Anesthesiology News
Director, Anesthesia for Otolaryngology
Department of Anesthesiology
Yale School of Medicine
New Haven, Connecticut
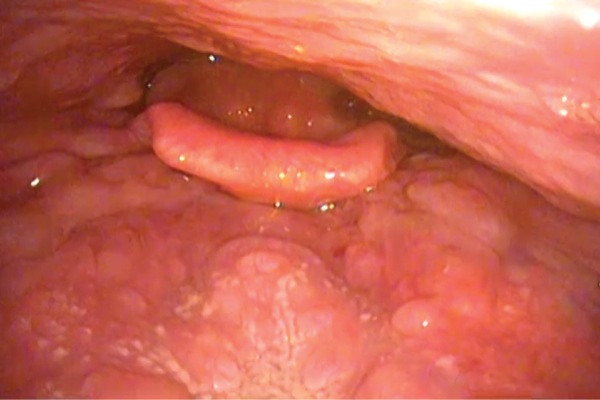
The rapid adoption of video laryngoscopy (VL) has, as the LMA (Teleflex) did in the 1990s, revolutionized the care of patients with routine and difficult airways. Along with careful premanagement evaluation, the routine use of VL promises to all but eradicate the phenomenon of the unanticipated difficult airway. Although there may be rare, undetected pathology of the airway, the majority of “cannot intubate” cases were shown by Ovassapian et al to result from lingual tonsil hyperplasia (LTH), that is, hyperplastic lymphoid tissue at the base of the tongue (Figure 1; video available at bit.ly/2JyUaRZ).1
VL, by virtue of placement of the imaging element at or distal to the anatomic location of LTH, renders impotent this most common cause of unanticipated difficult laryngoscopy. Unfortunately, as was shown in the Fourth National Audit Project (NAP4) of the Royal College of Anaesthetists and the Difficult Airway Society, poor or omitted airway evaluations and negligence to act on abnormal preoperative findings continue to result in failed airway management, but there is debate as to whether these occurrences should be labeled as “unanticipated.”2
Although the unanticipated difficult airway has been eliminated in theory, situations remain where airway pathology or iatrogenic airway changes (as the result of surgery, therapeutic radiation, etc) still present critical challenges to the airway manager.
Traditionally, these tumors or distortions of the airway were managed with techniques of awake intubation. Generally, after an exam, the decision whether to employ awake airway management should include the following criteria:
- the patient who is at risk for failed rapid intubation and alveolar oxygenation (by face mask or supraglottic airway);
- the patient who is at risk for failed rapid intubation and aspiration of gastric contents; and
- the patient who is at risk for failed intubation and will not tolerate apnea.
This last condition emphasizes the idea that no outcome is certain, and when any particular patient is at risk for precipitously suffering harm when an error in judgment has been made, caution remains the better part of valor.3
Law et al and Thomas et al studied the tenacity of the technique of awake intubation in the era of VL.4,5 In their study, Law et al found that the incidence of awake intubation remained constant at 1.06% of 146,252 surgical cases collected over a 12-year period. In the same epoch, this group increasingly embraced routine VL. Despite the progressive adoption of VL, the rate of awake intubation was stable. Thomas et al saw a similarly persistent rate of awake intubation over a 3-year period. In the authors’ opinion, what did not persist were the false-positive decisions leading to awake intubation; that is, fewer airways were perceived to be at risk as the appreciation for the above-mentioned criteria was refined.
Awake intubation is commonly associated with the use of a flexible intubation scope (FIS). Although often referred to as “fiberscopes,” the technology of modern devices has advanced from the 10 to 30,000 coherent bundle-glass fiber instruments in use in the 1960s to 1990s to an image-capturing charge-coupled device and complementary metal-oxide semiconductor technology embedded in the objective end of the FIS. However, the controlled trial literature, case reports, and online media demonstrated that the colloquialism of “awake fiber-optic” intubation should be abandoned. The decision to maintain a patient spontaneously breathing and cooperative (ie, aware, if not awake) should be separated from the device employed to deliver a tracheal tube.
Certainly this is not a new concept. Awake intubation by direct laryngoscopy has long been described, and retrograde wire-aided intubation remains a viable alternative technique in an awake or asleep patient.
However, the literature has been brimming with reports describing the use of VL in awake patients.6-12 Portability and familiarity—for those who often use VL in their routine practice—make awake VL an attractive alternative to FIS-aided awake intubation. As discussed above, because LTH is the most common cause of unanticipated difficult intubation, a patient previously identified as having this variant, and meeting other criteria for awake intubation, would ideally be served with VL. Of note, patients with even severe LTH typically maintain a sagittal plane airway; access to their airway from the lips to larynx can be described in a single curved plane (Figure 2A). This “axis” is required for the use of rigid devices such as the available video laryngoscopes. A more complex airway, where multiple axes must be negotiated (Figure 2B), are not as amenable to a rigid device and account for the continued need for flexible, steerable devices.
Figure 2.
Familiarity with the technique of VL-aided awake intubation can yield advantages: i, a flexible laryngoscope might not be available because of other clinical demands or damage.6 ii, Video laryngoscopes have become ubiquitous in anesthetic practice and therefore not only offer an available alternative, but one that the operator may be familiar with using in the anesthetized patient.iii, Compared with standard VL, many clinicians consider flexible endoscopy to be a demanding technique requiring skills difficult to maintain in routine practice. iv, Because of the dependent movement of blood or secretions in the airway, a likewise posterior-positioned objective of the FIS may be contaminated. v, Tracheal tube selection is less limited when standard VL is used; minimal tube size is not limited by the outer diameter of the FIS. vi, Video laryngoscopes do not include a working channel that can harbor biofilm that is difficult to remove. vii, Hang-up—where the size discrepancy between the FIS insertion cord and tracheal tube may result in tissue entrapment, tissue damage and failure to pass the tracheal tube into the larynx—is not a concern when using a video laryngoscope. viii, Lastly, expert use of an FISdemands a skilled and practiced operator, especially in the awake patient.
The first reported case of VL use for awake intubation was by Doyle in 2004.6 Because a fiber-optic bronchoscope was not available, a reusable GlideScope (Verathon) was employed for awake intubation in 2 patients. After demonstrating the feasibility of the technique, 2 additional awake intubations were electively accomplished with a GlideScope.
Subsequent to Doyle’s letter, several authors, in both controlled and uncontrolled reports, have described VL in awake intubation, compared VL with FIS in awake intubation, and compared various video laryngoscopes in awake intubation. The Table shows a nonexhaustive list of these reports. In all reports, use of VL in the awake patient has been found equivalent, or in some ways superior, to FIS. Common variables measured were first-attempt success, time to intubation, best glottic view, ease of use, and patient satisfaction.
| Table. Reports of Video Laryngoscopy for Awake Intubation | |||||
| Year | Citation | Device(s) | Report Type | Cases, N | Patient Conditions |
|---|---|---|---|---|---|
| 2004 | Doyle6 | GlideScope (Verathon) | Letter | 4 cases | Obesity, trismus |
| 2009 | Dimitriou et al7 | Airtraq (Prodol Meditec) | Case report series | 4 cases | Ankylosing spondylitis, trismus-high Mallampati score, trismusa |
| 2012 | Rosenstock et al8 | FIS vs McGrath MAC (Aircraft Medical) | RCT | 93 patients | Anticipated difficult airways |
| 2015 | Drenguis and Carlson9 | GlideScope vs C-MAC (KARL STORZ Endoscopy) | RCT | 26 views of the glottis | Normal airways, sitting “face to face” |
| 2016 | Mahran and Hassan10 | GlideScope vs FIS | RCT | 54 patients | Nasal intubation, oropharyngeal cancer |
| 2016 | Nassar et al11 | GlideScope vs Bonfils Retromolar (KARL STORZ Endoscopy) | RCT | 60 patients | Morbid obesity |
| 2016 | Mendonca et al12 | Pentax Airway Scope | RCT | 40 patients | Clinically evaluated risk for difficult intubation |
|
aTwo cases of urgent surgery in patients with significant trismus.
FIS, flexible intubation scope; RCT, randomized controlled trial
|
|||||
Preparation of the patient for an awake intubation with a video laryngoscope follows the tenets of awake intubation with an FIS or any other device13:
- The rationale for awake intubation and the procedure are explained to the patient.
- The airway is dried with an IV or intramuscular desiccant, suction, and/or gauze sponging.
- Topical and/or atomized local anesthetic is applied, or invasive local anesthetic blocks are performed.
- Modest, if any, sedation is administered, with the goal of keeping the patient cooperative with procedures.
- All steps are taken in a nonrushed manner.
One distinct difference between topical local anesthetic techniques for VL and FIS is the lack of a working channel in the former, ubiquitous in all but the smallest FIS. The application of local anesthetic below the vocal folds may therefore, but not always, demand a change in technique: use of a spray atomizer, such as a MADgic Laryngo-Tracheal Mucosal Atomization Device (Teleflex); trans-cricothyroid membrane injection or nebulized local anesthetic; and other techniques. (A video of a typical awake intubation technique is available at bit.ly/2sLCuMB.)
A limitation of the use of VL in the patient with a difficult airway is access to the oral cavity. Absolute trismus will be an absolute contraindication for VL in the awake or anesthetized patient. In Doyle’s first description, a patient with an interincisor gap of 2.5 cm was successfully intubated with a GlideScope. The present author has successfully used a video laryngoscope in an awake patient with an interincisor gap of 1.25 cm (video available at bit.ly/2KjOekh). Trismus by itself is not an indication for awake intubation. The patient should have another factor influencing the decision not to induce anesthesia (eg, in the author’s case, severe gastroesophageal reflux).
Another limitation of VL is the nonsagittal plane airway, meaning that a mass or some other distortion (eg, trauma, prior airway surgery) has resulted in non–straight line access from the oral aperture to the glottis (Figure 2B). Typically, the FIS is the ideal tool for navigating these “multiaxis” airways, but this is not to say that a video laryngoscope does not have a role. VL may be a superior technique for anterior tissue (eg, tongue, epiglottis, anterior mass) displacement when the FIS is used (see video available at Bit.ly/2mGjewp).
This “combined technique” has been described in several reports and may offer an alternative to tongue retraction or an intubating oral airway.14 Not only may the anterior forces applied with VL create an imaging space in front of the objective, but it also allows for guidance of the FIS through a complex airway.
In the technique, the patient is prepared for awake intubation following the clinician’s preferred routine, as discussed above. The patient is asked to open the mouth and extend the tongue. It may be helpful for the VL operator to hold the tongue extended using a gauze pad. The video laryngoscope is then gently inserted over the superior surface of the tongue, with care being taken not to contact the posterior pharyngeal wall, which may elicit a gag reflex. If a gag is elicited at any point, further topical anesthetic should be applied with an atomizer or other technique in a spray-as-you-go fashion.
If the larynx can be visualized, local anesthetic can be administered and/or the tracheal tube may be inserted as appropriate. If a pathway to the larynx is not evident, the FIS, controlled by a second operator, is inserted via the lumen created by the VL effort. If the laryngeal inlet is not apparent via the FIS, its advancement can be guided via the image produced by the video laryngoscope. As noted above, one disadvantage of the combined VL/FIS technique is the need for a second operator to perform the VL.
In summary, the use of VL for awake intubation is a viable and practical alternative to awake FIS intubation. For many practitioners, VL has become a familiar if not routine technique. Whereas basic skills with the flexible scope are difficult to maintain, VL skills may be reinforced daily.
Despite this, I believe that flexible scope skills cannot be completely abandoned. Complex airways without sagittal plane access to the larynx will often require a device that can operate along multiple planes. The good news is that such a complex airway should never be encountered unexpectedly. When a patient has been thoroughly evaluated in the preoperative clinic or holding area and there are no or only minor concerns for tracheal tube placement, the only problem that might arise, except in rare occasions, is the presence of LTH. As discussed above, VL renders this phenomenon unimportant from an airway management perspective. In fact, it is likely that when using VL routinely, patients with LTH will be encountered without the laryngoscopist’s knowledge.
References
- Ovassapian A, Glassenberg R, Randel GI, et al. The unexpected difficult airway and lingual tonsil hyperplasia: a case series and a review of the literature. Anesthesiology. 2002;97(1):124-132.
- Cook TM, Woodall N, Frerk C, et al. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011;106(5):617-631.
- Rosenblatt WH. The Airway Approach Algorithm: a decision tree for organizing preoperative airway information. J Clin Anesth. 2004;16(4):312-316.
- Law JA, Morris IR, Brousseau PA, et al. The incidence, success rate, and complications of awake tracheal intubation in 1,554 patients over 12 years: an historical cohort study. Can J Anaesth. 2015;62(7):736-744.
- Thomas G, Kelly F, Cook T. No reduction in fibreoptic intubation rates with universal video laryngoscopy. Can J Anaesth. 2016;63(1):113.
- Doyle DJ. Awake intubation using the GlideScope video laryngoscope: initial experience in four cases. Can J Anaesth. 2004;51(5):520-521.
- Dimitriou VK, Zogogiannis ID, Liotiri DG. Awake tracheal intubation using the Airtraq laryngoscope: a case series. Acta Anaesthesiol Scand. 2009;53(7):964-967.
- Rosenstock CV, Thøgersen B, Afshari A, et al. Awake fiberoptic or awake video laryngoscopic tracheal intubation in patients with anticipated difficult airway management: a randomized clinical trial. Anesthesiology. 2012;116(6):1210-1216.
- Drenguis AS, Carlson JN. GlideScope vs. C-MAC for awake upright laryngoscopy. J Emerg Med. 2015;49(3):361-368.
- Mahran EA, Hassan ME. Comparative randomised study of GlideScope video laryngoscope versus flexible fibre-opticbronchoscope for awake nasal intubation of oropharyngeal cancer patients with anticipated difficult intubation. Indian J Anaesth. 2016;60(12):936-938.
- Nassar M, Zanaty OM, Ibrahim M. Bonfils fiberscope vs GlideScope for awake intubation in morbidly obese patients with expected difficult airways. J Clin Anesth. 2016;32:101-105.
- Mendonca C, Mesbah A, Velayudhan A, et al. A randomized clinical trial comparing the flexible fibrescope and the Pentax Airway Scope (AWS) for awake oral tracheal intubation. Anaesthesia. 2016;71(8):908-914.
- Rosenblatt WH, et al. Airway management. In: Barash PG, Cullen BF, Stoelting RK, et al, eds. Clinical Anesthesia. 8th ed. Philadelphia, PA: Wolters Kluwer; 2017.
- Lenhardt R, Burkhart MT, Brock GN, et al. Is video laryngoscope-assisted flexible tracheoscope intubation feasible for patients with predicted difficult airway? A prospective, randomized clinical trial. Anesth Analg. 2014;118(6):1259-1265.




Leave a Reply
You must be logged in to post a comment.