience/depts/experience-partners/licensed-programs/communicate-with-heart |
| Compassion Resilience Toolkit https://compassionresiliencetoolkit.org/healthcare/ |
| Hillebrand Center for Compassionate Care in Medicine- University of Notre Dame https://compassionatecare.nd.edu/healthcare-professionals/ |
| Massachusetts General Hospital Empathy and Relational Science Program https://www.massgeneral.org/psychiatry/research/empathy-and-relational-science-program |
| T. Denny Sanford Institute for Empathy and Compassion- University of California, San Diego https://empathyandcompassion.ucsd.edu |
| The Schwartz Center For Compassionate Healthcare https://www.theschwartzcenter.org/programs/schwartz-rounds/ |
Conclusion
Stress and burnout can affect all health care providers. It existed long before the pandemic and will likely grow until we are able to recultivate the deep sense of professional satisfaction that comes with caring compassionately for the sick. Stated another way, “The practice of medicine has always been demanding and exhausting, and it always will be. It is the loss of the ability to care and the buffering of stress and exhaustion that come from caring deeply for and improving the quality of life of patients that have led to the current crisis of dissatisfaction and lack of well-being among many physicians.”18
As DW in the clinical vignette experienced, it was during a time of stress that she was able to reflect on the connectedness to her patient and colleagues in her role as an anesthesia professional. We must be steadfast in combating the forces that impede the delivery of compassionate care and contribute to burnout.
Whether they are financial pressures, production pressures or forces challenging the emotional connection formed with our patients, these pressures will always be part of the perioperative care landscape. In response, institutions in partnership with clinicians, can work to improve workplace support and, by extension, the ability for clinicians to provide compassionate care that is healing for patients and rejuvenating for clinicians such as DW. This is foundational to our commitment to deliver the safe, compassionate care that is emblematic of anesthesia professionals.
References
- Tarantur N, Deshur M. Anesthesia professional burnout- a clear and present danger. APSF Newsletter. 2018;33:43–44. https://www.apsf.org/article/anesthesia-professional-burnout-a-clear-and-present-danger/ Accessed August 11, 2021.
- Maslach C, Jackson S, Leiter M. Maslach Burnout Inventory. Maslach Burnout Inventory Manual (Fourth edition), Menlo Park, CA: Mind Garden, Inc. https://www.mindgarden.com/maslach-burnout-inventory-mbi/685-mbi-manual.html. Accessed July 5, 2021.
- Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129–146.
- Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91:422–431.
- Warner MA. Improving perioperative patient safety: a matter of priorities, collaboration and advocacy. APSF Newsletter. 2021;36:3–4. https://www.apsf.org/article/improving-perioperative-patient-safety-a-matter-of-priorities-collaboration-and-advocacy/ Accessed July 5, 2021.
- Del Grosso B, Boyd AS. Burnout and the nurse anesthetist: an integrative review. AANA J. 2019;87:205–213.
- Alfonso A, Cadwell J, Staffa S, et al. Burnout rate and risk factors among anesthesiologists in the United States. Anesthesiology. 2021;134:683–696.
- Farina CA, Horvath C, Lekhnych F, et al. Clinician burnout: how will we come through the fire? Guest editorial. AANA J. Online content August 2020:54–58. https://www.aana.com/docs/default-source/aana-journal-web-documents-1/farina-ge-r.pdf?sfvrsn=8fa2df1_4 Accessed July 5, 2021.
- Kane, L. Death by 1000 cuts 2021: Medscape national physician burnout and suicide report. https://www.medscape.com/slideshow/2021-lifestyle-burnout-6013456 Accessed July 5, 2021.
- Mental Health Screening Survey 2020, Mental Health America. https://mhanational.org/mental-health-healthcare-workers-covid-19. Accessed July 5, 2021.
- Saslow, E. You’re basically right next to the nuclear reactor. The Washington Post, https://www.washingtonpost.com/nation/2020/04/05/youre-basically-right-next-nuclear-reactor/?arc404=true. Accessed July 5, 2021.
- Trzeciak S, Mazzarelli A. Compassionomics: the revolutionary scientific evidence that caring makes a difference. Studer Group Publishing, USA, 2019.
- Wilkinson H, Whittington R, Perry L, et al. Examining the relationship between burnout and empathy in healthcare professionals: a systematic review. Burn Res. 2017;6:18–29.
- Thirioux B, Birault F, Jaafari N. Empathy is a protective factor of burnout in physicians: new neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Front Psychol. 2016;7:763. doi: 10.3389/fpsyg.2016.00763. PMID: 27303328; PMCID: PMC4880744.
- Waldinger R. What makes a good life? Lessons from the longest study on happiness. TEDXBeaconStreet. https://www.ted.com/talks/robert_waldinger_what_makes_a_good_life_lessons_from_the_longest_study_on_happiness. Accessed July 5, 2021.
- Lown BA, Manning CF. The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork and provider support. Acad Med. 2010; 85:1073–1081.
- Scarlet J, Altmeyer N, Knier S, et al. The effects of compassion cultivation training (CCT) on health-care workers. Clinical Psychologist, 2017;21:116–124.
- Schwenk TL. Physician well-being and the regenerative power of caring. JAMA. 2018;319:1543–1544.
- Hawkley LC, Thisted RA, Masi CM, et al. Loneliness predicts increased blood pressure: 5-year cross-lagged analysis in middle-aged and older adults. Psychol Aging. 2010;25:132–141.
- Valtorta NK, Kanaan M, Gilbody S, et al. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102:1009–1016.
- Almeida M, DeCavalcante G. Burnout and the mental health impact of COVID-19 in anesthesiologists: A call to action. J Clin Anesth. 2021;68:110084. doi: 10.1016/j.clinane.2020.110084.
- Hofmeyer A, Taylor R, Kennedy K. Fostering compassion and reducing burnout: How can health system leaders respond in the COVID-19 pandemic and beyond? Nurse Educ Today. 2020;94:104502. doi: 10.1016/j.nedt.2020.104502.


Leave a Reply
You must be logged in to post a comment.