Director, Anesthesia for Bronchoscopic Surgery
Director, Center for Sedation
Departments of General Anesthesiology and Outcomes Research
Cleveland Clinic
President, Society for Head and Neck Anesthesia
President-elect, Society for Ambulatory Anesthesia
Airway management has always been and continues to be of extreme interest to anesthesiologists. It requires cognitive and technical skills that are essential to safe patient care. Difficult airway is a term that historically has been used loosely to describe any challenge anticipated and/or encountered in the process of airway management. However, more recently, greater effort has been directed at better defining the challenge of the difficult airway with the aim of better studying it—its predictors, causes, and pathophysiology. By studying the difficult airway, we can identify ways to address airway challenges, improve the safety of airway management, and minimize related morbidity and mortality.
- Difficult face mask ventilation
- Difficult laryngeal mask ventilation
- Difficult laryngoscopy
- Difficult intubation
- Difficult surgical airway
However, anesthesiologists also commonly describe other airway-related challenges as being components of a difficult airway; examples are a patient with a subglottic stenosis or one with an anterior mediastinal mass. By doing this, anesthesiologists unintentionally dilute the terminology and create a set of generalized reactions, expectations, and preparations—some of which may be necessary and needed versus others that may be inappropriate, redundant, or merely wasteful—and at the same time miss out on an opportunity to be prepared for the real challenge at hand.
It is important to differentiate the true difficult airway (ie, the upper airway), which includes challenges encountered in managing the upper airway from induction of anesthesia to successful intubation of the trachea, and which encompasses the aforementioned 5 categories.
Contrast that with the difficult lower airway, which includes issues encountered from the level of the vocal cords to the very distal portions of the tracheobronchial tree.2
A difficult upper airway should not mean a difficult lower airway, and vice versa; for example, a patient with a large anterior mediastinal mass (a difficult lower airway) can be easy to intubate (an easy upper airway), but difficulty might be encountered in achieving adequate or even any ventilation despite proper positioning of an endotracheal tube (ETT).
Nonetheless, the 2 entities can occur simultaneously in the same patient, such as one who has an anterior mediastinal mass or an obstructive endobronchial tumor (a lower airway challenge) who is known to have a difficult upper airway due to anatomic derangements: an overbite, a small mouth opening, a short thyromental distance, and a large tongue. Another example is a patient who has a very large goiter extending retrosternally, causing distortion and compression of the larynx (difficult upper airway), as well as the upper trachea (a challenging lower airway).3
The difficult upper airway is discussed frequently in different ways and formats, but little attention is given to the challenge of the lower airway (Table).5 I hope this review will increase awareness of this concept and help us consider airway management more carefully, creating better plans.
| Table. Examples of Lower Airway Challengesa | |
| Category | Example |
|---|---|
| Subglottic stenosis | Idiopathic or due to granulomatosis with polyangiitis |
| Tracheostomy and Montgomery T-tube management | Urgent or emergent versus elective tracheostomy. Tracheostomy or T-tube replacement, up- or downsizing, and decannulation |
| Endoluminal, extraluminal, or mixed central airway obstruction | Bronchogenic carcinoma, goiter, mediastinal mass, etc |
| Tracheal disruption | Traumatic tear or tumor-related |
| Bronchial disruption | Dehiscence of lung transplant anastomosis |
| Tracheal resection surgeries | Certain types and degrees of tracheal stenosis or tumor invasion |
| Tracheoesophageal fistula | Esophageal or bronchogenic cancer complications versus traumatic fistula |
| Bronchopleural fistula | Post-thoracic surgery |
| Less common conditions | Tracheomalacia, tracheal reconstruction after an airway fire |
| a Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2018. All rights reserved. | |
Case Presentation
A 25-year-old man presented with symptoms consistent with stridor and shortness of breath, and was found to have granulomatosis with polyangiitis (formerly known as Wegener’s granulomatosis) and subglottic/upper tracheal stenosis with kidney sparing. He was scheduled for tracheal dilation (cuts, electrocautery, balloon dilation, and laser therapy if needed).
If the patient presents with stridor signifying more than 50% stenosis of the airway and increased work of breathing is noted, especially in urgent or emergent situations, the use of Heliox (a mixture of 70% oxygen and 30% helium) has been found to alleviate the stridor, decrease the work of breathing, and improve ventilation and oxygenation. Heliox is effective because of its low density compared to the higher fraction of inspired oxygen (FiO2) or air, thus decreasing the turbulent flow.
Tracheal stenosis patients without a history of or potential for a difficult airway can be anesthetized safely with an IV induction agent followed by a muscle relaxant, as face mask ventilation has not been found to be generally problematic in these patients, even in severe cases.6 Another technique that has been described and performed successfully is an inhalation induction. Sevoflurane is the volatile agent of choice for a mask inhalation induction because of its bronchodilating characteristics and lack of pungency

Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2018. All rights reserved.
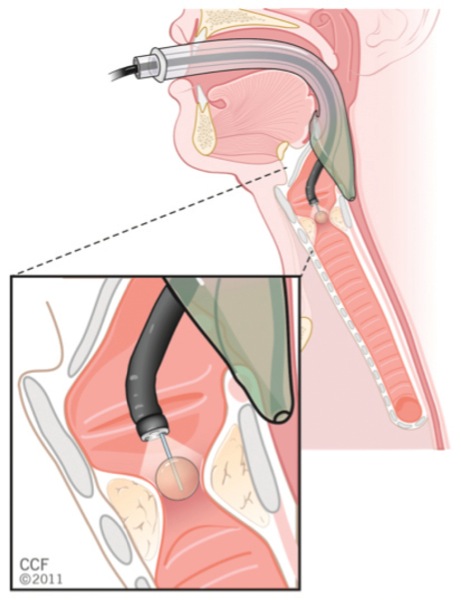
Treatment modalities and airway management will differ, depending on the exact location of the stenosis. Immediate subglottic stenosis lesions are treated by an ear, nose, and throat surgeon, using a suspension laryngoscopy technique and supraglottic jet ventilation, which can be either proximal jetting, in which the jetting needle is attached to the eye or proximal orifice of the suspension laryngoscope, or distal jetting, in which the jetting needle is attached to a side port running alongside the suspension laryngoscope to open at the level of the vocal cord (Figures 1A and B).7 This is differentiated from subglottic jetting, which often is used for managing vocal cord lesions using specialized tubes, such as a Hunsaker catheter (Figures 2A and B).
When jet ventilation is applied in this way (proximal and distal supraglottic jetting), the risk for airway fire from electrocautery or laser therapy is low because of the lack of a fuel (combustible material), despite the presence of an oxidizer and an energy source (in this case high oxygen concentration and electrocautery or laser, respectively). The lesion is generally treated with cuts by scissors, electrocautery, or laser therapy, followed by balloon dilation. In some instances, steroid injection is utilized with or without mitomycin application. The patient is then allowed to wake up from anesthesia after reversal of muscle relaxation and withdrawal of the suspension laryngoscope, and the airway is maintained with face mask ventilation, a supraglottic airway, or a small-diameter ETT. If the lesion is at a level lower than the immediate subglottic area, it is generally managed by thoracic surgeons or interventional pulmonologists, who intervene as described above albeit with instruments introduced through the operating channel of a flexible operating bronchoscope that is inserted through a supraglottic airway (for proximal tracheal lesions; Figure 3), a large-diameter ETT, or a rigid bronchoscope (for distal tracheal lesions).
If the patient had a history of a documented difficult airway, an appropriate approach would be awake intubation using a small microlaryngeal tube (MLT). After inducing general anesthesia and muscle relaxation, the MLT is then removed following establishment of an airway with suspension laryngoscopy or rigid bronchoscopy.
Ventilation through a rigid bronchoscope can be accomplished by jet ventilation through a special attachment to the side port; however, this is my least favorite technique because it is cumbersome, carries the risks associated with jet ventilation, and the FiO2 cannot be controlled unless a special and expensive automated jet ventilator is used, which adds another piece of equipment to the already limited space around the patient.
A simpler technique is to attach the anesthesia machine breathing circuit to the side port of the rigid bronchoscope, for which rubber caps are needed to seal its various openings and wet gauze is packed around it in the oropharynx to facilitate manual positive pressure ventilation (Figure 4). This is my preferred method, due to its immediate availability, simplicity, safety, low cost, and the fact that the FiO2 can be controlled easily.

When jet ventilation is used and/or the nature of the procedure results in circuit leaks, as is the case with rigid bronchoscopy or flexible bronchoscopic procedures, a total IV anesthesia (TIVA) technique—an infusion of propofol—is preferred to an inhalational anesthetic technique. Compared with an inhalational anesthetic technique, TIVA ensures continuous delivery of the anesthetic and prevents operating room pollution by inhalational anesthetic.
Inhalational anesthetics may have some advantages in certain situations, however. We previously described our anesthetic technique for the management of very large mediastinal masses,8 when inhalational anesthetics are used to augment the amnestic properties of dexmedetomidine while still maintaining spontaneous ventilation. Moreover, inhalational anesthetics’ potent bronchodilating effect can be helpful in overcoming the severe bronchospasm often encountered during thermoplasty for endobronchial treatment of severe bronchial asthma.9
When TIVA is used, the continuous flow of the anesthetic through the IV line should be monitored throughout the procedure. In addition, the use of a depth of hypnosis/anesthesia monitor (eg, the bispectral index monitor [BIS Monitor, Medtronic]) can help to gauge the depth of anesthesia and possibly avoid intraoperative recall.10
It should be noted that during any upper or lower airway surgery, it is very important to suction all airway debris and bleeding before clot formation, as organized clots may impair oxygenation and ventilation substantially (Figure 5). If a clot has formed already, suction may not be effective in clearing the airway, and the use of a forceps will be necessary to remove such clots.
Tracheal Tear
A tracheal tear is an uncommon complication of treating tracheal stenosis. The management of a tracheal tear can be observational (conservative) or surgical, depending on the extent of the injury, presenting signs and symptoms, and the general condition of the patient. Generally, small, shallow tears that do not lead to severe compromise in ventilation and oxygenation can be treated conservatively.11,12 If the patient is dependent on positive pressure ventilation, surgical treatment is indicated.
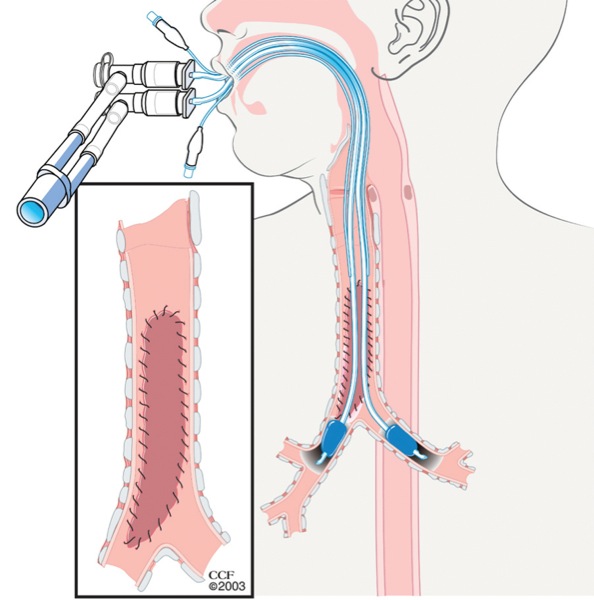
Ventilatory management consists of attempting to achieve adequate oxygenation and ventilation of the patient and prevention of development and/or worsening of subcutaneous emphysema, pneumomediastinum, or pneumothorax. This is best accomplished by positioning the ETT/tracheostomy tube with the cuff distal to the level of injury, and by close monitoring of the airway pressure, keeping it at the lowest possible pressure. Higher FiO2 and respiratory rates may be required. Selective or bilateral bronchial intubation can be performed in tears located near or above the carina (Figure 6). It is important to note that standard direct intubation can be potentially hazardous because a false passage can be easily created, widening the already existing tear and losing the ability to ventilate; flexible bronchoscope-guided intubation is safer.
Other reported options for ventilation and oxygenation in a tracheal tear include high-frequency jet ventilation and hyperbaric oxygen therapy in patients who are difficult to oxygenate or ventilate.13,14 In addition, cardiopulmonary bypass or percutaneous cardiopulmonary support systems have been used in the past in certain circumstances.15,16
Tracheal Resection
In the patient with tracheal stenosis described above, when a small segment of the trachea is resected in certain recurrent tracheal stenosis lesions, the airway management plan should proceed in phases, as follows17:

- Oral intubation: An MLT is positioned with the cuff distal to the lesion (Figure 7A).
- After accessing the trachea from the surgical field, the MLT is withdrawn to a level above the tracheal incision and its tip is sutured. The end of the thread is marked and attached to the drapes to facilitate repositioning toward the end of surgery, and a trans-field wire- reinforced ETT is introduced into the distal trachea to facilitate ventilation while the tracheal resection and posterior re-anastomosis are accomplished (Figure 7B).
- The trans-field ETT is removed and the oral MLT is reintroduced into the trachea under direct vision, which is facilitated by the suture placed earlier to the tip of the MLT to ventilate while the anterior re-anastomosis and wound closure are accomplished (Figure 7C).
- The patient is awakened, and every effort should be made to avoid coughing or straining. Next, the patient is extubated and admitted to the ICU for overnight monitoring and observation.
Conclusion
Lower airway challenges can present on their own or coexist with difficult upper airways. A clear understanding of the differences between the 2 conditions and excellent communications between the anesthesiology, surgical, critical care, emergency department and nursing teams are extremely valuable for developing and executing an effective and safe management plan.
References
- Brovocanin Z, Shapiro J. Introducing the difficult airway. In: Doyle DJ, Abdelmalak B, eds. Clinical Airway Management: An Illustrated Case-Based Approach. London, England: Cambridge University Press; 2017:7-12.
- Abdelmalak B, Sethi S, Gildea TR. Anesthesia and upper and lower airway management for advanced diagnostic and therapeutic bronchoscopy. Adv Anesth. 2014;32(1):71-87.
- Abdelmalak B, Makary L, Hoban J, et al. Dexmedetomidine as sole sedative for awake intubation in management of the critical airway. J Clin Anesth. 2007;19(5):370-373.
- Balan S, Abdelmalak B. Tracheal rupture. In: Doyle DJ, Abdelmalak B, eds. Clinical Airway Management: An Illustrated Case-Based Approach. London, England: Cambridge University Press; 2017:261-264.
- Doyle DJ, Abdelmalak B, eds. Clinical Airway Management: An Illustrated Case-Based Approach. London, England: Cambridge University Press; 2017.
- Doyle DJ, George J III. Anesthesia for management of subglottic stenosis and tracheal resection. In: Doyle DJ, Abdelmalak B, eds. Anesthesia for Otolaryngologic Surgery. London, England: Cambridge University Press; 2012:263-270.
- Abdelmalak B. Jet ventilation: principles and practice. In: Woodworth G, ed. Anesthesia Education Toolbox. 2017. toolboxlms.collectedmed.com. Accessed June 20, 2018.
- Abdelmalak B, Marcanthony N, Abdelmalak J, et al. Dexmedetomidine for anesthetic management of anterior mediastinal mass. J Anesth. 2010;24(4):607-610.
- Abdelmalak B, Gildea T, Doyle DJ. Anesthesia for bronchoscopy. Curr Pharm Des. 2012;18(38):6314-6324.
- Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness and the bispectral index. N Engl J Med. 2008;358(11):1097-1108.
- Zettl R, Waydhas C, Biberthaler P, et al. Nonsurgical treatment of a severe tracheal rupture after endotracheal intubation. Crit Care Med. 1999;27(3):661-663.
- Marquette CH, Bocquillon N, Roumilhac D, et al. Conservative treatment of tracheal rupture. J Thorac Cardiovasc Surg. 1999;117(2):399-401.
- Lin JC, Maley RH Jr, Landreneau RJ. Extensive posterior-lateral tracheal laceration complicating percutaneous dilational tracheostomy. Ann Thorac Surg. 2000;70(4):1194-1196.
- Ratzenhofer-Komenda B, Offner A, Kaltenbock F, et al. Differential lung ventilation and emergency hyperbaric oxygenation for repair of a tracheal tear. Can J Anaesth. 2000;47(2):169-175.
- Yamazaki M, Sasaki R, Masuda A, et al. Anesthetic management of complete tracheal disruption using percutaneous cardiopulmonary support system. Anesth Analg. 1998;86(5):998-1000.
- Hirsh J, Gollin G, Seashore J, et al. Mediastinal “tamponade” of a tracheal rupture in which partial cardiopulmonary bypass was required for surgical repair. J Cardiothorac Vasc Anesth. 1994;8(6):682-684.
- George J III, Lorenz R, Abdelmalak B. Airway management for tracheal resection surgery. In: Doyle DJ, Abdelmalak B, eds. Clinical Airway Management: An Illustrated Case-Based Approach. London, England: Cambridge University Press; 2017:190-





Leave a Reply
You must be logged in to post a comment.