Author: Michael Vlessides
Anesthesiology News
Sometimes budgetary pressure is a good thing.
So say clinicians and administrators at Thomas Jefferson University Hospital who, faced with constraints that threatened to shut down a preanesthesia testing center (PAT), instead redesigned patient and work flows throughout the center with a renewed focus on efficiency, cost containment, best practices and the patient experience. The results for the Philadelphia hospital were significant reductions in expense on salary and overtime, as well as a decrease in the average hospital length of stay.
“As is the case in many large hospitals, Jefferson was under budgetary constraints, with a focus on defining value and looking for revenue-earning opportunities in every department and expense category,” said David F. Nelson, MD, MBA, who was a fellow in perioperative management when the study was conducted. “A traditional preoperative testing center, which has all the bricks and mortar and staffing involved in an expensive downtown location, received attention as a place that had no direct revenue-earning opportunity but nevertheless represented a sizable cost.
“So the mandate to perioperative leadership was figure out a way to either drastically reduce cost or set up the PAT for downstream revenue-earning opportunities in the future,” said Dr. Nelson, now an assistant professor of anesthesiology at Thomas Jefferson University. “Knowing that the PAT provides value for day-of-surgery preparation, it was seen as a salvage technique to avoid closure of the center completely.”
Faced with this grim reality, the clinicians began the redesign by gathering data on almost every aspect of the center’s performance, including expenses and performance metrics. Key stakeholders from a variety of departments were invited to help reimagine the entire presurgical experience, only this time from the patient’s perspective. Three primary outcomes were identified: budgetary compliance, patient experience and seamless integration with the institution’s newly acquired electronic health record system.
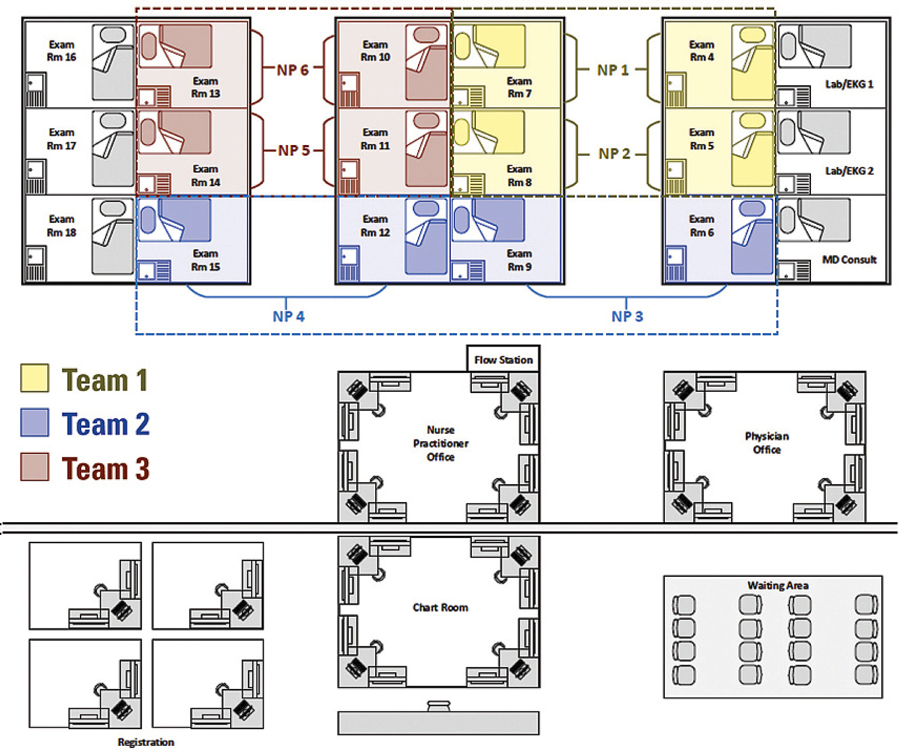
By September 2017, the institution began the first phase of the redesign, which involved restructured roles and responsibilities for PAT staff of registered nurses, nurse practitioners, medical assistants and registration officers (Figure 1). “Under the previous iteration, patients came in during an approximate appointment time zone and were seen by the next available staff member, in a rolling fashion,” Dr. Nelson said. “This didn’t work too well because there wasn’t a standard pathway for a visit.”
Rethinking Everything, From Arrival to Checkout
By comparison, the new design focused on assigning tasks that allowed each staff member to practice within the full scope of their license. This saw nonclinical assistants (and not nurses) focusing their energies on tasks such as patient scheduling and registration responsibilities, enabling nurses to make more screening calls. Medical assistants were charged with obtaining patient vitals, allowing nurse practitioners to perform patient histories and physical examinations.
“We also really structured the flow of patients so that the patient visit and flow were both more standardized,” Dr. Nelson said (Figure 2). This included predetermined scheduling times, standardized visit workflows, and built-in appointment slots for walk-in patients. “This helped create certain time expectations, so that clinicians would know exactly how much time they had with each patient.”
Reporting at the 2018 Perioperative Leadership Summit of the Association of Anesthesia Clinical Directors, Dr. Nelson said preliminary financial analysis of PAT salary and overtime expenses indicated a net reduction of $157,478 over a six-month period, representing a 22.4% decrease relative to the same interval in the previous year. Much of this decrease, he added, was due to a reduction in variable overtime expense as well as the elimination of one full-time employee from the workforce. Patients’ total visit times from arrival to checkout also fell, from an average of 134±27 to 102±11 minutes over the two time periods, which is a 23.9% decrease.
Although Dr. Nelson was quick to note that many of the implemented changes were commonsense, the nature of health care occasionally prevents clinicians from seeing their role in the broader continuum. “Many times in health care, we clinicians exist in silos, and sometimes there are opportunities for improvement that we miss.”
However, change doesn’t always come easily, as Dr. Nelson and his co-investigator Rebecca A. Barnett, MBChB, can attest. “I think one of the biggest challenges is asking professionals to redefine their roles and look at their job in a different way,” he said. “That’s hard in any sector, not just medicine.”
Even with their success, the researchers are looking at more ways to improve the PAT process for patients, clinicians and administrators alike. “The next phase is looking for revenue-earning opportunities and setting up a consult system with subspecialists, so that patients who are expected to be followed postoperatively can have their initial encounter in the PAT,” Dr. Nelson explained. “And even if they’re not seen by the specialist preoperatively, the point is to better integrate consistency, which is really one of the aims of quality.
“There’s nothing too groundbreaking or exciting about process maps or flows, but applying them to this setting is one way to show they can have a profound effect in a health care setting, especially on the downstream financials.”
According to Paul St. Jacques, MD, the president of the Association of Anesthesia Clinical Directors in Columbus, Ohio, the study by Drs. Nelson and Barnett is timely and important. “Their work takes the perioperative clinic to a new level by incorporating aspects of an improved patient experience, incorporation of evidence-based clinical pathways and full integration with hospital systems,” he commented. “They accomplish this while also addressing a significant barrier to preoperative assessment by reducing staffing costs.
“Given the national need to improve both the financial performance and outcomes related to surgical care,” Dr. St. Jacques said, “institutions should look to this model when considering redesign of the preoperative assessment process.”



Leave a Reply
You must be logged in to post a comment.