Author Thomas C. Mort, MD
Anesthesiology News
Emergent tracheal intubation outside the operating room (OR) is challenging in terms of complications and patient safety concerns. The acute and critical nature of the patient’s need for airway control escalates the dangers with both recognized and unrecognized difficult airway situations. Presuming a higher level of difficulty may benefit both the airway team and the patient by promoting a more cautious approach to induction method, equipment choices, and rescue planning. Optimizing initial attempts may reduce complications and patient injury, and ultimately lower total attempts and various equipment interventions.
The proliferation and availability of video-assisted laryngoscopy (VAL) may further hamper our specialty’s interest in maintaining adequate skills with an FFB.5 A limited availability of case reports and small studies purporting potential application of “awake VAL” to the difficult airway patient suggests a growing interest in this approach.6-9 This review determines the feasibility of whether VAL can be successfully deployed to assist with the management of the non-OR patient population requiring emergent tracheal intubation.
Patient preparation using the topical local anesthesia (TLA) approach can vary by the practitioner’s comfort, judgment, and experience; the patient’s airway status; the acute clinical condition(s) prompting the airway intervention; and the patient’s neurologic/mental status. Three common categories of patients receive TLA during emergency intubation in this anesthesia practice: the known/anticipated difficult airway patient, the patient in hemodynamic extremis (preexisting hypotension, shock, inadequate resuscitation, or significant cardiopulmonary compromise), and those with significantly depressed mental status who do not require IV medications to optimize intubation conditions. The large number of anesthesia attending staff who supervised the “stat” airway team provided a nonrandomized database of critically ill patients who were deemed appropriate for emergency tracheal intubation under TLA preparation combined with the “awake/aware” condition. However, many patients had depression of their mental status due to their underlying pathology or pharmacologic interventions prior to the airway team’s arrival.
Cases that involved concurrent sedative-hypnotic/anxiolytic agents with TLA were arbitrarily categorized by medication dosing on a weight basis to delineate “mild” from “moderate-heavy” dosing regimens. Midazolam at 0.04 mg/kg or less (eg, 1-3 mg), etomidate at 0.1 mg/kg or less (eg, 4-8 mg), and propofol at 1.0 mg/kg or less (eg, 20-70 mg) were chosen arbitrarily to represent “light” preparation as opposed to more generous dosing of induction agents commonly administered to render the patient tolerant of the airway intervention. Patients receiving neuromuscular blocking agents were excluded. Demographic data were evaluated in an attempt to discern which difficult airway characteristics were present that prompted the use of VAL.
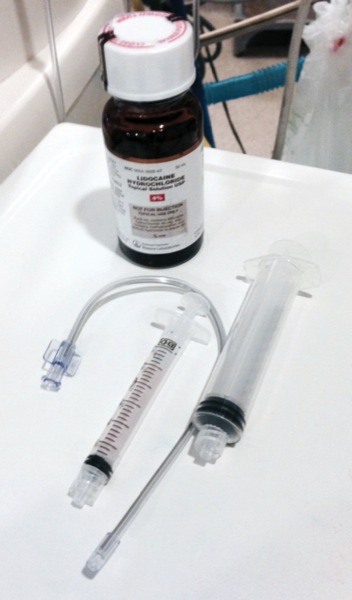
Topical application of 4% lidocaine was applied to the patient’s oral cavity and oro-hypopharynx by either a syringe or an atomizer (MADgic Laryngo-Tracheal Mucosal Atomization Device [Teleflex]; Figure 1). Particular areas of interest for coverage were the posterior tongue, tonsillar pillars, and the supraglottic areas. If the patient’s mental status allowed, they were requested to gargle as long as possible and then swallow the TLA liquid. A “cough” was anticipated as the TLA was sprayed and gargled. This suggested aspiration of the liquid and potential periglottic-tracheal coverage. Fewer than 5% were topicalized using a laryngo-tracheal analgesia device containing 4% lidocaine (4 mL). Additionally, lidocaine jelly/ointment was applied to the tongue with a tongue depressor or via the laryngoscope blade. The adequacy of topical anesthesia coverage was commonly determined with either a tongue depressor or the laryngoscope blade prior to formal laryngoscopy (Table 1).
| Table 1. Topical Local Anesthesia Tips |
| Optimize positioning |
| Suction airway prior to application of TLA |
| Anticipate “pooling” of the TLA once the patient is anesthesized, but don’t “prematurely” suction |
| Rigid suction catheter (>35∞) allows improved secretion removal with extreme curve of VAL |
| “Test” tongue with VAL blade ± TLA jelly/ointment |
| “Dry mucosa need to be moist, wet mucosa needs to be suctioned” |
| If mental status allows discussion, encourage patient participation |
| Time the ETT insertion with vocal cord abduction |
| Encourage a “deep breath” to open glottis, if applicable |
| Additional TLA during VAL was possible using the atomizer (supraglottic, trans-glottic, tracheal) |
| ETT, endotracheal tube; TLA, topical local anesthesia; VAL, video-assisted laryngoscopy |
The GlideScope blade (without the video baton inserted) served as an excellent “tester” of the patient’s ability to tolerate laryngoscopy. Once placed into the mouth and advanced past the curvature of the tongue, if tolerated, the video baton can be placed easily into the plastic blade to view the airway. TLA rarely consumed more than 1 to 4 minutes of preparation time. Local anesthesia nerve blocks were not used in the emergency setting. However, transcricoid membrane puncture was performed to instill tracheal lidocaine in 5 patients by the author.
Patient positioning was a key component of patient preparation. Ramping and head/torso elevation were pursued for obese patients and those with cardiopulmonary decompensation who were intolerant of the supine position (Table 1). Anesthesia personnel were positioned at the head of the bed for nearly all procedures. To compensate for head of bed elevation and upright positioning, the airway team personnel employed footstools or stood on the bed frame. Four cases involved airway personnel performing laryngoscopy (dual management) from the side of the bed coupled with intubation attempted by a second colleague from the opposite side of the bed (cardiopulmonary extremis: eg, severe chronic obstructive pulmonary disease or cardiac tamponade, where the patient benefited from the upright position). Patients laden with secretions were best served by aggressive suctioning prior to TLA application (Table 1). Administration of a “drying agent,” such as glycopyrrolate, was rarely used due to the acute nature of the intubation process.
Once applied, TLA required only 1 to 3 minutes before its numbing effect was achieved. One should resist suctioning out the airway post-TLA prematurely. However, suctioning out the airway just before insertion of the GlideScope was very helpful. The standard-angle Yankauer suction tip may not satisfy suctioning needs with the acutely angulated 65- to 70-degree GlideScope blade positioned in the hypopharynx. If this is your only available suction catheter, suctioning the oropharynx prior to blade placement may be more effective, although it is “blind.” Other rigid suction catheters with a more favorable angle are commercially available (Table 1).
Administration of “mild” IV induction agents was at the discretion of the attending anesthesia staff. This approach was used in 28.3% of the TLA cases (187/660). An important component of prompting acceptance of this technique by the patient was to provide an explanation to the patient outlining the importance of TLA as it relates to the patient’s airway status. Reassurance and gentle reinforcement of the need for the patient’s cooperation were provided, where applicable. This technique is inappropriate in agitated, belligerent, confused, or aggressive patients unless they are controlled by pharmacologic means or redirection by staff. On the other hand, the mental status and interactive capabilities were reduced in many patients due to their clinical condition prompting intubation, hypercarbia, or prior administration of sedative-analgesics prior to the airway team’s arrival.
Many of the critically ill patients were known or presumed to have a difficult airway based on physical examination at the bedside or from previous documentation in the electronic health record. Table 2 outlines the various characteristics that were documented. Elevated Mallampati scores and a preponderance of restricted or no cervical neck range of motion were noted. Based on the body mass index, over half of the encounters were with obese/morbidly obese patients. Other important difficult airway characteristics, such as trismus and head/neck pathology resulting in mass effect/swelling/edema, also contributed to airway management challenges. One-fifth of the total patients managed with VAL-TLA had baseline hypotension (systolic pressure <90 mm Hg) despite ongoing fluid resuscitation and administration of a vasopressor agent by the primary ICU team.
| Table 2. Difficult Airway Characteristics (n=660) | ||
| Characteristics | Measurement | Number (%) |
|---|---|---|
| Mallampati score Total | 3 | 184 (27.9) |
| 4 | 360 (54.5) | |
| 3 and 4 | 544 (82.4) | |
| CROM Total | 1=restricted | 351 (53.2) |
| 0=none (eg, collar, pathology) | 224 (33.9) | |
| 575 (87.1) | ||
| Head/neck infection/mass/edema | 55 (8.3) | |
| Trismus | <2 fingerbreadths opening | 39 (5.9) |
| BMI, kg/m2 | Obese (35-40) | 85 (12.9) |
| Morbid obesity (>40) | 265 (40.2) | |
| Thyromental distance, cm | <4 | 74 (11.2) |
| BMI, body mass index; CROM, cervical range of motion | ||
Each airway encounter took place in any non-OR locale where the stat airway team responded via pager and/or overhead announcement (Table 3). Hemodynamic demographics were varied and reflected the common instability witnessed by the responding airway team to the bedside in emergency non-OR intubation encounters. One-fourth of the patients undergoing VAL-TLA were hypotensive on arrival at the bedside, with many on vasoactive agents before the start of the airway intervention. Due to the pre-existing hemodynamic instability, underlying comorbidities, and the primary acute pathologic condition prompting tracheal intubation (Table 4), the decision by the airway team was to minimize or avoid induction agents that could further compromise the tenuous state of the patient’s hemodynamic status.
| Table 3. Location of Airway Intervention (n=660) | |
| Location | n (%) |
|---|---|
| Medical ICU | 194 (29.4) |
| Surgical ICU | 134 (20.3) |
| Neuro ICU | 101 (15.3) |
| Radiology/cardiac cath lab/GI suite | 89 (13.5) |
| Floor | 72 (10.9) |
| Coronary ICU | 59 (8.9) |
| ED | 11 (1.7) |
| ED, emergency department; GI, gastrointestinal | |
| Table 4. Primary Pathology Precipitating Tracheal Intubation (n=660) | |
| Primary Pathology | n (%) |
|---|---|
| Pneumonia/aspiration | 185 (28) |
| Respiratory failure/COPD/asthma | 160 (24.3) |
| CHF/cardiac deteriorationa | 159 (24.1) |
| CVA/ICB | 88 (13.3) |
| Airway protection/metabolic/alcohol withdrawal | 47 (7.1) |
| Upper gastrointestinal bleed | 21 (3.2) |
| 70.8% of patients were intubated for respiratory insufficiency related to COPD, pneumonia, aspiration, hypoxemia, CHF or asthma.
a Severe cardiopulmonary conditions, including pulmonary embolism and cardiac tamponade, were less common but may have benefited by maintaining spontaneous ventilation and minimizing potential hemodynamic swings with induction (n=13). The remaining cases were based on the need for airway protection due to altered mental status, metabolic derangements, alcohol withdrawal, upper gastrointestinal bleeding, stroke, or intracerebral pathology.
CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; ICB,intra-cerebral bleed
|
|
A total of 660 patients met the criteria for VAL-TLA. The majority of patients received TLA only (n=473; 71.7%), and the remainder received TLA plus limited dosing of sedative-hypnotic/amnestic agents. VAL was used electively in 73.9% (n=488) or as a rescue in 26.1% following difficulty with conventional direct laryngoscopy (DL), with or without bougie assistance, or other airway adjunct (SAD after DL difficulty or a flexible fiber-optic bronchoscopy, FFB). The airway procedure was performed by the anesthesia attending staff alone (n=218; 33.0%) or the supervised anesthesia resident trainee (n=442; 67.0%). The number of VAL attempts was limited to 3 or fewer: 79.4%, 1 attempt; 17.2%, 2 attempts; and 3.4%, 3 attempts. Overall, VAL assisted with successful tracheal intubation in 93.5% of all cases attempted, regardless of elective or rescue utilization (Table 5). Intubation was successful with VAL (unassisted) in 89.2% (n=588) of cases (Figures 2 and 3).

| Table 5. Elective Versus Rescue VAL: Success and Rescue Rates | ||||
| Success (Alone), % | Success With FFB or Bougie as Adjunct, % | LM Airway Rescue, n (%) | Surgical Airway, n (%) | |
|---|---|---|---|---|
| Elective (n=488) | 93.2 | 96.6 | 14 (3.0) | 2 (0.4) |
| Rescue (n=172)a | 76.2 | 87.2 | 19 (11) | 2 (1.2) |
| Total VAL (n=660) | 89.2 | 93.5 | 33 (5.0) | 4 (0.6) |
|
a Direct laryngoscopy rescue after VAL attempts was unsuccessful.
FFB, flexible fiber-optic bronchoscope; LM, laryngeal mask; VAL, video-assisted laryngoscopy |
||||
Adjuncts to assist the VAL procedure were noted: VAL plus FFB (2.3%; n=15) and VAL plus bougie (assistance with endotracheal tube [ETT] advancement past the glottis/cricoid ring) in 2.1% (n=14). VAL difficulty or failure requiring an alternative rescue intervention totaled 38 cases (LMA [Teleflex], n=33; DL, n=1; surgical airway=4). This was weighted heavily toward VAL rescue cases compared with elective VAL use as a primary mode of airway management (Table 4). The SAD laryngeal mask airway played a vital role for rescue when VAL proved difficult.
The overall complication rate for emergency intubation is considerable, as both hemodynamic perturbations and airway-related events may occur. Moreover, one complication often contributes to one or more additional events (esophageal intubation begets desaturation, then bradycardia, etc). Table 6 presents some of the more common complications seen in this population. Although the incidence of desaturation varies little with VAL-TLA compared with the overall database, this group did consist of some of the more challenging cases related to hemodynamic compromise and difficult airway characteristics.
| Table 6. Comparison of Complications | |||
| Complication | Database (2006-2017) (N=10,379) | All VAL (n=5,656) | VAL With TLA (n=660) |
|---|---|---|---|
| Hypotensive responsea | 26.5% | 23.3% | 12.2%b |
| Tachycardic response | 25.4% | 24.5% | 21.0% |
| Added vasopressor support | 20.1% | 19.1% | 4.5%b |
| Hypertensive response | 19.7% | 20.1% | 17.3% |
| Any desaturation (SpO2 <90%) | 14.4% | 14.3% | 15% |
| Severe hypoxemia (SpO2 <80%) | 7.7% | 8.1% | 8.3% |
| Dysrhythmia (bradycardia, SVT, atrial fibrillation) | 4.6% | 3.7% | 1.9%b |
| Esophageal intubation | 2.5% | 1.5% | 2% |
| Cardiac arrest | 1.45% | 1.0% | — |
| Bradycardic response | 1.3% | 1.3% | — |
| Regurgitation | 0.73% | 0.5% | — |
| Aspiration | 0.24% | 0.1% | -— |
|
a Hypotensive response: systolic blood pressure <90 mm Hg; mean arterial pressure <65 mm Hg. Therefore, 75% of those in the database who experienced postintubation hypotension had vasoactive agents administered to support hemodynamics. Many were provided with IV fluids with a vasoactive agent.10 b P<0.02.
SpO2, peripheral capillary oxygen saturation; SVT, supraventricular tachycardia; TLA, topical local anesthesia; VAL,video-assisted laryngoscopy
|
|||
The overall rate of esophageal intubation was 2.0% (13/660 cases), but the majority of these (8/13) occurred during DL attempts likely prompting VAL deployment as a rescue intervention. Esophageal intubation during elective VAL-TLA use was less common (5/488; 1%). Of note is the fortunate lack of regurgitation and aspiration events when caring for the VAL-TLA group. Moreover, the subdued hypotensive response postintubation (cardiovascular collapse)10 as well as the reduced need for vasopressor support in the VAL-TLA group likely reflect the difference in the hemodynamic response when induction agents are avoided or markedly reduced in conjunction with TLA. The rate of cardiovascular collapse in the entire database reflects published findings and is consistent with standard induction regimens practiced during emergency intubation (Table 6).
The incidence of new-onset dysrhythmia during airway manipulation was statistically reduced (Table 6). The much-feared bradycardic response during airway management and the catastrophic “cardiac arrest” associated with emergent airway interventions were not reported for any cases in the VAL-TLA subgroup.
Conclusion
Emergent airway management outside the OR is a highly stressful clinical situation that remains unpredictable and problematic for patient safety. Preserving spontaneous ventilation and maintaining an awake/aware state in the known or anticipated difficult airway patient may be successfully managed by a variety of airway equipment choices. Bronchoscopic-assisted intubation, however, remains the standard of care. However, FFB availability in the remote location may be limited. Further, our growing dependence on VAL may be leading to a shift away from FFB use with further erosion of our bronchoscopic skills.4,5 Dwindling confidence begets waning FFB use and further deterioration of our once-dependable proficiencies.
This author recommends that practitioners should not relegate the FFB to the museum. As we advance in some respects, we regress in others. Our students will be the recipients of this dwindling interest in maintaining or obtaining FFB competency. Our patients may be the heir to the new VAL era, but FFB and other airway adjuncts remain as valuable supplements to an overall, comprehensive airway management schema. Having said this, substituting VAL in the place of an FFB may be a viable alternative in some clinical airway situations, particularly if patient conditions, practitioner skills, and experience or equipment availability are compounding factors.
Our increasing reliance on advanced technology for airway management has allowed us to enjoy improved patient care and a lower incidence of complications.11-14 However, the airway team must remain vigilant and diverse in their abilities to control and secure the airway inside and outside the OR.4,5 In this data review, the airway team’s VAL utilization enjoyed an outstanding 90%+ success rate. Any method (and team) with a 90%+ success rate must be applauded for outstanding achievement.
However, VAL is not a “stand-alone” difficult airway cart on its own. Nearly 1 in 10 video laryngoscopic interventions required either FFB or bougie assistance (within the ETT, rather than free-hand passing of the bougie through the glottis) or other adjuncts for rescue, namely, the SAD. The airway team must be outfitted with such adjuncts and have them available at the bedside to manage the critical care airway outside the OR.
The feasibility of adapting an alternative approach to FFB during emergent airway care is inviting on the basis of successful deployment of VAL technology in the elective setting.10-13 Applying established airway management principles, for example, awake/TLA, to the anticipated difficult airway patient in a remote location under nonelective conditions using a relatively imprecise, hastened, and crude application of TLA appears achievable. Abridged TLA preparation followed by VAL instrumentation in the hopes of securing the airway without “burning any bridges” appears attainable, practical, and within a comfortable threshold of tolerance on the patient’s part coupled with a relatively high likelihood of success.
Although VAL served admirably as a stand-alone device, combining VAL plus FFB adds a new dimension for glottic visualization and ETT maneuvering. Moreover, the relatively common issue of ETT tip hang-up on the cricoid ring (typically responsive to ETT rotation), or an ETT that cannot be maneuvered through or past the glottic opening, may prove successful by advancement of a lubricated bougie via the ETT in a Seldinger maneuver. TLA may offer an additional advantage to the critically ill, unstable patient—a subdued hemodynamic response to the airway instrumentation. In summary, it would seem that this approach has merit and serves to provide valuable advantages when confronted by difficult airway concerns and/or hemodynamic instability.
References
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251-270.
- Rosenblatt WH. The Airway Approach Algorithm: a decision tree for organizing preoperative airway information. J Clin Anesth. 2004;16(4):312-316.
- Amathieu R, Combes X, Abdi W, et al. An algorithm for difficult airway management, modified for modern optical devices (Airtraq laryngoscope; LMA CTrach™): a 2-year prospective validation in patients for elective abdominal, gynecologic, and thyroid surgery. Anesthesiology. 2011;114(1):25-33.
- Fitzgerald E, Hodzovic I, Smith AF. ‘From darkness into light’: time to make awake intubation with videolaryngoscopy the primary technique for an anticipated difficult airway? Anaesthesia. 2015;70(4):387-339.
- Maslow A, Panaro S. Is airway management better? Anesthesiology. 2017;127(1):200-201.
- Doyle DJ. Awake intubation using the GlideScope video laryngoscope: initial experience in four cases. Can J Anaesth. 2004;51(5):520-521.
- Thong SY, Lim Y. Video and optic laryngoscopy assisted tracheal intubation—the new era. Anaesth Intensive Care. 2009;37(2):219-233.
- Suzuki A, Terao M, Aizawa K, et al. Pentax-AWS airway scope as an alternative for awake flexible fiberoptic intubation of a morbidly obese patient in the semi-sitting position. J Anesth. 2009;23(1):162-163.
- Moore AR, Schricker T, Court O. Awake videolaryngoscopy-assisted tracheal intubation of the morbidly obese. Anaesthesia. 2012;67(3):232-235.
- Perbet S, De Jong A, Delmas J, et al. Incidence of and risk factors for severe cardiovascular collapse after endotracheal intubation in the ICU: a multicenter observational study. Crit Care. 2015;19:257.
- Niforopoulou P, Pantazopoulos I, Demestiha T, et al. Video-laryngoscopes in the adult airway management: a topical review of the literature. Acta Anaesthesiol Scand. 2010;54(9):1050-1061.
- Griesdale DE, Liu D, McKinney J, et al. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anaesth. 2012;59(1):41-52.
- Agro FE, Doyle DJ, Vennari M. Use of GlideScope® in adults: an overview. Minerva Anestesiol. 2015;81(3):342-351.
- Paolini JB, Donati F, Drolet P. Review article: video-laryngoscopy: another tool for difficult intubation or a new paradigm in airway management? Can J Anaesth. 2013;60(2):184-191.



Leave a Reply
You must be logged in to post a comment.