Dr. Whitten is the author of “Anyone Can Intubate: A Step–by–Step Guide to Intubation and Airway Management” and “Pediatric Airway Management: A Step–by–Step Guide,” both from Mooncat Publications. She also blogs about airway management at AirwayJedi.com, and has created instructional DVDs on the topic. She reported no other relevant financial disclosures.
Anesthesiologists who perform fewer than 100 pediatric cases on infants and young children per year are five times more likely to experience complications compared with anesthesiologists who do more than 200 cases per year.
There is good reason why most providers are anxious about taking care of children, especially infants and children less than 2 years of age. It is challenging and intimidating to open the airway of such a small infant when adult-sized fingers dwarf the size of the baby’s mouth and all of the instruments are smaller.
The size, weight, anatomy and physiology of the infant and young child vary greatly from the adult. Failure to modify medical management appropriate to the age of the child can easily lead to complications, such as loss of the airway with failed ventilation, inadequate volume replacement and medication error.
My first introduction to the precariousness of the infant airway occurred during my anesthesia residency. I had just provided a sitting dose for a routine vaginal delivery and was monitoring vital signs. The obstetric resident had just delivered his first baby under the watchful eye of his attending. He was holding the newborn head downward to suction the airway, left hand wrapped securely around the baby’s neck to keep the slippery, wriggling newborn from sliding from his grasp. A minute passed. The baby wasn’t crying and had not taken a breath. I could see the resident’s anxiety rising. His attending leaned over and gently said, “Lift your left thumb.” Thumb raised, the baby took a huge gasp and let out a loud and raucous cry. The resident had been obstructing the baby’s airway simply by pressing on the neck.
Children Are at Increased Risk
The American Society of Anesthesiologists (ASA) closed claims analysis and the Pediatric Perioperative Cardiac Arrest (POCA) registry show that cardiac arrest and brain death in pediatric patients are still mainly caused by airway problems, despite improvements such as monitoring of oxygenation, capnography, and anesthetic medications.1,2 The POCA registry found that respiratory events led to 27% of all pediatric perioperative cardiac arrests. Laryngospasm was the most common cause of respiratory-related arrests. Other etiologies included airway obstruction, difficult intubation, esophageal intubation and aspiration.3 Pediatric respiratory events carry a higher mortality rate than adult events.
Anesthesiologists who perform fewer than 100 pediatric cases on infants and young children per year are five times more likely to experience complications compared with anesthesiologists who do more than 200 cases per year. One in five of those infants who have complications will experience severe complications.4-6 A 1994 review of anesthetics for over 4,000 infants less than 12 months of age found that one of the four main risk factors for bradycardia (in addition to ASA physical status, duration of surgery and emergency vs. elective procedure) was actually whether there was a non-pediatric versus pediatric anesthesiologist.5
These statistics refer to care provided by anesthesiologists, who perform advanced airway management daily. They don’t address care by more occasional managers of the pediatric airway, such as paramedics. For example, less than 1% of paramedic calls are for pediatric patients needing advanced airway management, yielding an average of one pediatric intubation every five years, even in urban areas. An endotracheal tube (ETT) placed in a pediatric patient in the field is more likely to be malpositioned.7,8
Because of these risks, it’s now common practice to concentrate the majority of pediatric care in the hands of providers who are more experienced with children. Pediatric anesthesia is increasingly directed to pediatric anesthesiologists, often in children’s hospitals.9 Many emergency medical services technicians now postpone advanced airway management in the field and instead support the airway with a bag-valve-mask device or laryngeal mask (LM) airway until the child arrives in the emergency department.
However, the trend to only use pediatric providers has a seriously negative unintended consequence: It deprives other providers of routinely caring for children, making them lessprepared for when they do inevitably have to care for a small child.
Don’t Let Fear Stop You From Providing Care to a Child!
Although it’s normal to be intimidated when treating an infant or a small child, most children have easily managed airways. It is essential that your pediatric patient stays oxygenated and ventilated. If you prepare what you need ahead of time, take the differences in anatomy and physiology into account, and are methodical and gentle, you will not hurt the baby. Let’s look at why children are at increased risk.
1. An Immature Nervous System Predisposes to Airway Complications
Infants are children up to 12 months old, and toddlers are between 1 and 2 years old. This article will concentrate on the differences in these youngest age groups. A young patient’s increased parasympathetic tone, immature brain, underdeveloped respiratory center, and behavioral responses increase the risk for airway complications and respiratory failure (Figure 1).
Hypoxia in a Child Causes Bradycardia!
Consider bradycardia in a child to be caused by hypoxia until proven otherwise! Hypoxia in an adult or older child usually triggers a sympathetic response, producing a tachycardia that improves oxygen delivery. Bradycardia is a late and very dangerous sign of imminent cardiovascular collapse.
In contrast, bradycardia in babies and young children may be the first sign of hypoxia—not the last. The small child’s immature nervous system has a better developed parasympathetic nervous system. Babies spend a lot of time eating and sleeping, and not so much time engaged in fight-or-flight activities. As a result, hypoxia triggers a vagal response and slows the heart.
Infants and small children have a cardiac output that is rate dependent. Bradycardia significantly lowers cardiac output and oxygen delivery; hypoxia and hypercarbia worsen. Acidosis develops, further depressing the myocardium. Cardiac arrest can occur very quickly in the hypoxic child and must be treated urgently with oxygen, ventilation, and if needed, atropine.
In one study, among 1,018 children who were difficult to intubate, 9% of patients developed hypoxemia, and cardiac arrest occurred in 16% of these hypoxemic patients.10 All cardiac arrests were preceded by hypoxemia.
Children Are Easily Oversedated
Nerve myelination is incomplete and the blood–brain barrier is poorly developed at birth. Central nervous system immaturity, combined with relative lack of exposure to drugs, can cause respiratory depression and apnea even in older children. Children often become very sleepy, and perhaps apneic, with even small doses of pain medications. It’s difficult to differentiate between a child crying from fear and one crying from pain. It’s very easy to overmedicate with pain medications to try to calm a crying child.
In addition, altered control of ventilation, with periodic breathing and apneas, can be seen up to about 60 weeks post-conceptual age. Young infants, especially if they have a history of prematurity, must be observed carefully when ill or when undergoing anesthesia because of the high risk for apnea. Many institutions will observe ex-premature infants less than 60 gestational weeks overnight following general anesthesia.11,12
Children Are Uncooperative
Babies and frightened younger children are rarely cooperative. Even simple tasks such as preoxygenation may prove impossible. Immature behavior increases the risk for hypoxia in children in the following ways13:
- Stress and physical struggling greatly increase metabolic rate and oxygen consumption at a time when the child may not be able to improve oxygen delivery.
- Crying increases secretions, airway irritability and airway edema.
- Physical struggling increases the work of breathing.
- An active upper respiratory infection or active wheezing also increases the work of breathing.
Make Care as Unthreatening as Possible
If you separate a toddler from his parent, force an oxygen mask on the child’s face, increase the sevoflurane to high, and then try to do a mask inhalational induction, the child will typically fight you as though their life depended on it. If the child has aspirated a peanut or has croup, panic and crying will only jeopardize the airway and worsen hypoxemia.
We routinely perform mask inhalational inductions on children, often with a parent present, to avoid stressing the child. We then place the IV access after the child is asleep. Inducing general anesthesia without IV access does increase risk that must be weighed against any benefit of proceeding without starting the IV first. Always be prepared for emergency airway management in case of complications, such as laryngospasm, by having the supplies for intramuscular injection immediately available.
Premedication, such as oral midazolam, can improve cooperation and perhaps provide amnesia, but has been associated with a longer postoperative stay and a higher incidence of emergence delirium. Sedation should be used with extreme caution if the child has a compromised airway or respiratory failure.
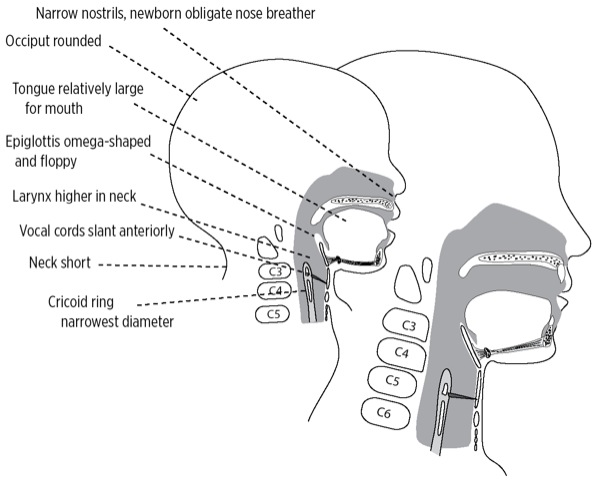
2. The Pediatric Upper Airway Is Prone to Obstruction
Children are not small adults. Pediatric anatomy differs in four main ways: size, composition, position and shape. We can often tell how old a child is simply by looking at head size, facial characteristics, neck length and body shape. It should not be surprising that the inside of the child is changing as well. Infants, who have the greatest anatomic differences, have the highest risk for airway complications (Figure 2 and Table 1).
| Table 1. Differences in the Infant and Toddler Airway Predispose To Airway Obstruction | |
| ANATOMY | RISKS |
|---|---|
| Narrow nostrils, newborn is obligate nose breather | Nasal obstruction in a newborn causes airway obstruction and respiratory distress. Choanal atresia can cause cyanosis when baby feeds, which resolves when baby cries. |
| Occiput is large and round, compared with flatter adult skull | When supine, occiput flexes head forward, potentially obstructing airway. |
| Tongue large relative to mouth, filling the oropharynx | Tongue easily obstructs larynx if baby loses consciousness. |
| Laryngeal and tracheal cartilage soft and easily compressed | Excessive flexion or extension of the head, as well as external pressure on the larynx can obstruct the airway. |
| Larynx higher in the neck: near C2, C3 vs adult location at C4, C5 | With the larynx higher, the tongue and soft tissue can easily obstruct the larynx. |
| Cricoid ring is narrower than glottic opening, reverse of adult | Narrow cricoid creates a funnel-shaped larynx, and places young child at risk for obstruction from subglottic edema such as croup. |
| Laryngeal and tracheal diameter is very narrow | Minimal edema can cause significant obstruction. |
| Neck is short | Infant’s chin rests on the chest, reaching the second rib. Hyoid overlaps thyroid cartilage. Identification of laryngeal landmarks for emergency percutaneous airway placement can be difficult. |
| Trachea is short | Accidental extubation and mainstem intubation occur easily with head position changes. |
| Adenoids and tonsils fill posterior pharynx | Hypertrophic tonsils and adenoids can cause obstructive sleep apnea and make manual ventilation difficult. |
| Baby teeth become loose | Accidental aspiration of loose teeth during airway management can occur. |
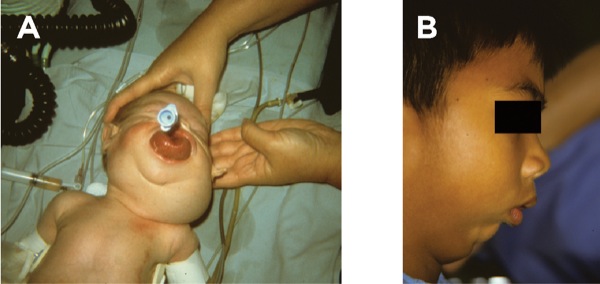
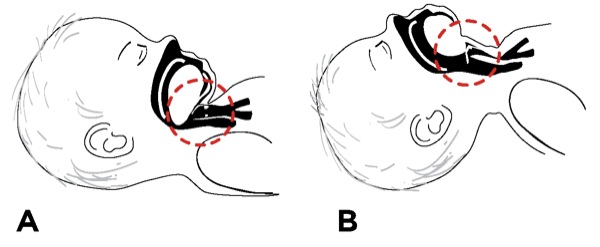
The infant’s large head relative to body size, rounded occiput, large tongue, and larynx positioned higher in the neck all predispose to obstruction if the head flexes forward or the child loses consciousness. The laryngeal and tracheal cartilages are soft and easily compressed (Figure 3A and B).
Infants have suffocated while being held in an extreme flexed position during lumbar puncture.14Studies of infant positioning for lumbar puncture show that oxygen saturation drops significantly more (28% reduction) when an infant is held in a lateral recumbent position with the head flexed forward onto the chest, rather than lateral with the head extended (18% fall) or in a sitting flexed position (15% decrease).15
The larynx itself has a different shape (Figure 4). Unlike in the adult, the airway in infants and children is wider at the top, above the glottis, and narrows below the larynx in the subglottic area (Figure 5). This funnel shape predisposes the child to a greater risk for airway obstruction from processes causing subglottic edema, such as croup or intubation trauma.
The larynx and trachea are so small that minimal swelling can cause tracheal obstruction. In an adult, 1-mm circumferential swelling with a 10-mm trachea causes a 44% decrease in cross-sectional area and triples the resistance to airflow. If an infant with a 4-mm trachea develops 1-mm circumferential edema, there is a 75% decrease in area, with an associated 16 times increase in resistance (Figure 6). Infections such as croup, or a coin stuck in the esophagus but compressing the soft trachea, can place serious limits on the infant or toddler’s ability to breathe.
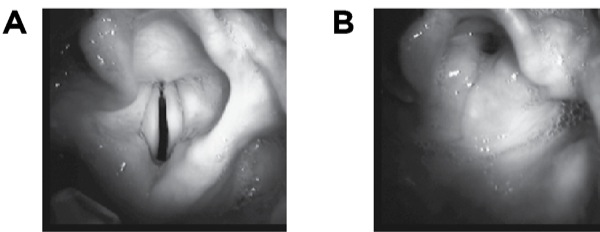
As a child gets older, tonsils and adenoids often fill the airway, causing obstructive sleep apnea and difficulty with manual ventilation. Figure 7 shows hypertrophied tonsils almost meeting in the midline—the so-called kissing tonsils. If you look closely, you can see that the epiglottis and vocal cords are high enough in the neck to be seen behind the back of the tongue.
Take Anatomy Into Account When Opening the Pediatric Airway
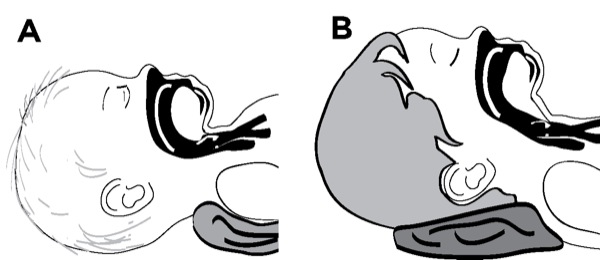
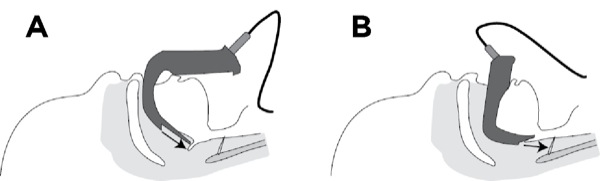
Extreme extension or flexion of the child’s neck can obstruct the airway. A child younger than 2 years, especially an infant, has a relatively large occiput and a short neck. The larynx is higher in the neck right behind the tongue. A pillow placed under the head of the infant or toddler will bend the head forward over the chest, force the tongue backward, and worsen airway obstruction. It will also make it harder for you to tilt the head back to open the airway. Instead, you should place a small rolled towel under the shoulders in children younger than 2 years to open the airway (Figure 8A).
As the child reaches 2 years of age, the occiput gradually becomes less prominent but is still rounded. Keeping the head in a more neutral position is helpful at this age. At some point in the older child, placing a roll under the child’s head, as you would with an adult, improves the airway (Figure 8B).
Oral Airways Must Be the Correct Size
The correct-sized oral airway places the flange immediately outside the teeth or gums and positions the tip near the vallecula. An airway that is too small places the tip in the middle of the tongue, bunching the tissue and worsening obstruction. It can obstruct the lingual vein and cause tongue swelling. Too large an airway extends from the mouth and prevents sealing the mask over the face. It can fold the epiglottis down over the glottic opening and worsen obstruction (Figure 9A and B).
To estimate the correct size, place the airway next to the child’s jaw parallel to the mouth and judge where it will lie. The tip should extend from the center of the patient’s mouth to the angle of the lower jaw (Figure 10).
Beware loose baby teeth! If one comes out during airway management, make sure you know where it is. If you can’t find it, take an x-ray.
Be Careful Using Nasal Airways With Hypertrophied Adenoids
Nasal airways can cause nosebleeds, especially in 3- to 6-year-old children with hypertrophied adenoids. They can become plugged adenoidal tissue, which can then be aspirated. Be very gentle when using one and lubricate it well.
The correct-sized nasal airway should reach from the patient’s nostril to either the earlobe or the angle of the jaw (Figure 11). It is usually 2 to 4 cm longer than the correct oral airway. Selecting the size of a nasal airway based either on nostril opening or comparing it with the size of the little finger is not accurate because the cartilaginous turbinates narrow the inside of the nasal passages. Once inserted, a nasal airway should not be so large that it blanches the skin around the nostrils—a sign of ischemic compression.
If you don’t have a nasal airway small enough for the child, you can cut an ETT to the appropriate length. Cut the adapter end and position the beveled tip in the posterior pharynx above the glottis, but not down the trachea. Reinsert the adapter, once cut, to prevent loss of the tube into the oropharynx. An ETT is stiffer than a typical nasal airway, so insert it gently.
You can manually assist ventilation through the nasal airway by closing the mouth and attaching an ETT adapter to a ventilation device (Figure 12).16
3. Babies and Small Children Get Hypoxic Very Easily
Infants and young children have little respiratory reserve and can develop respiratory failure and hypoxemia quickly when they are ill.
An Infant Can’t Hold His Breath As Long as an Adult
The infant metabolic rate is roughly double the adult rate. Full-term infants are born with 20 million to 50 million alveoli, about 10% of the 200 million to 500 million found in the adult—giving them about 26 times less area for gas exchange.17 Surface area varies from 2.8 m2 in the infant (about the size of a baby blanket) to 75 m2 in the adult (about half a tennis court).
Regardless of age, a normal resting tidal volume (TV) is about 8 mL/kg of lean body weight. A 2.7-kg infant’s TV is only about 22 mL.
Functional residual capacity (FRC), the amount of air left in the lung after a normal exhalation, effectively acts as the lung’s oxygen tank. The larger the FRC, the bigger the oxygen tank and the more respiratory reserve. FRC in an adult is about 70 mL/kg and is about 18 mL/kg in the infant.18,19 With a 75% smaller oxygen tank, the infant can’t hold his breath as long as an adult.
Dead space is also higher in the infant (3 compared with 2 mL/kg in the adult). A larger dead space means less of the TV is available to ventilate alveoli and more of each breath is wasted.
Putting all these values together, Figure 13 demonstrates the profound differences in the lung volumes that affect ventilation of a 2.7-kg infant compared with a 60-kg adolescent. The infant or toddler must have a higher respiratory rate and heart rate to compensate for smaller TVs, larger dead space, higher oxygen consumption, and higher carbon dioxide production. Slow respiratory or heart rate can rapidly lead to cardiorespiratory failure. The smaller TVs of an infant and a toddler also increase the risk for barotrauma when they are exposed to large TVs or high inflation pressures.
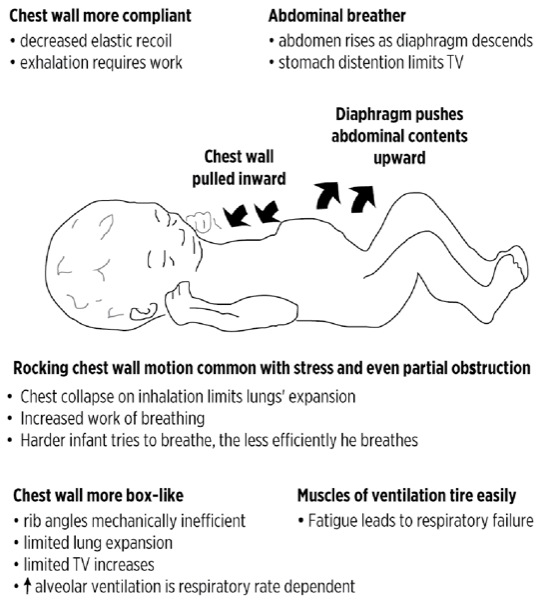
An Infant’s Chest Wall Increases Work of Breathing
The pediatric chest wall is mechanically less efficient and limits potential lung expansion. Babies “belly breathe.” To take a deep breath, the infant’s chest can only expand a little because of the more horizontal angles of the rib cage. The abdomen therefore expands a lot as the diaphragm descends, pushing abdominal contents down and out of the way. Anything that interferes with descent of the diaphragm, such as a stomach or intestines distended with air or liquid, can seriously impair an infant’s breathing.
The infant’s chest wall is also more compliant than an adult’s, with an elastic recoil close to zero because of the lack of rib cage ossification. When the infant takes a breath against resistance, such as with airway obstruction or poor pulmonary compliance from pneumonia, the chest wall actually moves inward as the belly moves outward. The inward movement of the chest wall decreases the amount of air that enters. A rocking chest wall motion is very common in children who have even partial airway obstruction.
Because chest wall structure and belly breathing limit the ability to increase TV, the infant must rely on increases in respiratory rate to compensate for respiratory distress. The harder a child tries to breathe, the less efficient and more labored breathing becomes (Figure 14).20
Ensure Good Ventilation to Avoid Hypoxia
If your patient is not breathing well after opening the airway, then you must assist by using a technique appropriate for the age of the child.
Preoxygenate All Patients If Possible
Optimize oxygenation. If the child won’t tolerate the mask, use blow-by oxygen. If you’re not sure of the airway, use 100% oxygen for induction. If I choose to use nitrous oxide to assist an induction, I never use more than 50% and then will turn off the nitrous oxide once the child falls asleep in order to maximize preoxygenation.
Minimize Apneic Periods
During elective anesthesia, and in the absence of preoxygenation, hypoxemia can occur rapidly—even in the brief period between stopping mask ventilation and insertion of an LM airway or ETT. If you must interrupt ventilation, use apneic oxygenation by holding the airway open while administering oxygen by face mask.
Obtain a Good Mask Fit
To ventilate a child, first choose the correct mask size. The proper size covers the space between the bridge of the nose and the crease of the chin. Too large or too small a mask will prevent a good seal.
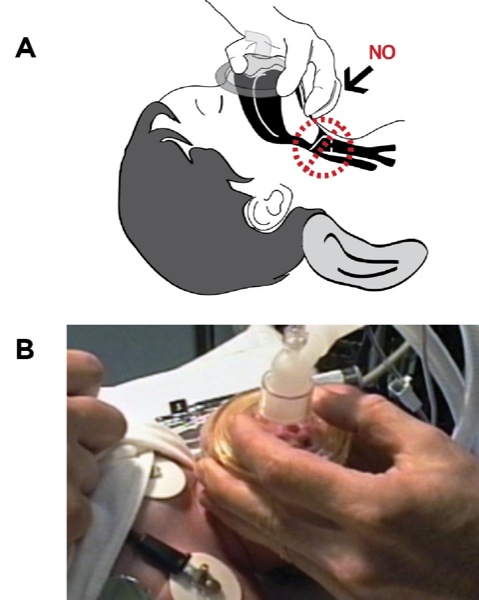
The face of an infant or a toddler is a lot smaller relative to your hand. You will still use your thumb and forefinger to press the mask against the face. Unlike in the adult, however, the size of your hand may not allow you to put all your fingers on the mandible. It’s not uncommon in a small infant to use just your third finger on the jaw to pull the face into the mask, with the fourth and fifth fingers free. Don’t press on the soft tissue under the chin with the remaining finger(s). Pressure there can increase airway obstruction by pushing the tongue and epiglottis back over the laryngeal outlet, and by compressing the soft laryngeal cartilages (Figure 15A and B).
Protect the eyes since small face size, large eyes and a minimal bridge of the nose place the child’s eyes in harm’s way from the mask. Consider taping them closed before applying the mask if the patient is unconscious.
Avoid Barotrauma: Ventilate With Appropriately Sized Breaths
It is essential that you know the appropriate size of your child’s TV. An infant weighing 3 kg has a 24-mL TV (8 mL/kg × 3 kg), which is less than 2 tablespoonfuls (30 mL). A 70-kg adult has a 560–mL TV. Because the walls of a child’s lungs are thinner and less mature, they are more fragile and more easily damaged. Giving an adult-sized TV to a small child can overpressurize the lungs and cause pneumothorax.
If you can, choose a ventilation bag appropriate for the size of the child. It is easier, and safer, to deliver a 30-mL TV when using a 250-mL infant bag than a 1-L adult bag.
Always watch the chest expand while ventilating to estimate the size of the TV you are delivering. Ensure the airway is open to avoid stomach distention, which can seriously impair your ability to ventilate a baby. If the diaphragm can’t descend, then air can’t easily enter the lungs. If stomach distention occurs, then pass a soft suction or oral gastric tube to decompress. You will often see marked improvement in ventilation.
Carefully Preset Your Anesthesia Machine
Case: One of my colleagues, a skilled anesthesiologist who infrequently anesthetizes small children, had just done a mask induction on an 18-month-old boy weighing 11 kg for hypospadias repair. I was assisting as an extra pair of hands by starting the IV line. After he intubated the patient, he pressed the start button on the ventilator. I looked over at the ventilator as he did so and saw the ventilator was set to volume mode and the tidal volume was still at the 500-mL default setting for an adult. Unable to reach the ventilator itself, I quickly disconnected the breathing circuit from the ETT and pointed out the problem. The baby never got the first breath. We were lucky.
Anesthesia providers often rely on the safety features of modern anesthesia machines, such as the high-pressure alarms, to help protect patients. However, you must take extra precautions when using your anesthesia machine on a child because there is little margin for error. What could be an inconsequential mistake in an adult can be a catastrophic error in a baby.
Use Pressure Mode Instead of Volume Mode
Even though you can use either pressure control mode or volume control mode to ventilate a child, it is more common to use pressure control. Historically, older anesthesia machines lacked the precision to deliver the small TVs needed to ventilate a small baby. In addition, the provider would not know whether the TV chosen would deliver too high an inspiratory pressure until after the first breath or two had already been delivered.
By using pressure control mode, the provider can deliver very small TVs with a preset maximum pressure, thereby avoiding potential overpressurization of the circuit and barotrauma. By starting with a lower than anticipated set pressure, you simply watch how the chest expands as you slowly, and safely, increase inspiratory pressure until the optimal TV is achieved. If you don’t see the chest expand, the TV is too small. I always watch my patient’s chest when setting the ventilator to verify that my patient is ventilating optimally.
Always Preset the Maximum Pressure And Tidal Volume
Starting an anesthesia machine ventilator for an adult patient is sometimes done in a very spontaneous manner. By this I mean the ventilator is often started using the default 500-mL TV setting. The provider then modifies the TV setting after the first few breaths for that particular patient. If you are caring for an average-sized adult, you will rarely cause harm with this technique. However, if you deliver a 500–mL breath to your 5-kg baby (40-mL TV) or 15-kg toddler (120-mL TV), you could very well cause a pneumothorax with the first breath.
Use your machine’s neonatal or pediatric settings. Always preset your ventilator settings for the size of the child you’re going to ventilate. Do so even if you plan spontaneous ventilation, because your anesthetic plan could change quickly.
Even when I am going to use the pressure control mode, I always preset my volume control parameters, too. In an emergency, or any moment of distraction, it’s too easy for you—or anyone who comes to help you—to accidentally turn on the volume mode instead of the pressure mode. If you’ve left the machine with any default adult settings, accidentally turning on the wrong mode could be dangerous.
Watch Your Pop-Off Valve to Avoid Barotrauma
To avoid traumatizing a child during elective surgery, anesthesia providers often perform a mask inhalational induction. It’s very common during mask inductions to use high volume flow, even a 10-L per minute flow, to rapidly change the agent concentration.
Once a patient is intubated, the ETT is immediately attached to the breathing circuit. Failure to fully open the pop-off, or to decrease the flow, can distend the ventilation bag and lead to potential barotrauma. The rather humorous picture in Figure 16 is an anesthesia machine inadvertently left in test mode for several minutes, with the pop-off valve set to 20 mm Hg and 10-L flow. Technically 20 mm Hg is not that high a pressure, but I think we can all agree that the ventilation bag is distended to the extent that if this were a pair of lungs, there might be serious trauma.
4. Always Have the Right-Sized Equipment Before You Start!
Be sure you have the appropriately sized equipment, especially ventilation equipment, immediately available for the child you are treating. If the mask you have is too large for the face, ventilation may be impossible. An incorrectly sized oral airway can make obstruction worse. If the ETT is too large, you won’t be able to insert it at all (Table 2).
| Table 2. Suggested Sizes of Pediatric ETTs | ||||
| Age | Size (mm ID) | Oral Depth (cm) | Miller | Macintosh |
|---|---|---|---|---|
| (age in years/4) +4 | (age in years/2) +12 | |||
| Premature | 2.5-3 | 6-8 | 0 | 0 |
| Newborn | 3-3.5 | 9-10 | 0 | 0 |
| 3-12 months | 4 | 10.5-12 | 0 | 0 |
| 1 year | 4 | 12.5-13.5 | 1 | 1 |
| 2 years | 4.5 | 13.5 | 2 | 2 |
| 4 years | 5 | 14 | 2 | 2 |
| 6 years | 5.5 | 15 | 2 | 2 |
| 8 years | 6 cuffed | 16 | 2 | 2 |
| 10 years | 6.5 cuffed | 17 | 2-3 | 2-3 |
| 12 years | 6.5-7 cuffed | 18 | 2-3 | 3 |
| Adolescent | 6.5-7+ cuffed | 21 | 2, 3, 4 | 3 |
| Adult | 6.5-8 cuffed | 21 | 2, 3, 4 | 3-4 |
| American Heart Association formulas: uncuffed ETT: (age in years) + 4; cuffed ETT: (age in years) + 3; depth at lip: ETT size X 3
Note: all patients are different and formulas are guidelines only—always check position clinically
ETT, endotracheal tube; ID, internal diameter
|
||||
In addition to the predicted size ETT, have one size larger and one smaller immediately available. Have a stylet and suction catheter that will fit the smallest tube you might use. You don’t want your helpers leaving you in an emergency to fetch things if the size you chose won’t fit. Please do not open all of this backup equipment until you need it.
A pediatric laryngoscope handle is thinner and lighter, and the blades are shorter. This makes it easier to manipulate the smaller anatomy, but can make it harder for a large adult hand to hold and control. Pediatric intubating equipment should include Miller or straight blades in size 0 for infants, size 1 for age 1 to 2 years, and size 2 for older children. You may want to have a Macintosh (Mac) 2 blade available as well.
Although you can intubate an infant or a toddler with a larger blade, it’s technically more difficult. The larger blade can interfere with both visualization and passing the tube. It also carries greater risk for injuring the oropharynx.
Anesthesia departments often have dedicated pediatric carts. In addition, emergency rooms and other treatment areas will frequently have Broselow pediatric emergency tape (Armstrong Medical). A Broselow tape is a color-coded measuring tape that correlates the length of the child with the average weight of such a child. This then guides the provider to the correct-sized equipment, dosages of emergency medications, and shock voltage on a defibrillator. An associated Broselow Cart has a color-coded drawer dedicated to each length of child on the tape, ensuring the correctly sized equipment is readily available.
5. The Infant and Toddler Have a More Anterior Airway for Intubation
We describe an airway as being anterior when the view of the larynx during laryngoscopy is hidden behind the back of the tongue. The anatomy of babies and toddlers often produces a slightly more anterior airway as follows:
- The pediatric larynx is located higher in the neck than in an adult, making it harder to lift the epiglottis by pressing on the hyoepiglottic ligament.
- The tongue is larger relative to the size of the mouth.
- Babies in particular have short necks.
- There is a smaller separation between the hyoid and thyroid cartilage.
Modify Your Intubation Technique For Infants and Toddlers
Which Type of Blade for Children?
A higher larynx and larger tongue make displacing the tongue and associated tissues forward, and off the larynx, more difficult. Straight blades, which lift the epiglottis, often allow a clearer view of the cords.
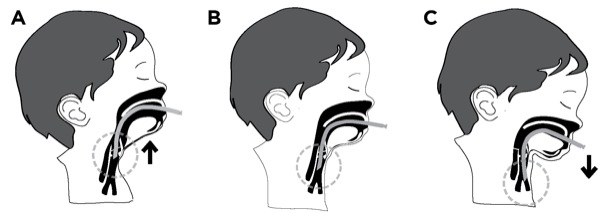
In contrast, in a baby or toddler, the curved Mac will often fold the child’s epiglottis down over the larynx, blocking your view of the cords (Figure 17). Because the larynx is higher in the neck, pressing on the hypoepiglottic ligament in the vallecula may pull the epiglottis into a closed position. If you do use a curved blade, you can, if needed, use it like a straight blade to pick up the epiglottis. Practice with both blade types to build confidence.
Choose the Correctly Sized Endotracheal Tube
An ETT that just barely fits can cause trauma to the mucosa with edema formation and the risk for postextubation croup. If it’s too large, it won’t pass at all. Too small an uncuffed tube won’t provide a seal and can prevent positive pressure ventilation. Sizes and depths of ETT insertion for children of various ages are shown in Table 2.
Cuffed Versus Uncuffed Endotracheal Tube?
Historically, we have used uncuffed ETTs in infants and children younger than about 8 years because the smallest diameter of the younger child’s airway is the cricoid ring. A properly sized round ETT sealed this round opening. Uncuffed tubes avoided cuff pressure on the trachea, which was felt to place the youngest children at risk for subglottic injury and postextubation croup.
The optimally sized uncuffed ETT lets you ventilate while allowing a leak at about 20 to 25 cm H2O. This pressure leak value minimizes the risk for ischemia from compression of the tracheal mucosa. A leak at a lower pressure makes controlled ventilation difficult and increases the risk for aspiration.
Children older than 8 years need a cuff to seal the trachea, because by this age the triangular vocal cord opening has become the smallest diameter.
However, postextubation croup can still occur with uncuffed tubes. Newer research has found that the cricoid ring is more elliptical in shape than round.21 A round, uncuffed ETT placed into an elliptical hole can, despite the presence of a leak, put excessive pressure on parts of the tracheal mucosa. This discovery makes use of uncuffed ETTs less compelling. In addition, pediatric cuffs are now mostly the low-pressure type. It’s therefore becoming much more common to use cuffed, low-pressure tubes in young children because cuffed tubes have advantages:
- They protect better against aspiration.
- They avoid tube changes (and additional trauma) if the initial tube selected is too small.
- The cuffed tubes allow higher ventilation pressures with poor pulmonary compliance.
- They allow more precise monitoring of ventilation.
- They provide a more accurate TV.
- The tubes release less OR pollution from leaking anesthesia waste gas.
- They decrease risk for fire in the OR when an ignition source is present.
Disadvantages of the cuffed tubes include:
- The cuffs take up space and force use of a tube size one-half to one size smaller.
- Smaller tubes have greater resistance to breathing.
- A size 4 ETT has a 59% higher resistance and work of breathing compared with size 5.
- There is a higher risk for plugging the smaller lumen with secretions.
- Suctioning smaller tubes is more challenging.
Choose a cuffed versus uncuffed ETT based on the status of the child and the reason for intubation. Cuffed tubes should be considered for critically ill children, or children undergoing certain surgical procedures where sealing the airway and allowing higher ventilation pressures may be needed.
Raising the Shoulders Can Help Position a Baby for Intubation
Regardless of age, the ear canal should be roughly level with the sternal notch. The infant’s rounded occiput and large head often raise it too high off the intubating surface to obtain the “sniffing position.” Placing a small folded towel or object of similar thickness under an infant’s shoulders raises the rest of the body and straightens the airway path (Figure 18A). As the child grows and the anatomy becomes more adult-like, a small towel under the head becomes helpful.
The infant’s pronounced occiput can also flex the head of the unconscious baby forward when the child lies flat on the bed. The infant occiput also tends to roll, making the act of balancing the baby’s head on your blade a challenge. There are several ways to deal with this tendency:
- Place a rolled towel on either side of the head (Figure 18B).
- Have an assistant steady the head for you (Figure 18C).
- Hold the head steady with your right hand while placing the blade with your left (Figure 18C).
- Use a small, flat gel “donut” designed for this task.
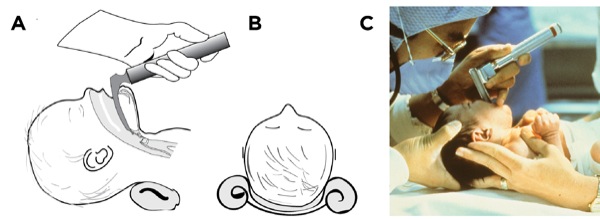
With practice, balancing the head becomes second nature.
Don’t Block the Mouth as You Open It
The infant’s mouth is very small compared with the size of your hand. Failure to place your fingers far to the right can block your view and prevent blade insertion.
Control of the Tongue Is Key to Seeing the Larynx
The infant tongue is much larger relative to the mouth and jaw than in the adult. Failure to sweep the tongue to the left with your laryngoscope blade will leave no room for visualization for tube passage. The laryngeal anatomy appears quite different in infants and toddlers compared with adults (Figure 4).
Careful! It’s Easy to Insert the Blade Too Deeply
Meticulous placement of the tip of the blade is necessary. Picking up the epiglottis with the blade tip in an infant or child less than 2 years old can be hard due to its short, stiff, U-shaped form. It’s very easy to insert the blade too deeply and into the esophagus of such a tiny patient. If you can’t identify anatomy, then pull the blade back slowly while you watch. Often the larynx will drop into view.
Passing the Tube May Be Challenging
The pediatric arytenoids and vocal cords incline anteriorly, an angle that can cause the ETT to catch on the anterior commissure during insertion. Rotating the tube to the right or left allows the tip to slip off the anterior commissure and pass.
Remember, the cricoid ring is smaller than the opening between the vocal cords. You can sometimes insert an ETT through the cords but not beyond the cricoid cartilage. Forcing an ETT can cause traumatic swelling. If the ETT won’t pass, use a smaller one.
Deciding Initial Depth of ETT Insertion
The most familiar formula for calculating ETT depth applies to children older than 2 years. Note: Depth at the lip (ATL) calculations are in centimeters (Table 2).
- Depth ATL = (age in years/2) + 12
For infants and children younger than 2 years of age, calculate ETT depth by using the formula:
- Depth ATL = Calculated uncuffed ETT interior diameter × 3
Formulas for ETT depth of insertion have been clinically validated for neonatal patients weighing more than 750 g up to 4 kg.19,22
- Depth ATL = weight (kg) + 6
Although these formulas are reasonably accurate, you still must verify bilateral breath sounds as children of the same age can vary much.
Esophageal Intubation and Mainstem Intubation Occur Easily
You must constantly be alert to potential misplacement of an ETT. Verify optimal placement every time you reposition the child.
The difference between intubation and extubation in a neonate can be 1 cm. Extension of the neck causes the ETT to rise within the trachea. Inadvertent extubation can occur if the tube is too high. Flexion of the head causes the tip to descend, possibly causing mainstem intubation (Figure 19). “The hose follows the nose” is a useful memory aid.
Cricoid Pressure Must Be Light
Sometimes you need cricoid pressure when intubating a child. However, pressure must be light to avoid distorting or compressing the airway. Placing cricoid pressure in an infant often requires just one finger. For toddlers and older children, use one or two fingers, as appropriate (Figure 20).
Don’t Forget to Ventilate
It is easy to lose track of time during an intubation when the baby is apneic. Infants and young children can’t hold their breaths as long as an adult before the onset of hypoxia. Stop and ventilate if the intubation attempt is taking longer than 30 seconds to one minute. Being proactive about ventilation will help avoid oxygen desaturation, with its risk for cardiac arrest.
6. Successful Laryngeal Mask Airway Use Depends on the Right Size
Not every child needs intubation. Supraglottic airways, such as LM airways, are less stimulating, less traumatic, and are often easier than intubation for the occasional pediatric provider to place. You can also use an LM airway as an interim airway when starting an IV line without an extra pair of hands during inhalational induction. They can be useful as intubation aids, and as rescue devices during difficult intubation.
LM airways are available in sizes for babies as small as 2 kg. But the weight-based size chart can be difficult to remember (Table 3). Choose a pediatric LM airway by comparing the size of the cushion to the child’s external ear. This technique has a 93% success rate, comparable to that of size charts.23
| Table 3. Laryngeal Mask Airway Sizes and Cuff Volumes | |||
| Note that the cuff volumes given are maximum volumes, not the recommended ones. Each cuff should be inflated to minimum seal, which will be a lower volume and will vary with each patient. | |||
| Size | Body weight | Max. Volume (mL) | ETT ID That Can Pass |
|---|---|---|---|
| 1 | Neonates and infants <5 kg | up to 4 | 3.5 |
| 1.5 | Infants 5-10 kg | up to 7 | 4.0 |
| 2 | Infants and children up to 20 kg | up to 10 | 4.5 |
| 2.5 | Children 20-30 kg | up to 14 | 5.0 |
| 3 | Children and small adults >30 kg | up to 20 | 6.0 |
| 4 | Average adolescents/adults | up to 30 | 6.0 |
| 5 | Large adolescents/adults >80 kg | up to 40 | 7.0 |
| ETT, endotracheal tube; ID, internal diameter | |||
Occasionally an LM airway won’t seat easily, especially if there are large tonsils in the posterior pharynx. Consider inserting a partially inflated LM airway laterally against the side of the tongue, advancing until resistance is met and then rotating back into midline. This technique is associated with the highest success rate of insertion and lowest incidence of complications. It could be the technique of first choice for LM airway insertion in children.24,25
An LM airway may slip out of position more easily in a baby less than one year of age. Since these babies desaturate quickly, I prefer to intubate babies less than one year old if the airway is not going to be immediately within my control, or if the procedure is going to last longer than one hour.
Choose your patient carefully. Laryngospasm or aspiration can still occur with LM airways. You won’t be able to deliver higher-pressure breaths if compliance is poor. Always be prepared for more advanced airway management.
7. Always Be Prepared for Laryngospasm
When laryngospasm occurs, vocal cord closure can be so forceful that it can prevent all ventilation or even the passage of the ETT. Life-threatening hypoxia can quickly follow. Other potential complications include post-obstructive pulmonary edema, and possibly even cardiac arrest.
The incidence of laryngospasm during anesthesia is higher in children than in adults, and ranges from 1.7% to 25%.26 Of cardiac arrests found in the POCA registry, 27% resulted from respiratory events. Laryngospasm was the most common cause of respiratory-related events, followed by airway obstruction, difficult intubation, esophageal intubation and aspiration.3
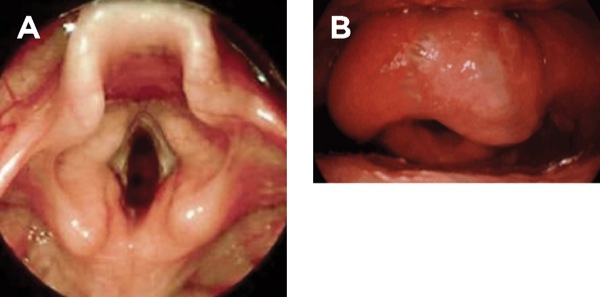
The larynx of an adolescent patient is shown in Figure 21, both before and during laryngospasm.27 You can see closure of the larynx occurs by four mechanisms:
- closure of the vocal cords, both by pulling them together and by tensing;
- closure of the false vocal cords;
- mounding of the paraglottic tissues (lower epiglottis, paraglottic fat, base of tongue) by elevation of the larynx; and
- folding of the epiglottis over the glottic opening.
Avoid Laryngospasm
Laryngospasm is most likely to occur when secretions, mucus, blood or instruments such as a laryngoscope stimulate the vocal cords in a patient who is lightly anesthetized or in stage II. Prime times are during intubation or immediately following extubation. However, laryngospasm can occur with the best of care, especially in patients with irritable airways such as those with asthma, those with upper or lower respiratory infection, and in the presence of airway anomalies.28
There are measures to manage laryngospasm:
- Consider postponement of elective surgery if the child has a significant upper respiratory infection or active wheezing.
- Never stimulate the airway in stage II anesthesia.
- Don’t extubate if the child is actively coughing. Time removal for quiet breathing when the cords will be open.
- Keep the airway clear of secretions.
- Consider a muscle relaxant during intubation of a high-risk child.
Recognize Laryngospasm
Laryngospasm can be obvious or subtle, but it always shows signs of airway obstruction. Depending on severity, there may be very little chest or ventilation bag movement with spontaneous ventilation. When laryngospasm is complete, no ventilation is possible. Signs of airway obstruction include rib retraction, tracheal tug, and rocking breathing movements (chest falls and abdomen rises with inspiration). There will be stridor if laryngospasm is partial; however, stridor won’t occur without some air movement.
Break Laryngospasm
Once the reflex is triggered in a semiconscious patient, it often persists for a dangerously long time because the part of the brain that would normally turn it off is “asleep.” Getting the patient out of stage II will break the spasm. This can be done by either deepening the anesthetic (with gas or intravenous agents) or allowing the patient to awaken to the point where the reflex stops itself. However, if the spasm isn’t broken, hypoxia will develop quickly and can lead to cardiac arrest. Waiting out the spasm usually isn’t an option.
To break laryngospasm, first stop stimulating the vocal cords. Suction the airway. Sometimes simply removing the object that touched the vocal cords or the secretions is enough to break the spasm.
Alert your colleagues and ask for help. Never treat laryngospasm alone. Direct all efforts to delivering oxygen. Apply your ventilation mask tightly against the face, and provide a continuous positive pressure breath with your ventilation bag while performing a jaw thrust. The jaw thrust is important. Thrusting the jaw forward:
- lifts the epiglottis and tongue off the glottic opening;
- rocks the larynx forward, counteracting some of the tension bunching the vocal cords together;
- pulls the aryepiglottic folds connecting the sides of the epiglottis to the back of the arytenoids, opening a small gap between the vocal cords; and
- stimulates the patient because it’s painful, perhaps waking the patient out of stage II toward consciousness.
All of these actions are directed at creating a gap between the vocal cords. Once you have that gap, then a positive pressure breath forces oxygen below the cords, pressurizing the larynx below the cords and forcing the cords further apart, usually breaking the spasm.
The time from onset of laryngospasm to hypoxia to bradycardia to cardiac arrest can be a matter of minutes, especially in small children. If laryngospasm is not breaking quickly with positive pressure alone, do not delay further treatment. A small dose of a sedative drug, such as propofol, may be needed. This deepens the level of anesthesia and usually stops the spasm.
If sedation doesn’t break it, then give a small dose (0.25-0.5 mg/kg IV) of a short-acting muscle relaxant, such as succinylcholine, to restore your ability to ventilate. If you don’t have IV access, then give this as an intramuscular dose (3-4 mg/kg IM). The patient can breathe after this small dose but will be very weak and need ventilatory assistance until it wears off. Just remember, if neostigmine reversal has been given prior to a dose of succinylcholine, that reversal agent will prolong the succinylcholine block, making it long acting.
8. Medication Errors Can Lead to Respiratory Emergencies
Case: I was on a volunteer medical mission to Vietnam in the 1980s. We had just finished a week of cleft lip and palate repairs for 80 children, and all of our equipment was packed and ready to go. A mother brought us a tiny, preterm infant weighing about 2.5 kg with a severe facial cleft that effectively left the baby’s left eye open and exposed. We could not operate on the little one, but our surgeon wished to sew the eyelid closed to protect the eye.
To be safe with this obviously high-risk patient, I told the surgeon he would have to manage without anesthesia. He agreed and said he would put a drop of local anesthesia in the eye to anesthetize the eye itself. A drop of topical lidocaine sounded reasonable, so I said yes. The surgeon then surprised me by squirting 2 mL of 4% lidocaine onto the eye. I don’t know how much of that 80 mg of lidocaine got absorbed systemically, but the previously crying baby immediately went limp and unresponsive. Fortunately she was still breathing.
The surgeon was extremely pleased that he now had an unmoving target. I, on the other hand, was terrified. The local hospital did not have an ETT, laryngoscope or mask small enough for this infant immediately available, and all of my airway equipment was in a packing crate. Failure to communicate clearly, and be specific about drug dose, had placed this baby at risk for apnea and potential seizures. I anxiously watched this baby breathe for the next two hours until she woke and began to nurse.
The literature states that 5% to 27% of all pediatric medication orders contain errors, a very sobering number.29-31 Considering that many of these errors occur in the smallest, and therefore most vulnerable, of our little patients, the potential impact is especially great.
Young children require weight-based dosing. Small doses in small volumes can be hard to administer, especially in an emergency. Not only do children require small doses, their immature nervous systems place them at high risk for drug overdose. Unforced errors like the one I witnessed can quickly lead to respiratory depression and apnea, as well as cardiac arrest.
How Do You Prevent Drug Error?
- Know the correct pediatric milligram per kilogram dose—if you don’t know, look it up. Be sure to be safe.
- Units count; never give an order without units. It’s especially important to make the distinction between milligram, microgram and milliliter because making a mistake often changes the child’s dose significantly.
- Broselow Tape can be misleading. The tape gives the dosage of medications for each size child in milligrams. The problem is that we administer liquid medications in milliliters. Changing from milliliter to milligram requires math, and whenever math is involved, errors follow.
- Check your math with someone else, especially for medications you rarely give, or with tiny doses.
- When using an electronic pediatric drug calculator, make sure the concentration of the drug you are using is the same one the app is using.
- Draw up the correct dose. Always check your concentration before drawing up the medication.
- Dose low and go slow. Respiratory depression can lead to cardiac arrest.
- Label syringes with diluted drugs completely.
9. GlideScope Technique Must Take Pediatric Anatomy Into Account
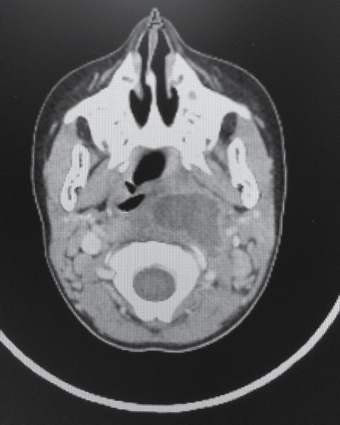
Case: I was anesthetizing a 5-year-old, 15-kg girl for CT-guided drainage of a retropharyngeal pharyngeal abscess (Figure 22). She had mild stridor and preferred to sit rather than lie flat, but otherwise appeared relaxed and comfortable. I planned to electively use a pediatric GlideScope (Verathon). I also had one of my colleagues with me in case of difficulty with mask ventilation. The difficult airway cart was available.
Although she had a preinduction IV placed, I planned an inhalational mask induction to allow her to continue to breathe spontaneously. I was concerned that manual ventilation might be difficult. I had propofol, atropine and succinylcholine drawn up and ready.
Her mother was present in the scanner room and held her hand while she went to sleep. I sent the mom to the waiting area as soon as the girl’s eyes closed. Because she was at high risk for laryngospasm, I waited at least five full minutes until end-tidal sevoflurane showed a deep level of anesthesia. I then visualized using the GlideScope GVL video laryngoscope 2.5, as per weight recommendations. I was not able to obtain a good view of the larynx. I switched to a GVL 2, the next smaller size, and immediately had a good view of the larynx. Intubation was easy and the case proceeded without difficulty.
Just as in adults, video laryngoscopes like the GVL can help in a difficult airway situation. Four sizes of pediatric GVL are currently available, and pediatric-sized blades are usually chosen by patient weight:
- GVL 0 for less than 1.5 kg;
- GVL 1 for 1.5-3.6 kg;
- GVL 2 for 4-20 kg; and
- GVL 2.5 for 10-28 kg.
Be aware that the shape of the pediatric GlideScope blade varies significantly with the size to accommodate the differences in airway anatomy (Figure 23). This may mean that selecting the next size smaller than recommended for that weight child may provide a better view. It allows more ability to manipulate the angle and depth of the blade in the small pediatric mouth.33,34 As you can see in the bullets above, there is some overlap in weight-based blade selection. You should optimally have both sizes available and be ready to switch blades if the first one doesn’t give good visualization.
The stylet should match the curve on the GlideScope blade. For children older than about 4 years, it’s often better to use a stiffer wire stylet rather than the highly flexible slip guide type, because the latter is often not long enough or stiff enough to guide an ETT larger than size 5.
Practice with the different shape pediatric GlideScope blades, or any other emergency rescue equipment, during routine intubations before you need them.
10. Recognize Limits Regarding the Difficult Pediatric Airway
Case: An ED physician from a small, non-pediatric hospital shared this case with me. The child was an 18-month-old girl whose older brother had been playing with laundry detergent pods. He had offered a pod to her, who promptly put it in her mouth and chewed it, releasing the liquid. Her mother had brought her to the ED with respiratory distress late at night. The child had severe stridor, with 40 breaths per minute. Oxygen saturation was 92%. She was awake and alert but anxious.
The ED doctor recognized significant airway obstruction and was concerned that the obstruction could worsen if the edema got worse. She immediately called for an anesthesiologist and a head and neck surgeon to come to the ED to evaluate the child. While waiting, she gave 10 mg of intramuscular dexamethasone (Decadron) and treated the child with nebulized racemic epinephrine. She attached a pulse oximeter, left the child sitting on her mother’s lap and otherwise did not disturb the child, trying to avoid making her cry. By the time the anesthesiologist and surgeon arrived, the stridor, although still present, sounded better.
The question was what to do next.
The head and neck surgeon was able to use his fiberscope to take a quick look at the child’s upper airway. Although the epiglottis and pharynx were swollen, he was able to see that the vocal cords themselves appeared normal, implying that the burn from the detergent was oropharyngeal and most likely not tracheal. This was an important distinction because a tracheal burn from aspirating the detergent might cause progressive lower airway edema and loss of the airway. Since this appeared to be oropharyngeal, they felt justified in initially treating this medically, without intubation, especially since racemic epinephrine had improved the stridor.
Transport to a larger pediatric hospital would have taken hours, and they were concerned that the child could decompensate on the way. Instead, they observed the child closely all night in the ED. The anesthesiologist had an OR prepared for a pediatric airway emergency, and the head and neck surgeon remained quickly available. Two additional doses of racemic epinephrine were given over the next few hours when stridor returned.
By the next morning, the stridor had resolved. After more hours of observation, the child was discharged.
In this case, the team—one that infrequently managed children—prepared for the worst, but treated the child conservatively rather than risk doing more harm.
What Constitutes a Difficult Airway?
Multiple studies have shown that laryngospasm, failure to ventilate and failure to intubate have been the leading causes of respiratory events resulting in cardiac arrest in healthy children.1,35
It’s easy to see that managing a pediatric airway is more challenging than in the adult in the best of times. When complicated by infection, foreign body aspiration or congenital deformity, the situation becomes more intense. Even the experienced intubator will be tested in these circumstances. A full discussion of the management of the difficult pediatric airway is beyond the scope of this article. However, you must be able to recognize a difficult airway when you see one. Signs of a difficult airway include:
- Edema or bleeding in and around the oropharynx
- Congenital facial anomalies such as facial asymmetry
- Chin that is short or hypoplastic
- Limited opening of the mouth
- Limited range of motion of the neck
- Prominent overbite
- Very large tongue (macroglossia)
- Poor visibility of uvula
- Extreme obesity (often with a short neck and significant double chin)
- History of sleep apnea
- Larynx fixed to the midline by a tumor or scar
- Neck mass
- Vocal cord abnormalities
- Mucopolysaccharidoses
Who Is the Right Person for the Job?
In your career, you will encounter children with difficult airways, from either acute processes like epiglottitis (Figure 24) or chronic conditions such as congenital anomalies. You must realistically assess whether you have the correct skills and, if not, what you can do to optimize the situation to maximize safety for the child. Ask yourself:
- Can I ventilate this child?
- Could I use a supraglottic airway like an LM airway?
- Will intubation be difficult because of anatomy, swelling or infection?
Only an expert, or a provider working with an expert in airway management, should attempt intubation of a child with significant airway abnormalities unless a life-threatening emergency exists (Figure 25). Seek the advice and assistance of any available experienced intubators. Consider having a surgeon available for surgical airway intervention if loss of the airway is a serious risk. If the expertise to manage a particular child’s airway is not available, and conditions permit, transport the child to a more optimal location.
Caveats If You Must Proceed in the Presence Of Airway Obstruction
Airway obstruction from such common pediatric emergencies as epiglottitis, croup or foreign body aspiration may force you to proceed emergently with airway management.
In the presence of airway edema, you may be able to avoid the need for intubation by treating with steroids, racemic epinephrine and cool humidified oxygen.
In epiglottitis or croup, decompensation usually develops slowly, giving you time to attempt medical management. Obstruction from foreign body aspiration can occur rapidly and unpredictably as the aspirated object is free to move from partial to total obstruction without warning. Airway burns can also progress from minimal to complete obstruction as edema worsens.
Once a diagnosis of airway obstruction is made, regardless of the diagnosis, the child should be accompanied at all times by someone skilled in airway management. Decompensation from fatigue can occur suddenly and without warning.
Keep the parent with the child to avoid crying and agitation, which will worsen swelling and obstruction. Consider transporting both in the same wheelchair or gurney. Provide extra oxygen.
If intubation is required, consider bringing a child with airway compromise to the OR. There, a gentle general anesthetic induction can be performed using spontaneous ventilation in a setting with equipment and personnel to minimize the risk for loss of the airway. Have everything you need to treat loss of the airway, should it occur. Choose a smaller than predicted ETT size. A cuffed tube will provide the most flexibility and minimize the risk for requiring a tube change.
Manually ventilating a child with obstruction is usually possible but may take two people—one holding the mask with both hands and using maximal jaw thrust, and the second squeezing the bag. Make sure to open the airway as much as possible to avoid distending the stomach. Distention will decrease effective TV and increase the risk for vomiting and aspiration.
Don’t forget that supraglottic airways can and should be available as a rescue airway. They may allow for safe transport to a facility where the child’s airway can be more safely managed. However, they will not open the airway if the obstruction is subglottic, as in croup or with a foreign body.
The cricothyroid space is underdeveloped in young children. Percutaneous needle or surgical cricothyrotomies and tracheostomies carry a higher risk for trauma and failure. A rigid bronchoscopy in children younger than 8 years may be preferable.36
Extra Warning: Foreign Body Aspiration
Avoid manual bag-valve ventilation in a child with an aspirated foreign body until after you have attempted removing it. Positive pressure may push it farther down the airway, precipitating complete obstruction. Anesthesiologists typically allow the child to breathe spontaneously until deep enough under inhalational anesthesia to perform laryngoscopy or bronchoscopy to remove the object.
As a last resort, if you have been unable to ventilate the patient, intubation can be used to both establish an airway as well as to push the object farther down the trachea and into a mainstem bronchus. This will allow at least partial ventilation and the foreign body can be removed later by bronchoscopy, once the crisis has passed. The risk is blocking the carina, but if you can’t ventilate at all, it may be a risk worth taking.
If the patient has inhaled soft material like peanut butter or marshmallow, it can plug the ETT. You may need to extubate and reintubate with a new tube if obstruction persists after the intubation.
Pediatric Airway Management Doesn’t End in the OR
You and your anesthesia staff and OR staff may be well prepared to manage a complicated pediatric patient or surgery, but is the rest of your hospital? Care of pediatric patients doesn’t end at the OR door. Nursing staff can monitor, recognize and treat problems early because of familiarity and pattern recognition. If the staff is unfamiliar with the anatomy and physiology of younger patients, or even what constitutes normal vital signs, then the risk for missing early warning signs of trouble is greater. It is necessary to:
- know your nursing staff’s experience;
- know your staff’s comfort level;
- know the availability of emergency pediatric equipment in your hospital; and
- evaluate whether the child needs critical care monitoring, and if so, whether your hospital has an appropriate unit.
Conclusion
If you take the differences in the anatomy and physiology of infants and toddlers into account, you will become confident in your ability to help children breathe and keep them safe.
- The immature nervous system creates risk. Hypoxia causes bradycardia in a child due to increased parasympathetic tone. Avoidance of hypoxia is challenging because the immature brain gets oversedated easily. A young child will not be able to cooperate.
- Pediatric anatomy predisposes to airway obstruction.
- Babies and small children get hypoxic easily due to their immature respiratory system and their inefficient mechanics of breathing.
- Caring for a baby or toddler without correct-sized equipment jeopardizes patient safety.
- The infant and toddler have a more “anterior airway,” mandating modification of intubation technique.
- Successful LM airway use depends on selecting the right size and possibly modifying insertion technique.
- Recognize laryngospasm and always be prepared to manage it.
- Medication errors are common in children.
- Pediatric GlideScope video laryngoscopes have different shapes for children of varying ages, so you must adjust your technique accordingly.
- Be aware of any limitations in yourself, your staff and your hospital regarding care of the difficult pediatric airway.
References
- Morray JP, Geiduschek JM, Caplan RA, et al. A comparison of pediatric and adult anesthesia closed malpractice claims. Anesthesiology. 1993;78(3):461–467.
- Lee C, Mason L. Complications in paediatric anaesthesia. Curr Opin Anaesthesiol. 2006;19(3):262-267.
- Bhananker SM, Ramamoorthy C, Geiduschek JM, et al. Anesthesia-related cardiac arrest in children: update from the Pediatric Perioperative Cardiac Arrest Registry. Anesth Analg. 2007;105(2):344-350.
- Auroy Y, Ecoffey C, Messiah A, et al. Relationship between complications of pediatric anesthesia and volume of pediatric anesthetics. Anesth Analg. 1997;84(1):234-235.
- Keenan RL, Shapiro JH, Kane FR, et al. Bradycardia during anesthesia in infants. An epidemiologic study. Anesthesiology. 1994;80(5):976-982.
- Anders JE, Brown K, Simpson J, et al. Evidence and controversies in pediatric airway management. Clin Pediatr Emerg Med. 2014;15(1):28-37.
- Babl FE, Vinci RJ, Bauchner H, et al. Pediatric pre-hospital advanced life support care in an urban setting. Pediatr Emerg Care. 2001;17(1):5-9.
- Lerner EB, Dayan PS, Brown K, et al. Characteristics of the pediatric patients treated by the Pediatric Emergency Care Applied Research Network’s affiliated EMS agencies. Prehosp Emerg Care. 2014;18(1):52-59.
- Weiss M, Vutskits L, Hansen TG, et al. Safe anesthesia for every tot—the SAFETOTS initiative. Curr Opin Anaesthesiol.2015;28(3):302-307.
- Fiadjoe JE, Nishisaki A, Jagannathan N, et al. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med. 2016;4(1):37-48.
- Zhao J, Gonzalez F, Mu D. Apnea of prematurity: from cause to treatment. Eur J Pediatr. 2011;170(9):1097-1105.
- Cook TM, Wolf AR, Henderson AJ. Changes in blood-gas tensions during apnoeic oxygenation in paediatric patients. Br J Anaesth. 1998;81(3):338-342.
- Whitten CE. Pediatric Airway Management: A Step-by-Step Guide. San Diego, CA: Mooncat Publications; 2018.
- Weisman LE, Merenstein GB, Steenbarger JR. The effect of lumbar puncture position in sick neonates. Am J Dis Child.1983;137(11):1077-1079.
- Gleason CA, Martin RJ, Anderson JV, et al. Optimal position for a spinal tap in preterm infants. Pediatrics. 1983;71(1):31-35.
- Whitten CE. Use of the nasal airway to assist ventilation during fiberoptic intubation. September 16, 2015. https://airwayjedi.com/?2015/?09/?16/?use-of-a-nasal-airway-to-assist-ventilation-during-fiberoptic-intubation. Accessed March 14, 2019.
- Crelin ES. Development of the upper respiratory system. Clin Symp. 1976;28(3):1-30.
- Thorsteinsson A, Larsson A, Jonmarker C, et al. Pressure- volume relations of the respiratory system in healthy children. Am J Respir Crit Care Med. 1994;150(2):421-430.
- Morris MG. Comprehensive integrated spirometry using raised volume passive and forced expirations and multiple-breath nitrogen washout in infants. Respir Physiol Neurobiol. 2010;170(2):123-140.
- Whitten CE. Pediatric airway risks: inefficient mechanics of breathing. February 25, 2019. https://airwayjedi.com/?2019/?02/?25/?pediatric-airway-risks-inefficient-mechanics-of-breathing. Accessed February 25, 2019.
- Abramson Z, Susarla S, Troulis M, et al. Age-related changes of the upper airway assessed by 3-dimensional computed tomography. J Craniofac Surg. 2009;20 Suppl 1:657-663.
- Peterson J, Johnson N, Deakins K, et al. Accuracy of the 7-8-9 rule for endotracheal tube placement in the neonate. J Perinatol. 2006;26(6):333-336.
- Zahoor A, Ahmad N, Sereche G, et al. A novel method for laryngeal mask airway size selection in paediatric patients. Eur J Anaesthesiol. 2012;29(8):386-390.
- Nakayama S, Osaka Y, Yamashita M. The rotational technique with a partially inflated laryngeal mask airway improves the ease of insertion in children. Paediatr Anaesth. 2002;12(5):416-419.
- Ghai B, Makkar JK, Bhardwaj N, et al. Laryngeal mask airway insertion in children: comparison between rotational, lateral and standard technique. Paediatr Anaesth. 2008;18(4):308-312.
- Olsson GL, Hallen B. Laryngospasm during anaesthesia. A computer-aided incidence study in 136,929 patients. Acta Anaesthesiol Scand. 1984;28(5):567-575.
- Whitten CE. Anyone Can Intubate: A Step-by-Step Guide to Intubation and Airway Management. 5th ed. San Diego, CA: Mooncat Publications; 2012.
- Flick RP, Wilder RT, Pieper SF, et al. Risk factors for laryngospasm in children during general anesthesia. Paediatr Anaesth. 2008;18(4):289-296.
- Cimino MA, Kirschbaum MS, Brodsky L, et al; Child Health Accountability Initiative. Assessing medication prescribing errors in pediatric intensive care units. Pediatr Crit Care Med. 2004;5(2):124-132.
- Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114-2120.
- Marino BL, Reinhardt K, Eichelberger WJ, et al. Prevalence of errors in a pediatric hospital medication system: implications for error proofing. Outcomes Manag Nurs Pract. 2000;4(3):129-135.
- Heinrich S, Birkholz T, Ihmsen H, et al. Incidence and predictors of difficult laryngoscopy in 11,219 pediatric anesthesia procedures. Paediatr Anaesth. 2012;22(8):729-736.
- Lee JH, Park YH, Byon HJ, et al. A comparative trial of the GlideScope video laryngoscope to direct laryngoscope in children with difficult direct laryngoscopy and an evaluation of the effect of blade size. Anesth Analg. 2013;17(1):176-181.
- Armstrong J, John J, Karsli C. A comparison between the GlideScope video laryngoscope and direct laryngoscope in paediatric patients with difficult airways—a pilot study. Anaesthesia. 2010;65(4):353-357.
- Braz LG, Braz JR, Modolo NS, et al. Perioperative cardiac arrest and its mortality in children. A 9-year survey in a Brazilian tertiary teaching hospital. Paediatr Anaesth. 2006;16(8):860-866.
- Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management—part 1—difficult tracheal intubation encountered in an unconscious/induced patient. Can J Anaesth. 2013;60(11):1089-1118.

















Leave a Reply
You must be logged in to post a comment.