You’re a patient scheduled for elective surgery tomorrow. You’re nervous and you’d like to drink a glass of wine (or two) at dinner the night before the surgery. Is this OK? What’s the relationship between alcohol and anesthesia?
Alcohol use is common in the United States—fourteen percent of the United States adult population suffers from alcohol addiction. Surgery is common in the United States—there were more than 17 million surgeries performed in America in 2014. The intersection of an alcohol-addicted patient and surgery is therefore common. How much alcohol consumption is too much? The thresholds for defining high-risk alcohol consumption are 5 or more drinks in one day (>14 drinks per week on average) for males under 65 years of age, and 4 or more drinks in a day (>7 drinks per week on average) for all females and males 65 or more years of age. (Miller’s Anesthesia, 9th edition, Chapter 31, Preoperative Evaluation) All adults and adolescents should be questioned regarding their history of alcohol use prior to anesthesia.
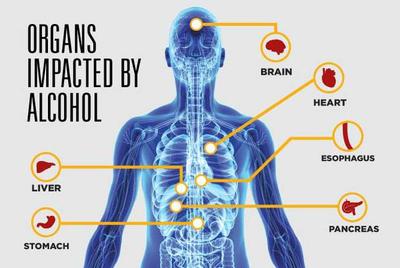
Let’s look at the risks for an acutely alcohol intoxicated patient first. Hospital emergency rooms have no shortage of drunken individuals who’ve been involved in motor vehicle trauma, motorcycle accidents, gang violence, or domestic violence. Acute intoxication with alcohol is usually diagnosed by history or by the smell of a patient’s breath. If an individual requires an acute surgical procedure, their level of intoxication is documented by measuring the alcohol concentration in their blood prior to surgery. Extreme levels of acute alcohol intoxication can cause coma or stupor, because alcohol is a central nervous system depressant, but other causes of decreased mental status must also be considered. An altered mental status in a trauma victim who smells of alcohol may be secondary to the central nervous system depressant effect of alcohol, or it may also be secondary to intracranial trauma. A CT scan of the head is indicated. High levels of alcohol intoxication alter a patient’s tolerance to anesthetic medications, because many anesthetics are central nervous system depressants just like alcohol, and there can be an additive effect between the alcohol and the anesthetic doses. Polydrug abuse is common, and blood tests are done on intoxicated patients to determine if other central nervous system depressants (opioids or sedatives), stimulants (cocaine, amphetamines), or other psychotropic substances (e.g. cannabis REF) are present. During surgery, anesthesiologists titrate medications to the desired effect by adding doses cautiously and following the effects on the patient’s vital signs of blood pressure and heart rate. Following surgery, anesthesiologists are vigilant symptoms of acute alcohol withdrawal syndromes. Chronic heavy alcohol use is associated with a two-fold to five-fold increase in postoperative complications, including higher rates of admission to intensive care units and increased lengths of hospital stay. (Chapman R, Plaat F, et al, Alcohol and Anaesthesia, Continuing Education in Anaesthesia, Critical Care and Pain, Volume 9, number 1, 2009, pp 10-13)
For elective scheduled surgeries, patients are seldom intoxicated, but the issue of their chronic alcohol intake is important. Doctors and nurses question each patient regarding the history of alcohol consumption prior to surgery, and are aware that patients often downplay the quantity of their alcohol consumption. A patient who admits to one or two drinks per day may very well consume twice that amount. Chronic alcohol use can increase the dose requirements for general anesthetics, either because of induction/stimulation of the microsomal ethanol-oxidizing system (cytochrome P-450 system), or through the development of cross tolerance to other central nervous system drugs. (Chapman R, Plaat F, et al, Alcohol and Anaesthesia, Continuing Education in Anaesthesia, Critical Care and Pain, Volume 9, number 1, 2009, pp 10-13)
As a patient, what should you do?
Be honest with yourself and your doctors if you drink daily. Alcohol dependence can and will affect your anesthetic and your body’s reaction to anesthetic drug dosing. Your anesthesiologist will be your consultant, and will administer anesthetic medications and doses in a range that is safe for you. In a perfect world, patients with heavy alcohol dependence should be identified before elective surgical procedures and referred to alcohol counseling services.
Does mild alcohol consumption of one to two glasses of wine or one to two beers per day increase anesthetic risk prior to surgery? Your risks will ultimately depend on the complexity of the surgery and the number of other medical problems that you have, but for most patients it’s unlikely you’ll have any anesthetic or surgical complication based only on this amount of alcohol consumption. One glass of wine with dinner may very well help you relax and get adequate sleep the night before your anesthetic.

