INTRODUCTION
The APSF Newsletter in 2009 discussed the risk of late thrombosis after drug-eluting stent placement as an ongoing patient safety concern.1 It found that in-stent thrombosis, though rare, accounted for a 60% myocardial infarction (MI) rate and a mortality of 45% when it occurred. Early animal studies found that complete endothelialization with bare metal stents (BMS) occurred in 28 days, whereas first-generation drug-eluting stents (DES) uniformly showed incomplete healing at 180 days.2 In 2008, the American College of Chest Physicians (ACCP) recommended delaying elective surgery for 12 months after the placement of a drug-eluting stent,3 placing burdens on patients needing urgent surgery. As such, the APSF Newsletter acknowledged in 2009 the lack of universally accepted protocols for managing patients presenting for noncardiac surgery following recent stent placement. It emphasized the necessity for collaborative decision-making involving the patient, internist, surgeon, anesthesia professional, and cardiologist, stating that this multidisciplinary discussion should consider the type and timing of stent placed, the nature and urgency of the proposed surgery, the management of perioperative antiplatelet therapy, and the choice of facility at which to perform the surgery. If surgery must be performed in patients with recent stent placement, it should ideally take place at a facility with a 24-hour interventional cardiologist available, as emergent percutaneous coronary intervention (PCI) remains the best treatment option for in-stent thrombosis.1
DAPT: Dual Antiplatelet Therapy; ACC: American College of Cardiology; AHA: American Heart Association; ESC: European Society of Cardiology
Technology has since evolved dramatically and the recommended duration of dual antiplatelet therapy (DAPT) has changed substantially. First generation stents consisted of a standard bare metallic stent, and a coated polymer mixed with an antirestenotic drug such as sirolimus or paclitaxel. Newer-generation drug-eluting stents such as biodegradable polymer stents or bioresorbable scaffolds are available, which have been shown to lead to lower rates of stent thrombosis. These newer-generation stents may permit a shorter course of DAPT without compromising patient safety.
Perhaps the most important consideration when deciding on the optimal duration of DAPT is balancing the risk of in-stent thrombosis with the risk of bleeding complications. Studies have shown that prolonged DAPT therapy is associated with an increased risk of bleeding, particularly in elderly patients or those with co-morbidities.4,5 Bleeding complications significantly increase the risk of morbidity and mortality, and high bleeding risk (HBR) is present in approximately 40% of patients presenting for PCI.5 Tools that evaluate bleeding risk with DAPT include the PRECISE-DAPT Score6 and the Academic Research Consortium for High-Risk Bleeding (ARC-HBR) Criteria.4
SUPPORTING EVIDENCE FOR SHORTER DAPT DURATION
High Bleeding Risk (HBR) is defined according to the presence of at least 1 HBR criteria (Table 1).⁷
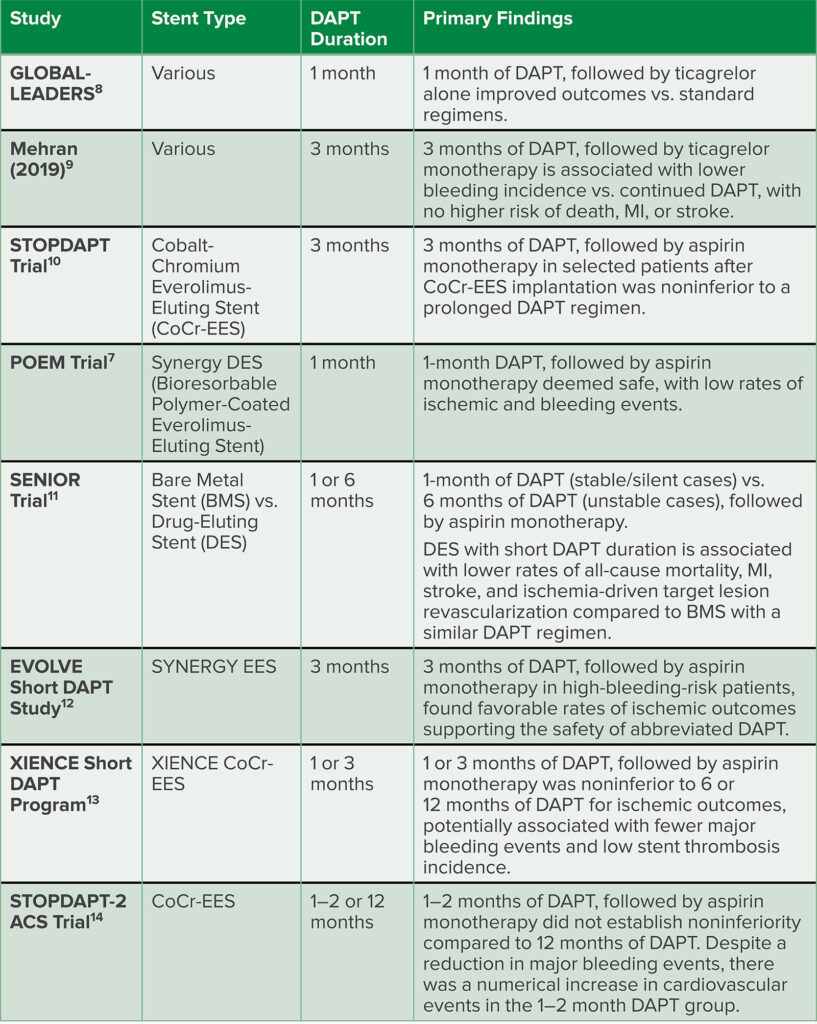
Two early studies examined high-risk patients who underwent PCI and completed a short duration of DAPT with either ticagrelor monotherapy or ticagrelor plus aspirin. Ticagrelor is a reversible and direct-acting oral P2Y12 receptor antagonist that provides faster, greater, and more consistent platelet inhibition than clopidogrel. The first study found that ticagrelor in combination with aspirin for 1 month, followed by ticagrelor alone, improved outcomes after PCI compared to standard antiplatelet regimens.8 The second study examined high-risk patients who underwent PCI and completed 3 months of DAPT, determining that ticagrelor monotherapy was associated with a lower incidence of clinically relevant bleeding than ticagrelor plus aspirin, with no higher risk of death, MI, or stroke.9
Several other pivotal trials have recently been published that highlight the safety and efficacy of the earlier discontinuation of dual antiplatelet therapy (Table 2). These newer stents are ideal for patients who are at higher risk of bleeding. These studies have uniformly found lower rates of ischemia, allowing shorter duration of DAPT, which lessens patients’ bleeding risk. These newer stents also compare favorably to bare metal stents in terms of all-cause mortality, myocardial infarction, stroke, and ischemia-driven target lesion revascularisation.10-14
Table 2: Summary of Recent Studies Examining Abbreviated DAPT Regimens.
SOCIETAL GUIDELINES
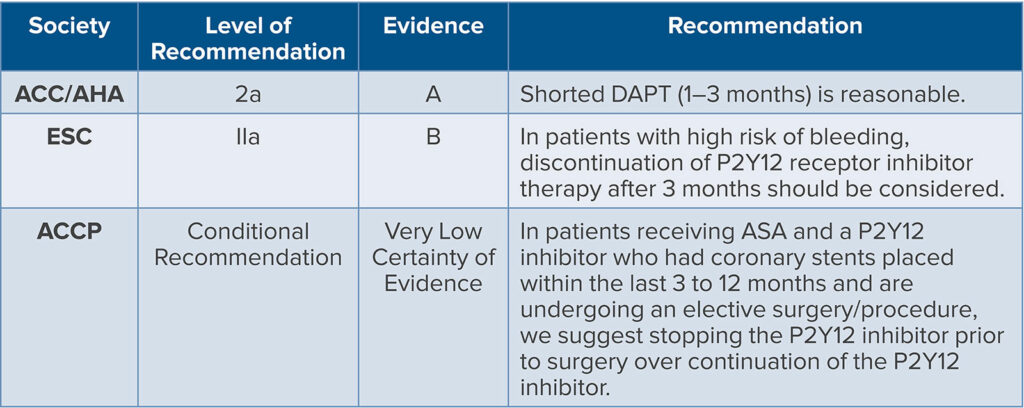
Based on the available and updated evidence, The American College of Cardiology (ACC) and the American Heart Association (AHA) give a Class 2a (moderate) recommendation for a shorter duration of DAPT. Select patients undergoing PCI may safely transition to P2Y12 inhibitor monotherapy and discontinue aspirin after 1–3 months of DAPT, where the benefits outweigh the risks.15
In contrast, the European Society of Cardiology offers the following guidance on DAPT duration.16 Following PCI for non-ST-segment elevation acute coronary syndrome (NSTE-ACS), DAPT with a potent P2Y12 receptor inhibitor and aspirin is generally recommended for 12 months, regardless of stent type, unless contraindicated. However, in specific clinical contexts, such as high bleeding risk (e.g., based on the PRECISE-DAPT scoring of > 25 or meeting ARC-HBR criteria), clinicians may consider shortening DAPT duration (<12 months) or modifying the regimen based on ischemic and bleeding risks, adverse events, comorbidities, concomitant medications, and drug availability. Notably, in NSTE-ACS patients with stent implantation at high bleeding risk, discontinuation of P2Y12 receptor inhibitor therapy after 3–6 months should be considered. In cases of very high bleeding risk, such as a recent (past 30 days) bleeding episode or imminent nondeferrable surgery, a regimen of 1 month of aspirin and clopidogrel may be appropriate.
In 2022, the American College of Chest Physicians (ACCP) updated its recommendations regarding the timing of DAPT after DES placement.17 The ACCP provides a conditional recommendation for patients scheduled for elective surgery who have had stent placement within the last 3 to 12 months and are on DAPT. It recommends the discontinuation of the P2Y12 inhibitor prior to surgery, based on indirect evidence and expert opinion suggesting the safety of stopping P2Y12 inhibitors in patients with stents implanted more than 3 months prior (Table 3).
Table 3: Societal Recommendations for Shortening DAPT Prior to Surgery.
CONCLUSION
Paradigms within the field of cardiology regarding the duration of DAPT have changed dramatically since the 2009 APSF Newsletter. Newer generation stent technology has led to less stent thrombosis, and cardiology experts have in turn reduced their recommended duration of DAPT on these new drug-eluting stents to 1–3 month courses of anticoagulation in patients with stable coronary artery disease. Due to the enhanced performance of these newer stents, BMS have been rendered relatively obsolete and have fallen out of favor, and therefore, not frequently placed. Decisions of duration of DAPT in the setting of urgent surgery should be made by cardiologists, in close cooperation with surgical and anesthesia teams, and may include a very short course of DAPT. Anesthesia professionals must be mindful of these shorter durations of DAPT and be cognizant of the fact that durations of anticoagulation of as little as one month may be recommended for their recently stented patients, based on the evidence of enhanced safety profile of these newer-generation stents.
REFERENCES
- Greenberg SB, Matten EC, Murphy GM, Vender JS. Perioperative coronary stent thrombosis: a continuing safety concern. APSF Newsletter. 2009;24:17. https://www.apsf.org/article/perioperative-coronary-stent-thrombosis-
a-continuing-safety-concern/ Accessed August 8, 2024. - Tsimikas S. Drug-eluting stents and late adverse clinical outcomes: lessons learned, lessons awaited. J Am Coll Cardiol. 2006;47:2112–2115. PMID: 16697332
- Douketis JD, Berger PB, Dunn AS, et al. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:299S–339S. PMID: 18574269
- Ueki Y, Bär S, Losdat S, et al. Validation of the Academic Research Consortium for High Bleeding Risk (ARC-HBR) criteria in patients undergoing percutaneous coronary intervention and comparison with contemporary bleeding risk scores. EuroIntervention. 2020;16:371–379. PMID: 32065586
- Capodanno D, Morice MC, Angiolillo DJ, et al. Trial design principles for patients at high bleeding risk undergoing PCI. JACC Scientific Expert Panel. J Am Coll Cardiol. 2020;76:1468–1483. PMID: 32943165
- PreciseDAPT Web calculator. PREdicting bleeding Complications In patients undergoing Stent implantation and subsEquent Dual Anti Platelet Therapy. http://www.precisedaptscore.com/predapt/ Accessed August 9, 2024.
- Pivato CA, Reimers B, Testa L, et al. One-month dual antiplatelet therapy after bioresorbable polymer everolimus-eluting stents in high bleeding risk patients. J Am Heart Assoc. 2022;11:e023454. PMID: 35114814
- Vranckx P, Valgimigli M, Jüni P, et al. Ticagrelor plus aspirin for 1 month, followed by ticagrelor monotherapy for 23 months vs aspirin plus clopidogrel or ticagrelor for 12 months, followed by aspirin monotherapy for 12 months after implantation of a drug-eluting stent: a multicentre, open-label, randomised superiority trial. Lancet. 2018;15;392:940–949. PMID: 30166073
- Mehran R, Baber U, Sharma SK, et al. Ticagrelor with or without aspirin in high-risk patients after PCI. N Engl J Med. 2019;381:2032–2042. PMID: 31556978
- Natsuaki M, Morimoto T, Yamamoto E, et al. One-year outcome of a prospective trial stopping dual antiplatelet therapy at 3 months after everolimus-eluting cobalt-chromium stent implantation: ShortT and OPtimal duration of Dual AntiPlatelet Therapy after everolimus-eluting cobalt-chromium stent (STOPDAPT) trial. Cardiovasc Interv Ther. 2016;31:196–209. PMID: 26518420
- Varenne O, Cook S, Sideris G, et al. Drug-eluting stents in elderly patients with coronary artery disease (SENIOR): a randomised single-blind trial. Lancet. 2018;39:41–50. PMID: 29102362
- Kirtane AJ, Stoler R, Feldman R, et al. Primary Results of the EVOLVE Short DAPT study evaluation of 3-month dual antiplatelet therapy in high bleeding risk patients treated with a bioabsorbable polymer-coated everolimus-eluting stent. Circ Cardiovasc Interv. 2021;14:e010144. PMID: 33641374
- Mehran R, Cao D, Angiolillo DJ, et al. 3- or 1-month DAPT in patients at high bleeding risk undergoing everolimus-eluting stent implantation. JACC Cardiovasc Interv. 2021;14:1870–1883. PMID: 34503737
- Watanabe H, Morimoto T, Natsuaki M, et al. Comparison of clopidogrel monotherapy after 1 to 2 months of dual antiplatelet therapy with 12 months of dual antiplatelet therapy in patients with acute coronary syndrome The STOPDAPT-2 ACS Randomized Clinical Trial). JAMA Cardiol. 2022;7:407–417. PMID: 35234821
- Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2022;145:e18–e114. PMID: 34882435
- Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289–1367. PMID: 32860058
- Douketis JD, Spyropoulos AC, Murad H, et al. Perioperative management of antithrombotic therapy: An American College of Chest Physicians clinical practice guideline. CHEST. 2022;162:e207–e243. PMID: 35964704


Leave a Reply
You must be logged in to post a comment.