Author: Michael Vlessides
Anesthesiology News
A successful outpatient total joint arthroplasty program with minimal readmissions is feasible in carefully selected patients, according to a team of researchers.
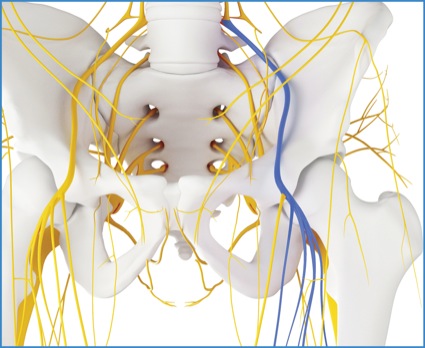
As explained by Andre P. Boezaart, MD, PhD, a professor of anesthesiology and orthopedic surgery at the University of Florida, in Gainesville, the linchpin in the program’s success is a viable continuous femoral nerve block, which enables early mobility and early discharge, safeguards against patients being readmitted for pain-related complications, and offers marked opioid sparing with increased patient satisfaction.
“The biggest thing we noticed was that we didn’t have any readmissions for pain,” he said. “But we also saw that a very large percentage of our patients never even filled their postoperative opiate prescriptions, presumably because we sent them home with these continuous femoral nerve catheters.”
Given these anecdotal observations, the investigators sought to more systematically assess the efficacy of the continuous blocks as a central part of the institution’s outpatient total joint arthroplasty (TJA) program. Their motivation was tangible: By some estimates, as much as half of all such surgeries will be performed on an outpatient basis in the next 10 years.
The investigators reviewed a consecutive series of the first 105 individuals to go through their outpatient TJA protocol. Each participant was discharged with a continuous femoral nerve block comprising 0.2% ropivacaine infused at 3mL per hour with a disposable pump as the central component of postoperative analgesia. All patients also received concomitant multimodal pain management consisting of acetaminophen, nonsteroidal anti-inflammatory drugs and tramadol as necessary.
Dr. Boezaart and his colleagues investigated a variety of end points, most notably same-day discharge rate and the reasons for same-day discharge failures. They paid particular attention to pain and block-related failures, as well as rates of complications and readmission. These metrics were then compared with the records of 390 matched inpatients undergoing TJA during the same period.
Complications Fall Among Outpatients
As Dr. Boezaart reported at the 2019 annual meeting of the American Academy of Pain Medicine (abstract 214), 79% of patients (83/105) were successfully discharged home after surgery.
The most common reasons for admission after having been unable to discharge on the same day were: orthostatic hypotension, patient’s own decision or insistence, urinary retention, nausea and leg buckling. Significant leg buckling and pain occurred in fewer than 3% of patients in the study group.
Not surprisingly, mean hospital length of stay was shorter among outpatients (0.24 days) than matched inpatients (1.53 days; P<0.01). The outpatients also proved superior on mean readmission rate: 0.95% versus 3.70% (P=0.18).
Interestingly, the rate of complications also was lower in the outpatient group (1.9%) than among inpatients (2.90%; P=0.61). No outpatients were readmitted for pain management.
Stimulating Catheters Improves Success
Yet as Dr. Boezaart discussed, the program’s viability is inextricably linked to the anesthesiologists’ ability to place a viable continuous femoral nerve block. “Unfortunately, that’s where a lot of folks fall flat,” he said in an interview with Anesthesiology News.
The way he sees it, the success of this block can be maximized by using stimulating catheters, which he said are superior to ultrasound in these situations.
“When ultrasound first came out, everyone thought it could be used to successfully place continuous catheters,” Dr. Boezaart said. “Of course that’s true, but you must be in the correct compartment around the nerve, and you can’t see the membrane—specifically the circumneurium, to which the catheter has to be positioned—with ultrasound.
“So, you might have a great block on the first day because the high concentration and volume of local anesthetic allows the drug to diffuse through the relevant membranes,” he said. “But on the second day, when we use a low concentration for the continuous infusion, the local anesthetic gets taken up by the blood before it can diffuse through these membranes. So to be truly successful, you have to physically put the catheter between the circumneurium and epineurium membranes in the most optimal perineural adipocyte-containing space.” The chances of successful catheter placement, he asserted, can be maximized by using stimulating catheters.
Given that he invented stimulating catheters, Dr. Boezaart admitted the potential for a conflict of interest. “What most people don’t realize is that I get royalties from Teleflex for both stimulating and nonstimulating catheters,” he reported. “So for me, there’s no financial incentive to use one or the other.
“It’s a patient care issue, and to prevent secondary block failure, based on our 27-year experience and at least 50,000 catheter placements, you have to stimulate the catheter,” he said.
Nevertheless, he acknowledged that the continuous block demands a certain level of technical expertise, which ultimately led to the development of raeducation.com, a website dedicated to enhancing all aspects of regional anesthesia training.
“Are these continuous catheters a bit more demanding to place from a technical standpoint? Yes, they are. But I feel it’s just something you have to learn,” Dr. Bozeaart said.
“Our readmission rate for pain after total joint arthroplasties has been zero; our secondary block failure doesn’t exist; and opioid prescriptions decreased by up to 56%,” he added. “And it’s all based on our technique, which works.”
Confirmatory Data Needed
Jeffrey C. Gadsden, MD, an associate professor of anesthesiology and the chief of orthopedic, plastic and regional anesthesiology at Duke University Medical Center, in Durham, N.C., agreed that the success of an outpatient joint program rests mainly on the ability to provide reliable, long-lasting, block-based analgesia. “Catheters are an excellent way to do this, and the authors have shown that with the right expertise and infrastructure, we can achieve very good outcomes with minimal side effects,” said Dr. Gadsden, who is also a member of the editorial advisory board of Anesthesiology News.
“Many anesthesiologists prefer motor-sparing adductor canal blocks for total knee replacements, but we tend to forget that these blocks are also sensory-sparing,” Dr. Gadsden said. “In contrast, the authors’ use of a low-rate femoral nerve infusion appears to provide high-quality pain control with minimal motor block. Having said that, I would like to see more data from their institution on rehab measures and ambulation to satisfy the concern about safety with ambulatory femoral catheters.”
Dr. Gadsden agreed that secondary failure is a concern, and stimulating catheters may be one way to verify catheter tip location. “However,” he added, “we know that evoked motor response by stimulation is insensitive; the tip can be inside the nerve and fail to generate a twitch. In our practice, verification of correct local anesthetic spread through the catheter using ultrasound leads to very low failure rates.”


Leave a Reply
You must be logged in to post a comment.